Intentional replantation for a Class 4/Stage C cemental tear: Etiology, choice and outcomes of treatment
Key Clinical Message
Cemental tears, root cracks, and associated periapical-periodontal lesions may occur simultaneously in one tooth, and can be effectively managed by intentional replantation and etiological control. A durable splint, along with occlusal and periodontal monitoring, is required as healing progresses slowly and may be insufficient.
1 INTRODUCTION
The cemental tear (CeT) is defined as a “complete separation along the cementodental border or a partial split within the cemental tissues along an incremental line.”1 Depending on its location, CeT may lead to corresponding destruction and symptoms of periodontal and/or periapical tissues. The manifestations of CeT may include rapid localized attachment loss and deep periodontal pockets,2-4 swelling/sinus formation in the alveolar mucosa/gingival,5-7 purulent discharge1, 5, 6 and tooth mobility.3, 6 Diagnosis of CeT often requires radiographic assessment, with a typical periapical radiograph showing needle-like or flake-like structures that are partially or completely separated from the mesial-distal root surface, accompanied by the corresponding alveolar bone destruction images.8, 9 CeT in the buccal-lingual direction often requires diagnosis in combination with cone-beam computed tomography.9 According to the location and accessibility, CeT can be treated by scaling and root planning, periodontal flap surgery, apical surgery, or intentional replantation (IR).8, 9
Intentional replantation is a procedure that involves extracting a tooth, assessing and managing the root and socket, and placing the tooth back in its original position in the socket.10 IR is typically used in cases where traditional surgical methods, such as periodontal flap surgery and traditional apical surgery, cannot reach the lesion area or are not feasible due to anatomical factors.10 Nagata treated CeT in the maxillary central incisor with IR and observed the patient for 12 months. However, his focus seemed to be on histology.3 This case report presents the application of IR for the treatment of mesial-palatal-distally involved CeT (Class 4/Stage C) in the maxillary right central incisor (tooth #8) and demonstrates the treatment results within 16 months. The etiology of the case, as well as the choice and outcomes of replantation are discussed concurrently.
2 CASE HISTORY/EXAMINATION
A healthy 34-year-old smoking male patient was referred to the Department of Periodontology due to intractable swelling and discharge from tooth #8. The patient reported undergoing root canal treatment initially for discomfort in the tooth, but he experienced no relief afterward. 6 months later, gingival swelling and discharge developed on the palatal aspect. The tooth was retreated 1 year after the first attempt, but no improvement was observed.
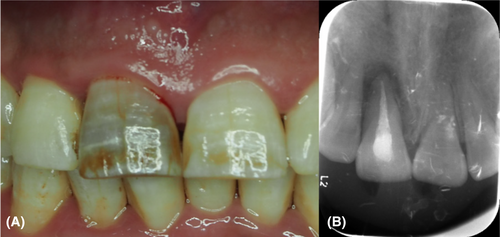
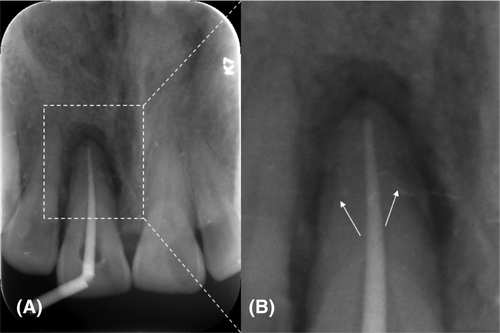
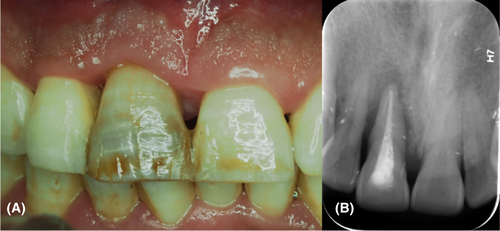
The patient denied any history of dental trauma and hard-object biting, but expressed uncertainty regarding bruxism. However, he admitted experiencing significant work and life-related stress. Examination revealed that multiple teeth, including the affected one, had varying degrees of tooth wear (Figure 1, Figure 2A). Probing depth (PD) at the midpoint of the palatal aspect measured approximately 8 mm (Figure 3, Table 1). Tooth mobility was grade II according to the Miller index (Table 1). Radiographic images displayed flake-like structures detached from the root surface (Figure 4, Figure 2B). A preliminary diagnosis of CeT in the affected tooth was made. Treatment options discussed included exploratory surgery and IR, as well as fixed bridge or implant restoration following extraction. The patient opted to preserve the tooth and underwent IR.


