Orbital apex syndrome due to herpes zoster infection in a patient with chronic kidney disease: A case report
Abstract
We report the case of an 89-year-old man with typical herpes zoster ophthalmicus on the left side of his face with delayed clinical presentation of orbital apex syndrome. After treatment with intravenous antiviral agents and corticosteroids, the patient fully recovered. Clinical suspicion should be concerned in immunocompromised cases.
1 INTRODUCTION
Herpes zoster is a viral infection caused by varicella-zoster virus of the Herpesviridae family that can cause systemic complications in humans.1 Usually, the virus is latent in the neurosensory ganglion and reactivates in patients with weak immune system.2 The ocular manifestations are observed in 20–70% of all cases of herpes zoster ophthalmicus.3, 4 The estimated incidence of herpes zoster ophthalmicus in herpes zoster infection is 1.1 cases per 100,000 person-years annually.5 Reactivation of the varicella-zoster virus in the trigeminal ganglion can cause various forms of eye involvement from anterior to posterior segments, such as blepharitis, keratoconjunctivitis, anterior uveitis, and retinal involvement.3, 4 Additionally, due to reactivation, neuro-ophthalmic manifestations are found less frequently than ocular complications, including optic neuritis and cranial nerve palsies.6 Orbital apex syndrome (OAS) is a very rare complication of herpes zoster ophthalmicus7 that results in symptoms of increased severity. Verhaeghe et al.8 reviewed OAS cases secondary to herpes zoster ophthalmicus, which revealed only 14 reported cases from 1966 to 2015. In recent years, several cases OAS caused by herpes zoster infection have been more reported.9-14 Regarding OAS, various clinical presentations, treatments, and long-term sequelae can occur. Current evidence published in the literature suggests that OAS treatment is possible using antiviral plus anti-inflammatory drugs via either an oral or intravenous route. However, a definitive treatment of this condition remains unclear.8-16
Herein, we present a case of OAS due to herpes zoster ophthalmicus in an immunocompromised Thai patient.
2 CASE HISTORY
An 89-year-old man presented with a rash and vesicle on his left forehead. The patient had underlying diabetes mellitus, hypertension, dyslipidemia, and triple-vessel disease. He also had a history of coronary bypass surgery and chronic kidney disease (CKD) stage 3 without hemodialysis. The patient had previously undergone cataract surgery in both eyes with pseudophakia. His best-corrected vision was 20/25 in both eyes. He had primary open-angle glaucoma and well-controlled intraocular pressure with latanoprost in both eyes. His optic disk status was sharp pink with a 0.8 cup-to-disk ratio. The patient underwent stable visual field testing within the last 3 years. He was diagnosed with herpes zoster ophthalmicus by his internist and administered 800 mg of acyclovir 5 times daily for 10 days and 300 mg gabapentin before bedtime to control neuralgia for a month. Subsequently, his rash and neuralgic symptoms improved.
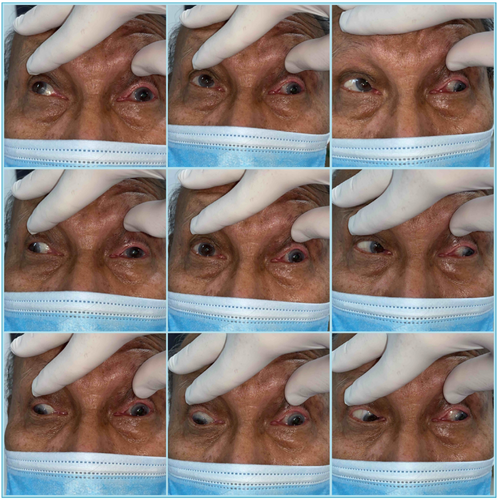
Again, the patient presented with complaints of blurring of vision and diplopia. He presented to the ophthalmology clinic for an evaluation, which showed an old scale and crust on his left forehead compatible with the left ophthalmic division of the trigeminal nerve, with decreased sensation (Figure 1). He had complete ptosis of the left eyelid. His right eye's visual field and color vision were normal. However, his left eye had color deficits that were revealed via an Ishihara test. Ocular duction of his right eye was normal; however, a 10% residual limitation to supraduction and infraduction was observed and adduction did not pass the midline of his left eye (Figure 2). Incyclotorsion was detected in attempted downgaze of the left eye. His best-corrected vision was 20/30 in his right eye and hand movement vision in his left eye. Furthermore, a relative afferent pupillary defect was present in his left eye. An examination of his anterior segment was unremarkable, with no chemosis, proptosis, or periorbital edema. Further, his optic disk was sharp pink with a 0.8 cup-to-disk ratio. There was no inflammation in the anterior chamber, and no evidence of retinitis or choroiditis after dilatation. Optical coherence tomography was performed to exclude the possibility of a retinal cause of visual loss. However, the results were unremarkable. Involvement of the optic nerve, oculomotor nerve, and ophthalmic division of the trigeminal nerve prompted a diagnosis of left OAS.

