A case report of sacral neuromodulation tined lead migration into the rectum
Abstract
This report describes a 26-year-old woman who underwent sacral neuromodulation explant following lead migration and rectal wall penetration. Her device was implanted due to persistent urinary retention. The tined lead wire was dissected to the fascia and cut. The rectal part of the lead was removed with gentle traction.
1 INTRODUCTION
In the early 1980s, Tanagho and Schmidt developed sacral neuromodulation (SNM), an effective and minimally invasive approach for the treatment of refractory overactive bladder, nonobstructive urinary retention, fecal incontinence, and chronic constipation.1, 2
Although SNM is generally considered to be a safe procedure, adverse events are usually classified as infection, pain at the implant site, adverse stimulation, lead migration, lead breakage, hardware issues, adverse change in bowel function, and loss of effectiveness.3 A meta-analysis conducted in 2021 by van Ophoven et al. revealed a pooled adverse event rate of less than 25% following permanent SNM in patients with neurogenic lower urinary tract dysfunction. The most common adverse events were loss of effectiveness (4.7%), infection (3.6%), pain at the implant site (3.2%), lead migration (3.2%), and adverse stimulation (2%).4 Although lead migration following sacral neuromodulation is a relatively rare event, it is also the second most common indication for surgical intervention.5 Thus, this report describes the management of a case of a migrated tined lead that presented as a foreign body in the rectal lumen.
2 CASE REPORT
A 26-year-old woman underwent sacral neuromodulation with the implantation of tined lead (3889-28, Medtronic, Minneapolis, Inc.) and InterStimTM (Medtronic, Minneapolis, MN) due to persistent urinary retention, self-clean intermittent catheterization, and frequent urinary infections. The procedure was uneventful, and there was more than 50% response to the treatment, and the patient became catheter-free. 15 months later, she presented with the complaint of feeling a foreign body in the rectal canal. Her past medical history included constipation and a right-side nephrectomy at the age of 14 due to uncontrolled recurrent pyonephrosis and renal function impairment.
Eight months following the successful implantation of SNM, she started to occasionally turn off the battery, and since she was able to urinate well, this practice continued. Approximately, 15 months after surgery, the patient experienced severe diarrhea and gastroenteritis for 3 weeks, treated by hospitalization and intravenous and oral medicines, before the sensation of the presence of a rectal foreign body. In the clinical examination, the patient's general condition was good, and there was no evidence of fever or peritonitis. In the rectal examination, lead was touched inside the anal canal, and migration was evident on pelvic X-rays (Figure 1A,B).

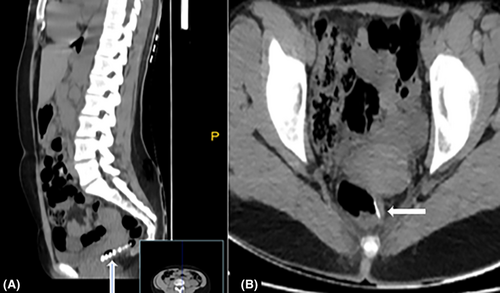
A computed tomography (CT) of the pelvis was performed in order to exclude the presence of a deep pelvic collection, indicating penetration of the tined lead into the rectal lumen and proper positioning of the implanted pulse generator (IPG) (Figure 2A,B).
Following consultation with a gastroenterologist, the interdisciplinary medical team concluded that the tined lead could be removed without additional colonoscopy.
The patient was placed in a prone position with abducted hips and prepped with chlorhexidine. Under general anesthesia, incisions were made on the left side of the lateral buttocks, and the implanted pulse generator was removed. The lead wire was dissected down to the fascia and cut sharply with scissors without being extracted through the sacral foramen to avoid contamination with fecal material at the surgical site (Figure 3A,B).