| Time | Subjective symptoms | Periodontal index | ||
|---|---|---|---|---|
| Probing depth (mm) | Gingival recession (mm) | Tooth mobility | ||
| Baseline | Discharge | 8 | 0 | II |
| 9 months | None | 2 | 2 | I |
| 16 months | None | 3 | 2 | / |
- Note: Data of probing depth were measured at the midpoint of the palatal side; the other 5 sites remained normal. Gingival recession represented the average data of proximal surfaces on both labial and palatal sides.
3 METHODS
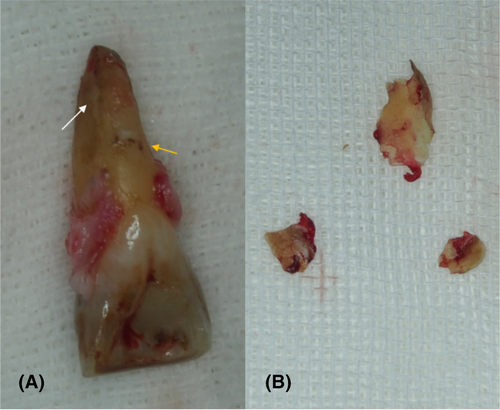
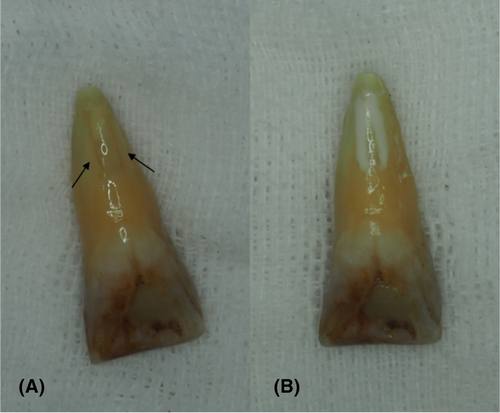
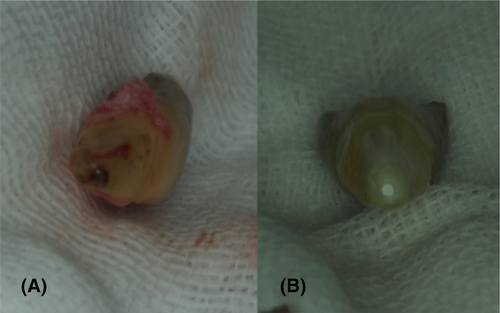
The initial treatment included oral health instruction, psychological counseling, smoking cessation counseling, supragingival scaling and subgingival scaling. During the surgery, a full-thickness mucoperiosteal flap was raised, and the torn fragments were found not fully accessible between the palatal root surface and the alveolar bone. Subsequently, tooth #8 was extracted. The CeT extended from the mid-palatal root to the apex and mesiodistally involved some proximal surfaces. Specifically, the mesial portion of the CeT remained on the root surface (Figure 5A), while the remaining fragments were removed from the alveolar socket (Figure 5B). Following the thorough removal of calculus (Figure 5A) and torn fragments from the root surface, two cracks were observed on the palatal side (Figure 6A) and repaired (Figure 6B). After the apical procedure (Figure 7), the root surface underwent treatment with 12% EDTA (Premier, USA) for 5 min, followed by washing with sterile saline for 1 min. The patient opted against using regenerative materials. Then the tooth was reinserted into the socket and the flaps were sutured. Finally, tooth #8 was stabilized to the adjacent tooth by Superbond (Kyoto, Japan). Additionally, an occlusal adjustment was performed.
The patient was prescribed amoxicillin for 5 days and 0.12% chlorhexidine rinses three times a day for 2 weeks. The sutures were removed 10 days after surgery (Figure 8). He received instructions to refrain from using the affected tooth as much as possible for the next 3–6 months, especially avoiding biting hard objects. Furthermore, he was advised to consult the Department of Prosthodontics for the diagnosis and treatment of the possible parafunctional habits.

