Interatrial septum dissection, severe aortic stenosis, and paravalvular mitral regurgitation: A rare combination and their hemodynamic interrelationship
Abstract
Left atrial wall dissection is a rare entity with controversial management approaches. We report the case of an 85-year-old woman with a mitral bioprosthetic admitted for heart failure. Diagnosis of atrial septum dissection, severe aortic stenosis, and paravalvular mitral regurgitation was established. A percutaneous approach provided clinical improvements.
1 INTRODUCTION
Left atrial wall dissection (LAWD) is a rare condition with a wide clinical presentation. In addition, the management of the condition is yet to be properly studied. The first case of LAWD was reported in 1887 by Maguire.1
LAWD is a false, blood-filled cavity caused by the discontinuation of tissue from the mitral annulus to the left atrial free wall or interatrial septum.2 A systematic review of published cases from 1979 to 2014 by Fukuhara highlighted that the majority of cases had an iatrogenic etiology secondary to mitral or aortic valve surgery or percutaneous coronary intervention. Among noniatrogenic etiologies, myocardial infarction, infectious endocarditis, tumor, trauma, and spontaneous dissection were the leading causes.3
In the last decade, there has been an increase in the number of LAWD cases alongside the rise of complex percutaneous procedures, including circumflex artery angioplasty, mitral valve valvuloplasty, and transcatheter valve implantation (TAVI).4 Recently, the analysis of two national registries revealed a rise in coronary angioplasty procedures by 15.8% in the United States and 36% in Japan from 2013 to 2017.5 Additionally, from 2013 to 2016, the number of MitraClip procedures rose by 84.4% annually. However, mitral valve replacements decreased by 5.6% per year.6 This trend may explain the likelihood of an increase in the incidence of LAWD as a complication of percutaneous techniques in the near future.
LAWD commonly occurs in the posterior wall, closely related to the mitral valve. However, LAWDs in the interatrial septum are becoming prevalent, as a consequence of the increase in procedures that require transseptal suction, such as edge-to-edge mitral valve repair and pulmonary vein isolation.5
LAWD has a wide clinical spectrum, from the absence of symptoms to heart failure and cardiogenic shock. A relationship has been theorized between the dissection size, resulting hematoma, and mitral valve and left ventricle filling compromise and hemodynamic instability and heart failure presentation.6
In a shock situation, emergency surgery is required. Notwithstanding, the majority of LAWDs are managed conservatively, especially those resulting from percutaneous procedures. A close clinical and imaging follow-up is necessary, existing a discordance in determining the most appropriate timing for surgery.4
Given the rarity of evidence on the management of this rare entity, this report aimed to contribute to the literature by presenting a new case. This is the first reported case in which severe aortic stenosis, paravalvular mitral regurgitation complicated with hemolytic anemia, and LAWD coexist.
2 CASE REPORT
We report the case of an 85-year-old woman with a history of mild degenerative aortic stenosis and severe mitral regurgitation due to posterior leaflet prolapse. Mitral valve replacement surgery was indicated and Mosaic 27 bioprosthesis was implanted. During the intervention, a reentry in extracorporeal circulation was necessary owing to the immediate development of a significant paravalvular dehiscence in the septal portion of the mitral ring. In addition, as a consequence of this rarely placed dehiscence and mild paravalvular regurgitation, hemolytic anemia developed.
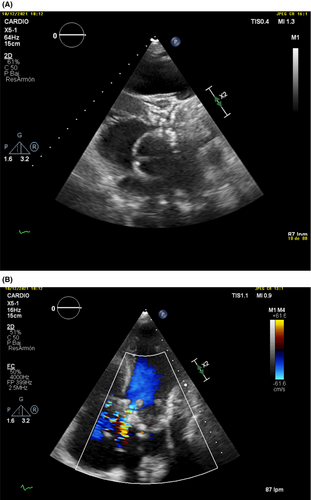
Over the next 7 years, the patient's aortic stenosis became severe and symptomatic, exhibiting signs and symptoms of left and right heart failure; in addition, there was a severe accentuation of the patient's diagnosed hemolytic anemia, with 6 d/gl of hemoglobin. Other anemia etiologies, such as digestive tract bleeding, were ruled out with endoscopic studies. In addition, high levels of reticulocytes, low levels of haptoglobin, and presence of schistocytes in the blood smear proved the presence of hemolysis. A transthorathic echocardiography (TTE) was performed to assess left ventricular systolic function, aortic valve disease, and mitral valve disease. It was described as a degenerative aortic valve with severe calcification and stenosis, moderate paravalvular mitral regurgitation with slightly raised gradients of the mitral bioprosthetic, severe pulmonary hypertension, and dysfunctional right ventricle (Figure 1). Medical therapy was unsaturated with scares clinical improvement. The case was discussed in the weekly Heart Team session, and given the high surgical risk, it was decided that TAVI should be performed.