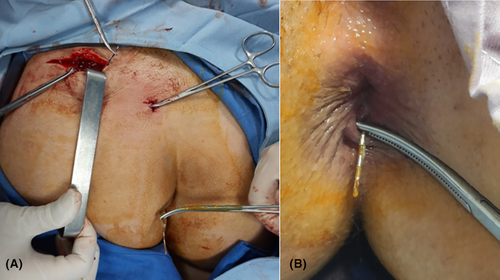
The remaining part of the lead in the rectal canal was removed with hand over hand gentle traction using Kelly clamps. The surgical site above the sacrum was washed out with an antibiotic solution of vancomycin and gentamycin and closed primarily.
The patient received broad-spectrum IV antibiotics (metronidazole 500 mg three times a day, and ceftriaxone 1000 mg twice a day) and was discharged the following day under the coverage of oral antibiotics (Ofloxacin and metronidazole); however, remained under observation for a week. There were no symptoms of peritonitis or fever. During the follow-up 6 weeks later, the patient's general condition was good, with no problem at the surgical site, and micturition was preserved without any significant postvoid residual; thus, reimplantation of the device was not justified.
3 DISCUSSION
The present case illustrates the interdisciplinary removal of a complete SNM device following the migration of an intact tined lead through the rectum wall.
As the number of patients implanted worldwide increases, such situations could be encountered by SNM implanters. To date, the majority of discussion regarding broken leads during SNM removal focuses on patients undergoing MRI with non-MRI compatible devices.6 In a study by White et al., the timing of adverse events varied depending on the type of complications. The mean time between SNM implantation and complication varied from 0.3 days for hematomas to 24.6 months for lead migrations. An increased risk of adverse events was associated with a history of trauma, a change in body mass index, participation in a pain clinic, and prior adverse events.7 As in this case, there was no trauma or provable incident which could be considered as the etiologic factor resulting in rectum penetration, we hypothesized that the rectum penetration was caused by spontaneous migration and facilitated by bowel contractions during a period of severe diarrhea. However, due to the substantial rate of explants and revisions, better instructions should be provided on how to completely remove tined leads. Practitioners alternate between pulling the lead back through the implantable pulse generator pocket, dissecting to the original incision from which it was placed, or making a larger incision to reach the S3 foramen.
In the event of a lead fracture, there has been debate over whether it should be left in situ or removed, by all means, owing to the possibility that the lead may migrate into surrounding tissues or organs, as well as the potential complications of peritonitis as a result of intestinal perforation. One case of endoscopic retrieval of a migrated tined lead fragment from the sigmoid colon following an accidental wire fracture during a previous removal attempt has been reported.8 As the SNM device in our case was not fractured, an integrated surgical approach was required to explant the lead wire and IPG.
A surgical technique for the removal of tined lead wires for InterStim devices through the sacral foramina was described by Okhunov et al., this procedure involves dissection of the fascia to the level of the fascia and gentle traction using a clamp. The procedure is contraindicated in cases of intestinal injury due to the possibility of bacterial seeding along the lead passage, which may result in presacral abscess formation or sacral osteomyelitis.9
By utilizing the combined surgical technique, the penetrating lead wire can be retrieved in order to prevent bacteria from seeding inside the surrounding tissues, preventing complications. Due to the fact that primary closure of small and extraperitoneal intestinal wall defects is not considered beneficial, it was left open for secondary healing. In cases of larger defects or intraperitoneal localization, an endoscopic clipping could be considered.
4 CONCLUSION
As tined lead migration into the intestinal lumen is a rare and delayed complication, physicians should maintain a high index of suspicion in order to diagnose the condition early on. The patient in our case did not exhibit any urinary symptoms, and the lead was functioning. As part of a comprehensive management strategy, patients should be evaluated for other symptoms in addition to urinary symptoms. Furthermore, no protocol for removal has yet been established. We propose to implement a combined multidisciplinary approach to neuromodulation surgery as a salvage strategy.
AUTHOR CONTRIBUTIONS
Farzaneh Sharifiaghdas: Data curation; project administration; supervision; writing – review and editing. Mohadese Ahmadzade: Data curation; investigation; writing – original draft; writing – review and editing. Hamidreza Rouientan: Data curation; investigation; writing – original draft; writing – review and editing.
ACKNOWLEDGMENT
None.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