4 OUTCOME AND FOLLOW-UP
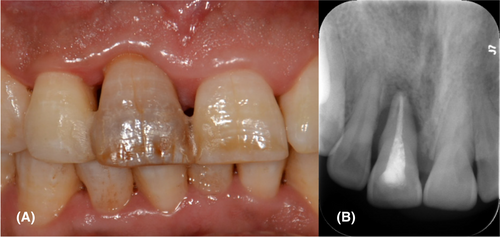
At the 9-month postoperative follow-up visit, the patient stated that symptoms had disappeared since the surgery. Both clinical (Table 1, Figure 9A) and radiographic examinations (Figure 9B) showed significant improvement, while the gingival recession was observed. After the removal of the splint, tooth mobility decreased to grade I. One week later, the patient returned, reporting increased tooth mobility. Examination revealed that tooth #8 exhibited tooth mobility near grade II with normal PDs, prompting refixation. Upon the 16-month postoperative follow-up visit, splinting remained intact, and continued improvement in symptoms, clinical (Table 1, Figure 10A) and radiographic outcomes (Figure 10B) persisted. At this point, a treatment plan involving a fixed prosthesis splint was discussed with the patient. Unfortunately, he was lost to follow-up from that point onward, and subsequent information could not be obtained.
5 DISCUSSION
Cemental tears, root cracks, and associated periapical-periodontal lesions were found simultaneously in the affected tooth. CeT was defined as localized tooth-related factors that modify or predispose to plaque-induced gingival diseases/periodontitis according to the consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions.11 Local mechanical irritation to the surrounding periodontal tissue and alveolar bone caused by torn fragments produces low-grade inflammation.9 Coronal extension of inflammation may form periodontal pockets, which open up pathways for plaque accumulation and retention.9 In this case, the deep isolated periodontal pocket on the palatal side facilitated continuous colonization of intraoral bacteria in the fragments surface, the root surface, and the space between them. Additionally, the root cracks exacerbated the periodontal–pulpal interinfection, imposing a severe inflammatory and infectious burden on the affected tooth.
Cemental tear can be considered a decompensated response when the accumulation of force exceeds the cemento-dentinal junction bearing threshold. Among the previously discovered predisposing factors, increasing age, prior root canal treatment, and systemic diseases6 may increase the likelihood of CeT, by affecting its structural strength. The accumulation of force can result from acute trauma, such as dental trauma7 or biting unexpectedly on a hard object.4 It can also be chronic damage caused by the prolonged accumulation of normal or abnormal forces beyond the fatigue limit, such as increased chewing intensity and frequency,5 clenching2/ bruxism, and other parafunctional habits. Moderate to severe tooth attrition, significantly associated with CeT,12 may also stem from functional contacts or parafunctional habits.13 In this case, multiple teeth with varying degrees of wear were observed, and the attrition of canine, which is rarely used in the functional state, likely results from parafunctional habits. In addition, although it is not clear what the occlusal status of tooth #8 was before CeT, the possibility that the effects of occlusal discrepancies are magnified by increased functional and/or nonfunctional contacts cannot be ruled out. The occurrence of root dentin cracks has also been linked to stress fatigue and root canal treatment.14 In conclusion, the CeT in this case may be a chronic fatigue injury, resulting from one or more factors contributing to an increased occlusal burden on the affected tooth.
The primary concern of treatment is to eliminate the inflammatory and infectious burden. Complete removal of torn fragments is essential for effective management of CeT, with treatment selection based on fragment location and accessibility.8, 9 According to the new three-dimensional classification of CeTs, this case was classified as Class 4 (clinically inaccessible, infrabony defect, apical involvement)/Stage C (cemental tear involves 3 surfaces of the root), and the treatment recommendation is open flap debridement and apicectomy.9 However, studies have been reported that the prognosis of CeT involving the root apex is affected by the difficulty of complete removal of the fragments,5, 6 and CeT located in the apical third of the root had a significantly lower healing rate.15 Nagata et al.3 underwent IR after discovering CeT extending to the palatal side during a periodontal flap surgery. In this case, CeT involved the palatal aspect and the root apex, and the decision of IR was based on anatomical limitations and the partial lesion accessibility. Treatment for unexpectedly discovered root dentin cracks primarily involved crack repair under IR, as reported in limited case reports.14 Tai et al.5 supposed that it was undetectable root cracks that led to the failure of CeT treatment, which was supported in this case. For the space between the root surface and the alveolar bone after the removal of fragments, recent literature suggests a combination of periodontal regenerative procedure.9 However, it has also been suggested that both regenerative and nonregenerative treatment modalities can achieve long-term success, even when the root fragment constitutes a significant portion of the root surface.4 Ultimately, regenerative materials were not utilized due to the patient's refusal.