3 DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS, AND TREATMENT
The other location of pathology could be the cavernous sinus or superior orbital fissure area. By the way, evidence of optic neuropathy made these areas less likely. The possible etiologies were infection, inflammation, or vasculopathy event by onset.
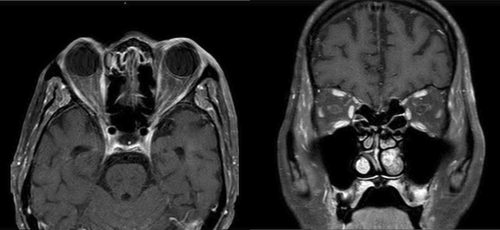
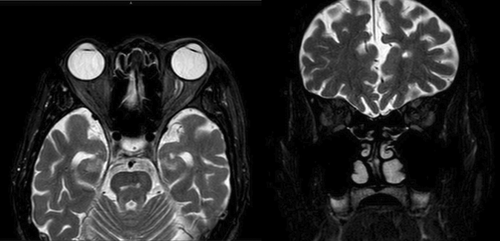
The following laboratory test results indicated a normal complete blood count: white blood cells, 6500/μl (4500–10,500); polymorphonuclear leukocytes, 61.5% (25–75); lymphocytes, 25.7% (20–40); and platelets, 161,000/μl (162,000–402,000). These results also revealed an erythrocyte sedimentation rate of 98 mm/h (0–20) and C-reactive protein level of 0.9 mg/L (0–5) that was unremarkable. Serological testing for human immunodeficiency virus was negative; treponema pallidum hemagglutination was non-reactive. Chest radiography revealed no abnormal findings. A lumbar puncture showed no pleocytosis and was negative for cytology, meningitis, and encephalitis. A cerebrospinal fluid polymerase chain reaction test for seven herpes virus types was positive for human herpes virus type 3. Magnetic resonance imaging of the brain and orbit with gadolinium contrast revealed subtle enlargement of the extraocular muscles of the left orbit, enhancement of orbital fat, and optic nerve sheath enlargement of both orbits, which was more prominent on the left side (Figure 3). Magnetic resonance imaging of the orbit also showed a T2 hyperintensity of the intraorbital part of the left optic nerve without definite enhancement (Figure 4). No mass or other infiltrative lesions were observed at the left orbital apex or left cavernous sinus.
After consultation with a neurologist, intravenous acyclovir (500 mg every 12 h) and methylprednisolone (1 g/day) were initiated. Intravenous antiviral therapy was administered for 10 days; then, a prophylactic, 400 mg, oral tablet was administered twice a day for approximately 2 months. Intravenous corticosteroids for 5 days and oral prednisolone for 2 weeks at a dose of 1 mg/kg/day were administered.
4 OUTCOME AND FOLLOW-UP
After treatment, the patient's symptoms gradually improved. In particular, vision and ocular ductions gradually improved after 3 and 2 days of treatment, respectively.
At 6-month follow-up, the patient's vision had improved to 20/32 in the left eye. Ocular movement in the left eye also improved to nearly complete ductions (Figure 5). The optic disk was sharp, mild pallor in color, with an 0.8 cup-to disk ratio. At final follow-up at 6 months post-treatment, no recurrent symptoms of herpes zoster were noted.

5 DISCUSSION
Herein, we describe a rare case of herpes zoster ophthalmicus complicated by OAS in a patient with CKD. Generally, OAS is a form of ocular disorder that involves multiple cranial nerves.16 The diagnosis of OAS is based on both a patient's clinical history and a physical examination.16 In patients with OAS, orbital signs such as proptosis, chemosis, and periorbital edema can occur.16 Moreover, neuroimaging can reveal abnormalities, including optic nerve anomalies, extraocular muscle enlargement, and perioptic nerve sheath enhancement, especially in the orbital apex area.16 The common etiologies of OAS comprise inflammatory, infectious, neoplastic, traumatic, and vascular causes.16 Herpes zoster ophthalmicus is a rare cause of this condition.