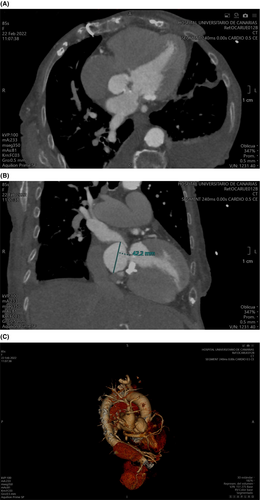
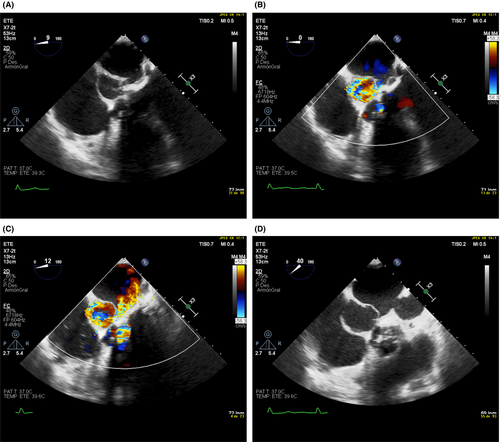
The preparation for TAVI included a cardiac contrast computed tomography for characterization of aortic annulus, coronary ostium location, and patency of the arterial femoral iliac branches. The practiced study resulted in an accidental detection of LAWD, described as a continuity solution of the septal portion of the mitral ring that extends to form an interatrial septum dissection flap (Figure 2). In light of these findings, a transesophageal echocardiography (TEE) was performed. This imaging modality contributes to the better assessment of the interatrial septum, blood flow by the Doppler technique, and hemodynamic interaction between LAWD and mitral valve, without the acoustic window limitation associated with TTE. It was described as a moderate paravalvular mitral regurgitation. One of the regurgitant jets was in the direction of the interior of a thin-walled cavity located in the interatrial septum, with systolic expansion of its walls, protruding towards the right atrium. These findings were diagnostic for LAWD (TEE, Figure 3).
When the heart failure clinic was medically compensated, the patient underwent TAVI. The outcome was favorable, and after discharge refers to an adequate functional class without heart failure clinic and hemoglobin levels similar to those reported before the severe aortic stenosis development.
3 DISCUSSION
LAWD is a rare entity with variable symptomatology. In our reported case, the patient was diagnosed with LAWD 7 years after the surgical implantation of a mitral bioprosthesis, in the context of heart failure secondary to severe aortic stenosis complicated with severe hemolytic anemia. The location of the majority of LAWDs with a mitral origin is the posterior wall of the ring, characterized by several anatomical factors, such as the mitral ring frailty, calcification, suture traction, endocardial disruption during the native valve debridement, and posterior prosthesis mismatch.7 LAWDs of the atrial septum are more frequent after aortic valve surgery.8 This patient underwent a complex surgery in which a disruption of the septal portion of the prosthetic suture was repaired with the need for reentry in extracorporeal circulation. During follow-up, mild paravalvular regurgitation was diagnosed; however, the severity progressed to moderate, alongside associated severe aortic stenosis. Tissue fragility could have been a notable predisposing factor for the development of this complication.
Hemolytic anemia of valvular origin is generally related to mechanical valves, although paravalvular regurgitation of a bioprosthesis can also produce it.9 The patient developed chronic anemia after mitral valve surgery until the patient suffered a severe exacerbation coincident with severe aortic stenosis and LAWD development. The after-load increment derived from the aortic valve disease could increase the velocity of the paravalvular regurgitant flow, thus producing a hemolysis enhancement. After TAVI, the hemoglobin level stabilized and returned to the basal value. In patients undergoing TAVI with coexistent significant mitral regurgitation, up to a 66% decrease after the procedure of the latter has been reported. This fact probably impacted the clinical course of our patient.
