Foreign body reaction granuloma mimicking an aggressive tumor of the mandible
Abstract
Inflammatory granuloma caused by a vegetable foreign body is a lesion that can develop in the oral cavity. It results from the implantation of vegetable matter, leading to an inflammatory reaction and the development of bone resorption. This case highlights the importance of clinicians' awareness regarding this uncommon disorder.
A 7-year-old male patient, in good general condition, presented for a painful right lower genian mandibular tumefaction with inflamed skin persisting for more than 1 month. On palpation, the swelling was indurated and difficult to mobilize in deep planes. The patient had multiple mobile cervical lymphadenopathies in the jugulocarotid and spinal chains.
Intraoral examination revealed an ill-defined vestibular redness facing the erupting right mandibular first molar (46), which was painful to percussion. On probing, a distal pocket of 8 ml in depth was noted.
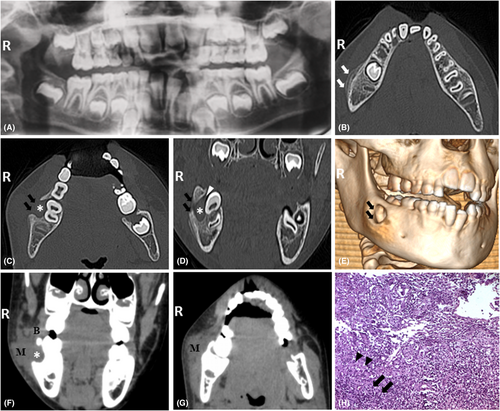
The panoramic radiograph (Figure 1A) was featureless. CT scan revealed a well-limited hypodense image without a condensation line, facing the vestibular side of the (46) and destroying the vestibular table from the outset (Figure 1C–E). The multilamellar periosteal reaction was also noted (Figure 1B). Narrow window sections (Figure 1F,G) revealed thickening of the masseter muscle and a partial thickening of the buccinator. Radioclinical confrontations were in favor of a potentially aggressive lesion. Biopsy confirmed the diagnosis of a vegetable foreign body inflammatory granuloma (Figure 1H). The treatment was the removal of the skin lesion with bone cavity curettage. The evolution was favorable.
The current case presents an uncommon oral disorder, known as foreign-body reaction, resulting from the implantation of food vegetable particles.1 This rare clinical entity has received several nomenclatures, of which hyaline ring granuloma is the most current. According to the literature, it manifests in several areas, including the lung, gastrointestinal tract, and oral cavity. Women are less affected than men, with the highest incidence in adults. The mandible is more affected than the maxilla. This pathology is mostly reported in edentulous patients with prostheses. It is associated with odontogenic cyst walls, extraction sockets, deep periodontal pockets, and partially erupted teeth as in the present case.1 We, herein, reported an unusual oral osseous lesion in a child with clinical and radiographic features possibly leading to misdiagnosis and inadequate treatment, including an excessively aggressive approach.2 Once aware of this disorder, clinicians may prevent it, provide the proper diagnosis, and indicate the appropriate treatment.
AUTHOR CONTRIBUTIONS
Dr. R. K. contributed to the study design, radiographs' analysis, and writing of the paper. Dr. I. CH. and Dr. R. Z. contributed to the study design and radiographs' analysis. Dr. B.S. participated in the realization and interpretation of the histological sections. Dr. T. BA. supervised the study and contributed to the radiographs' analysis, and the writing of the paper.
ACKNOWLEDGEMENTS
None.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
CONSENT
Written informed consent was obtained in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




