Laparoscopic resection of a uterine lipoleiomyoma
Abstract
Uterine lipoleiomyomas are rare variants of leiomyomas that usually occur in postmenopausal women. Their incidence ranges from 0.03% to 0.2%. Few cases of laparoscopically resected lipoleiomyomas have been reported in the literature. Further accumulation of lipoleiomyomas could help establish an accurate preoperative diagnosis of this uncommon and benign mesenchymal tumor.
1 CLINICAL IMAGE
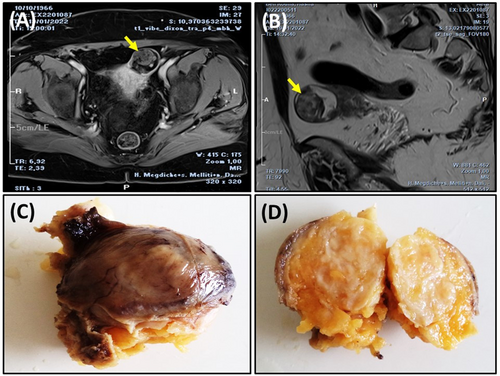
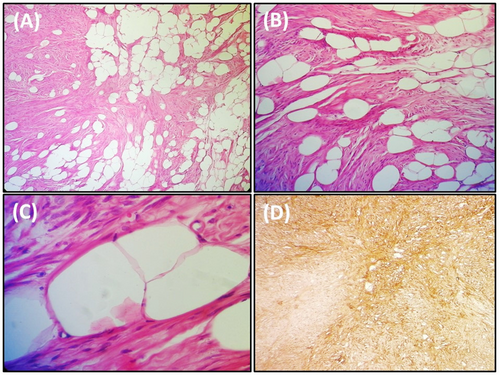
A 57-year-old postmenopausal gravida seven para five woman, presented with a 6-month history of pelvic pain. The gynecological examination was unremarkable. Transvaginal ultrasound showed a well-defined hyperechogenic uterine mass. Pelvic MRI revealed a fatty, heterogeneously enhancing subserosal mass in the anterior wall of the uterine body (Figure 1A,B). The patient underwent laparoscopic resection of the uterine mass. Grossly, the tumor was well-circumscribed and measured 4 × 3 × 2.5 cm (Figure 1C). On cut section, it showed a yellowish-white cut surface (Figure 1D). Histological examination of the nodule revealed a benign mesenchymal proliferation made of spindle-shaped smooth muscle cells arranged in a whorled pattern intermingled with mature adipocytes (Figure 2A–C). An Immunohistochemical study showed positive staining of the spindle-shaped smooth muscle cells with Desmin (Figure 2D). The final pathological diagnosis was uterine lipoleiomyoma. The postoperative recovery was uncomplicated. Although imaging studies play an important role in identifying the fat component and determining the site of the lesion, the definitive diagnosis is based on histopathological examination.1 The treatment of uterine lipoleiomyomas depends on the symptoms and the size of the tumor.2 Lipoleiomyomas carry an excellent prognosis. When asymptomatic, no surgical intervention is usually required.
AUTHOR CONTRIBUTIONS
Faten Limaiem: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; writing – original draft; writing – review and editing. Ahmed Halouani: Investigation; methodology; resources; supervision. Nizar Ben Aissia: Supervision; validation; visualization.
ACKNOWLEDGEMENT
None.
FUNDING INFORMATION
We did not receive funding for this article.
CONFLICT OF INTEREST
None declared.
ETHICAL APPROVAL
All procedures performed were in accordance with the ethical standards. The examination was made in accordance with the approved principles.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