The clinical evolution and prognosis of LAWD are poorly understood. The clinical manifestations seem to be dependent on the time of evolution, size, and outflow tract compromise.11 Acute presentations, the most frequent ones, can exhibit cardiac tamponade and hemodynamic instability.2 Notwithstanding, the most advanced cases, mostly secondary to percutaneous procedures, are associated with a variety of symptoms that include dyspnea, palpitations, fever, chest pain, and hemodynamic stability.
Other authors have reported cases in which circumflex artery compression and subsequent ischemic severe mitral regurgitation were described as LAWD complication.12 Our patient was clinically stable for 7 years, with paravalvular mitral regurgitation and mild aortic stenosis. The turning point of the patient's evolution was the progression of the aortic stenosis to severe, aggravating the patient's chronic hemolytic anemia and precipitating the admission for heart failure. Hence, the LAWD was not acute, and the patient was hemodynamically stable.
LAWD diagnosis requires a multimodality imaging approach, including TTE, cardiac magnetic resonance imaging (MRI), and cardiac tomography (CT).13 TEE is a bedside technique useful in post-surgical patients that allows three-dimensional reconstruction and accurate delimitation of size and location. The Doppler assessment allows an analysis of the left ventricle inflow tract and pulmonary veins drainage.14 Cardiac MRI is the preferred option for tissue characterization, as it visualizes the presence of thrombi inside the LAWD and confirm its resolution during follow-up.15
Considering all of the above, A. Cereda et al. suggested a diagnostic approach algorithm in which TEE is proposed as the first-line test when LAWD is suspected. If the patient is hemodynamically stable, a CT or cardiac MRI can confirm the diagnosis; in addition, they are the most appropriate methods for follow-up. In our case, the diagnosis was made in the planning CT before TAVI and, subsequently, TEE was performed to evaluate compromise of surrounding structures.
Today, there are no clinical guidelines or management consensus on this pathology. In addition, its treatment is controversial. Historically, the surgical approach has been the preferred option in most cases, especially those with associated hemodynamic instability. However, an optimal surgical technique is not yet established. There are two types of procedures: (1) entry closure by an edge-to-edge matrasses suture or a bovine pericardial patch, and (2) internal drainage.15 A percutaneous drainage was performed in just one case, after a complicated coronary intervention.16 Although recent nonsurgery-associated cases of LAWD have followed an expectant and conservative strategy with satisfactory evolution,4 some authors suggest that anticoagulation reversion and follow-up ETE or CT should be considered if it is risk affordable.17 Some of the reported cases had spontaneous resolution of LAWD and lower mortality, particularly for percutaneous etiologies.2, 4 Considering the high surgical risk in our patient and theorizing a left ventricle after-load reduction after TAVI, decrease in flow velocity in the dissection section, and consequently, anemia alleviation, we decided to use TAVI implantation and nonsurgical approach for LAWD treatment. The clinical evolution confirmed the management, and the patient remained asymptomatic without new heart failure admissions in addition to the patient experiencing hemolytic anemia improvement.
4 CONCLUSION
LAWD is a rare disease, with multiple etiologies and controversial management. A multimodality imaging approach that considers the advantages and disadvantages of every technique is required for diagnosis. The management is even more challenging when other valvular diseases, such as aortic stenosis and paravalvular mitral regurgitation, are associated with the condition. Although surgery has been the paradigm in most of the reported cases, a conservative or percutaneous approach may be appropriate in cases with a high surgical risk and stable hemodynamics, even in those that require the treatment of concomitant comorbidities. This LAWD case was treated with TAVI and thereafter, follow-up was initiated; the patient achieved clinical stability and improvement in anemia.
AUTHOR CONTRIBUTIONS
Mauro Di Silvestre Alonso: Writing – original draft; writing – review and editing. Rebeca Muñoz-Rodríguez: Writing – original draft. Aida Tindaya: Investigation. Francisco Bosa-Ojeda: Writing – review and editing. Antonio Barragán: Data curation; validation. Alfonso Bonilla: Supervision; validation. Juan Lacalzada-Almeida: Conceptualization; supervision.
ACKNOWLEDGMENT
None.
FUNDING INFORMATION
There is no other funding details.
CONFLICT OF INTEREST
The authors declare no conflict of interest for this publication.
PATIENT CONSENT STATEMENT
The patient consent has been signed and collected in accordance with the journal's patient consent policy. The document is signed by her son because the patient has died.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