Another key to treatment is to reduce the occlusal burden on the affected tooth. A periodontal splint and occlusal adjustment are recommended preoperatively for the affected hypermobile tooth demonstrating signs of occlusal trauma.9 In this case, occlusal control was performed in three ways: occlusal adjustment under splinting after replantation to reduce occlusal discrepancies, psychological counseling and suggestions for possible prosthodontics treatment to control potential parafunctional habits, and oral instructions at each visit to manage chewing habits. The patient did not visit a prosthodontic doctor during the observation period.
The operational convenience brought by IR enabled the complete removal of fragments and root infection, which contributed to the disappearance of symptoms, successful soft tissue closure and normal PDs after IR. However, IR also poses a healing challenge. Different healing patterns may occur after IR. Damage to the periodontal ligament may lead to surface resorption or ankylosis/replacement resorption.16 A recent study of 10-year treatment outcomes of autotransplanted teeth has shown that the once considered poor healing outcomes are not significant factors affecting long-term treatment outcomes, and more attention should be paid to periodontal condition and marginal bone loss.17 A replanted tooth with ankylosis can also be retained long-term.18 In this case, there was extensive loss of periodontium within the scope of CeT, but no clinically significant ankylosis was observed. This could be because the ankylosis had not yet occurred or had not involved more than 20% of the root surface.19
The duration of splint application for periapical periodontitis in the literature is advocated within 1 month.20 When there is a lack of initial stability, the splinting duration can be extended to 6 weeks.21 The replantation of periodontally hopeless teeth combined with regenerative procedures take 12–18 months for mobility to return to normal.22, 23 In this case, the mobility decreased to grade I 9 months after surgery, suggesting the healing between the root and alveolar bone had been achieved. While the later increased mobility in functional state indicated that the degree of healing was not enough to independently bear the occlusal load or to deal with occlusal accidents. Imaging results did not show more bone filling 6 months after refixation. In addition to the failure to incorporate regeneration technology, the reduction of the remaining periodontium after extensive CeT, prolonged extracorporeal manipulation due to multiple root anomalies affecting the viability of the remaining periodontium, and the patient's smoking habit24 may influence the healing process and periodontal regenerative capacity, thus affecting the bone fillings. According to Hou et al.,25 significant periodontal regeneration of severe periodontal teeth with vertical bone defects can be achieved after replantation without any regenerative materials on condition of a reliable and durable splint (fixed prosthesis) and a long enough observation time (5–12 years). The longer the distance between the alveolar bone and the root surface, the longer the time for bone healing to reach the root surface.25 Simultaneously, several longitudinal studies have shown that tooth mobility hurts the treatment outcome of periodontal regeneration surgery and maintenance.24, 26 Therefore, long-term splint is needed both to restore normal occlusal function and to maintain the existing healing results and promote the theoretical possibility of more bone filling.
Although the Superbond bonding splint used in this case was not found to be fractured during the observation period, a fixed prosthesis was planned because of its limited strength. The long-term reliability of the splint was questionable, as the control of chewing habit and potential parafunctional habits was unknown after the patient was lost to follow-up.
6 CONCLUSIONS
Intentional replantation provides a better approach for the complete removal of inaccessible torn fragments, as well as the detection and management of other root abnormalities. CeTs, root cracks, and associated periapical–periodontal lesions may occur simultaneously in one tooth, and can be effectively managed by IR and etiological control. Healing after IR progresses slowly and may be insufficient to fully regain occlusal function. Therefore, a long-term and reliable splint is required, along with continuous attention to occlusal control and periodontal maintenance.
AUTHOR CONTRIBUTIONS
Ning Luo: Conceptualization; investigation; project administration; validation; visualization; writing – original draft; writing – review and editing. Xuan Ying: Investigation; project administration; writing – review and editing. Yuxin Tong: Investigation; project administration; writing – review and editing. Yue Chen: Conceptualization; investigation; project administration; resources; supervision; validation; writing – review and editing.
ACKNOWLEDGMENTS
The authors would like to thank Jianglin Zhang and Dan Li for their help during the surgery, as well as Haoyu Wang for his suggestions before treatment.
FUNDING INFORMATION
This project was funded by grants for New Clinical Techniques of Hospital of Stomatology, Xi’an Jiaotong University (xjkqxjs2015-06); Science and Technology Project of Xi’an (2016051SF/YX07), Youth Scientific Research Fund of Hospital of Stomatology, Xi’an Jiaotong University.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




