Localized skin mottling associated with acute gastric dilatation
Abstract
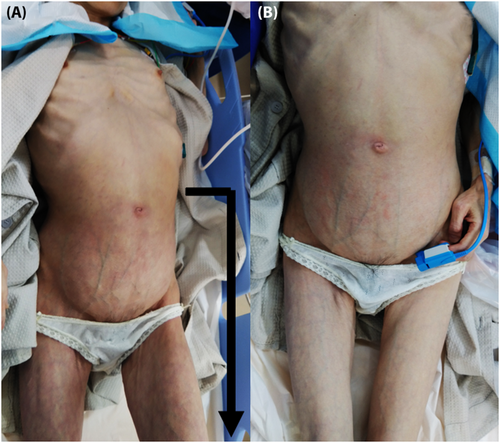
We present a case of a 55-year-old woman complaining of abdominal distension owing to acute gastric dilatation. Her localized skin mottling had spread from the lower abdomen to both knees. The skin mottling in the area affected by gastric dilatation improved immediately after stomach emptying using a gastric tube and upper endoscopy.
1 INTRODUCTION
Acute gastric dilatation is often observed in patients with eating disorders who have a history of overeating. Several complications related to gastric dilatation have been reported, that is, gastric rupture, heart rhythm disorders caused by neurological compression, aortic occlusion with mesenteric ischemia syndrome, and abdominal compartment syndrome.1
Herein, we report a case of acute gastric dilatation complicated by localized skin mottling.
2 CASE PRESENTATION
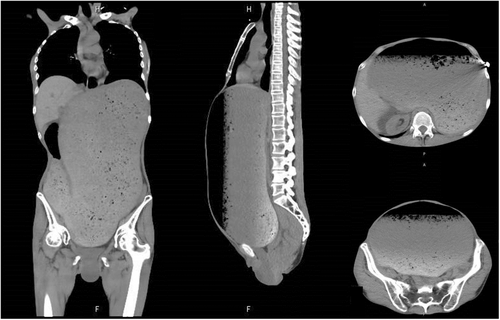
A 55-year-old woman was admitted to our hospital complaining of abdominal distension. Her body mass index is 13.4. She had an eating disorder and had continued binge eating since the night before. She was alert and conscious on arrival with the following vital signs: blood pressure, 89/56 mmHg; pulse, 128 beats per minute; regular respiration rate, 18 breaths per minute; blood oxygen saturation of 99% room air; and body temperature, 37.2°C. Physical examination revealed that the abdomen was distention and rigidity. Her skin mottling had spread from the lower abdomen to both knees (Figure 1A). A computed tomography scan showed food residues filled from the esophagus to descending duodenum (Figure 2). Approximately 5 L of food residue was aspirated using a gastric tube and upper endoscopy. After aspiration of gastric food residue, the skin mottling rapidly returned to normal (Figure 1B), and her vital sign had become stable.
3 DISCUSSION
There are several complications of acute gastric dilatation often observed in patients with an eating disorder.1 However, in patient with gastric dilatation, skin discoloration in the localized area supplied by an artery is a rare finding.
We should be aware of gastric rapture in the complication of gastric dilatation. When acute gastric dilatation progress to gastric rupture, the condition of the patient develops a septic shock state, and skin discloration appears systemic. Skin discoloration, that is, skin mottling is caused by skin hypoperfusion and is often a clinical sign in patients in shock.2 The previous report showed skin mottling disappeared after treatment of shock due to adenovirus infection.2 Skin mottling caused by septic shock has spread to systemic, while that caused by ischemic shock is localized and temporary.
This report focused on localized skin mottling from the lower abdomen to both knees associated with acute gastric dilatation in the patient. The skin area supplied by the inferior epigastric artery was discolored (Figure 1A). The skin mottling caused by gastric dilatation disappeared immediately after stomach emptying (Figure 1B). Gastric dilatation of this patient caused compression of the inferior epigastric artery; therefore, her lower abdomen experienced temporary peripheral circulation insufficiency.
The standard treatment of acute gastric dilatation is early nasogastric decompression and expulsion of stomach contents. In gastric rupture, the patient of hemodynamic will be continued to unstable without disappearing systemic skin mottling even after aspiration of gastric food residue. Unfortunately, some patients die as a result of gastric rupture.3
4 CONCLUSION
There are several complications of acute gastric dilatation. Localized skin mottling disappeared immediately is a rare complication of acute gastric dilatation.
AUTHOR CONTRIBUTIONS
Yoshiteru Tominaga: Project administration; writing – original draft. Ichiro Hirayama: Conceptualization; writing – review and editing. Tetsuhiro Yano: Visualization. Kazuto Kurihara: Resources. Mitsuru Ishii: Supervision.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest in this article.
ETHICS STATEMENT
Our institution does not require ethical approval for reporting individual cases.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