The authors reviewed previous case reports describing OAS, which totaled 19 cases.8-16 Among the published cases of OAS, the average age of patients was approximately 67 (range 29–84) years.8-16 Most affected patients were women (80%).8-16 Our patient was male with an older age than previous reports. Some comorbidities were reported, including diabetes mellitus, hypertension, acquired immunodeficiency syndrome, multiple myeloma, and leukemia.8-16 Our patient had chronic kidney disease, which was never reported. The initial best-corrected vision widely ranged from a perception of light to 20/40.8-16 The average interval between rash and OAS onset has been reported to be approximately 10 (0–40) days.8-16 In our case, initial vision was hand movement, which occurred 2 weeks after the rash presentation. Regarding lumbar puncture in this aforementioned study, cerebrospinal fluid profiling showed pleocytosis, predominantly involving lymphocytes;8-16 however, it was unremarkable in our case. OAS cases that received neuroimaging, and magnetic resonance imaging showed enhancement of the extraocular muscles, optic nerve sheath, optic nerve, and soft tissue around the orbital apex,8-16 the same as for our case. The mainstay treatment of OAS consists of antiviral and corticosteroid therapy, which may be administered via intravenous or oral routes.8-16 Most studies reported initiating corticosteroids after antiviral drugs were administered for 48 h.8-16 The duration of combined treatment ranged from 2 to 6 months, depending on clinical recovery.8-16 In our case, the patient received concurrent treatment of intravenous antiviral and intravenous corticosteroids with a duration of 10 and 5 days, respectively. In most studies, 60% of patients had partially improved visual acuity, and most patients regained nearly all their ocular motility.8-16 Venous sinus thrombosis may occur as a complication of OAS with herpes zoster ophthalmicus. Since thrombosis is associated with poor outcomes, this is a concern in severe cases.10
Urgate et al.17 proposed that the pathophysiology of OAS secondary to herpes zoster infection is due to the reactivation of viral particles that had spread along the trigeminal nerve to other nerves around the orbital apex. The spreading of reactivated virus causes inflammation, vascular insufficiency, occlusive vasculitis, direct cytopathological effects, or a combination of these factors.18 Histologic evidence of herpes zoster ophthalmicus has revealed perineuritis and perivasculitis of the ciliary nerve and ophthalmic artery.19, 20 Perivascular monocytic infiltration and secondary demyelination have also been demonstrated in autopsy cases of cranial nerve palsies.21 The pathophysiology in our case could have been the reactivation of viral infection, which subsequently caused an inflammatory process rather than vascular insufficiency. The rapid and significant response to corticosteroids supports this hypothesis. The sequelae of OAS in patients with herpes zoster ophthalmicus vary from complete recovery, as was observed in our case, to deficits in vision and ocular motility.8-16 Recent data have shown that concurrent treatment with corticosteroids, either orally or intravenously, and antiviral drugs are adequate.8-16 Although OAS is a rare complication, scheduled follow-ups should be performed. If patients experience abnormal symptoms, they should seek urgent medical help.
Of note, CKD was one of the risk factors for herpes zoster infection. From recent meta-analysis, patients with CKD increase risks of herpes zoster infection with relative risk as 1.29 (1.10–1.51) (95% CI; p < 0.0001) compared with a healthy population.22 Herpes zoster infection risk increases among those with CKD and end-stage renal disease23 and is highest among patients undergoing hemodialysis and renal transplant.24 Both innate and adaptive immune system dysfunction contribute to infection susceptibility. Lymphopenia and low-albumin levels have the potential to diminish a patient's immune status.25 Concern regarding progression to OAS in those with CKD complicated by herpes zoster ophthalmicus should be highlighted. A thorough examination and follow-up can detect further complications and facilitate prompt treatment. Further prospective studies are needed to confirm the association between CKD and the progression of herpes zoster ophthalmicus to OAS.
OAS is a rare but severe complication of herpes zoster ophthalmicus. Concurrent antiviral agents and corticosteroids are proper for the treatment of this condition. To avoid poor outcomes, this complication should be considered in immunocompromised patients, especially those with CKD. Scheduled follow-ups in patients with herpes zoster ophthalmicus should be performed because late-onset sequelae can occur.
AUTHOR CONTRIBUTIONS
Worapot Srimanan treated the patient and collected clinical data. Worapot Srimanan wrote the manuscript, and Somboon Panyakorn revised the manuscript. All authors approved the final version of the manuscript.
ACKNOWLEDGMENTS
We acknowledge the assistance of Natthanose Panarojwongse, MD, ophthalmology resident, Phramongkutklao Hospital, in this manuscript preparation.
FUNDING INFORMATION
The authors did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST
None.
ETHICS STATEMENT
Study approval statement: The study protocol was reviewed and approved by the Institutional Review Board of the Royal Thai Army Medical Department (approval number: S086h/64_Exp).
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




