Double valve replacement in a case of Hedinger syndrome
Abstract
Hedinger Syndrome or carcinoid heart disease is a rare cardiac complication of neuroendocrine tumors (NET) affecting the tricuspid and pulmonary valves. Following is a case description of a patient undergoing treatment for a neuroendocrine tumor with liver metastasis, referred with symptomatic tricuspid valve regurgitation and pulmonary valve stenosis for surgical valve replacement. Planned surgical valve replacement was successfully performed before the onset of severe right ventricular failure or pulmonary hypertension in this case of carcinoid heart disease. An interdisciplinary approach and regular follow up is recommended in such cases.
1 INTRODUCTION
Carcinoid heart disease is a rare form of valvular heart disease, seen as a cardiac complication of neuroendocrine tumors (NETs) due to endocardial fibrosis, most commonly on the right side, caused by elevated levels of serotonin1 and called Hedinger syndrome.2 Operative valve replacement is the only effective treatment option for these patients, and timely surgical valve replacement provides symptomatic relief and survival benefit.3 Here, we present a successfully treated case of Hedinger syndrome with simultaneous operative replacement of tricuspid and pulmonary valves.
2 CASE REPORT
A 68-year-old female patient was referred to our department of cardiac surgery in January 2019 with a diagnosis of symptomatic TIPS (Tricuspid valve insufficiency and pulmonary valve stenosis) due to Hedinger syndrome,2 caused by a neuroendocrine tumor of the terminal ileum (Stage IV with Liver metastasis 16.7 × 10.5 cm, somatostatin receptor positive; initial diagnosis August 2017).
The patient presented with recurring episodes of carcinoid syndrome, successfully treated with Lanreotid 120 mg every 4 weeks and Interferon alpha 3 million IU every 3 days.
At presentation, the patient had dyspnea on exertion and a loss of weight but was otherwise free from symptoms under the above-mentioned therapy in the past. On examination, she had a heart rate of 65 bpm, blood pressure of 160/90 mmHg, weight of 66.1 kg, BMI of 22.6 kg/m2, had flushing of the face and clubbing of the fingers.
The preoperative echocardiography showed a high-grade tricuspid valve regurgitation, with a vena contracta of 10 mm and a normal left ventricular ejection fraction. A right heart catheterization showed the following: a total cardiac output of 3.1 L/min, pulmonary valve area of 1 cm2, a pulmonary capillary wedge pressure of 12/11 mmHg, pulmonary arterial pressure of 22/11 mmHg, and pressure in the right ventricle of 29/7 mmHg. Transthoracic echocardiography showed a normal RV function. Coronary artery disease was ruled out via angiography.
The decision to operate was taken in an interdisciplinary consensus in view of worsening valvular pathology with progression of symptoms, and a planned consecutive resection of the liver tumors.
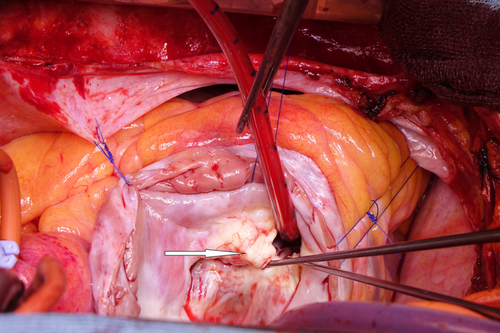
Operation was performed via a median sternotomy. Total cardiopulmonary bypass was achieved by cannulating both the superior and inferior vena cava. After cross clamping the aorta, antegrade blood cardioplegia was given and the right atrium and RVOT was opened. The tricuspid valve leaflets and chordae showed sclerotic thickening with inward rolling (Figure 1). The pulmonary valve also showed similar macroscopic changes, thus confirming the need for replacement of both valves. The tricuspid valve was replaced with a 29 mm xenograft (Bio Perimount plus 6900 Edwards Lifesciences) and the pulmonary valve was replaced with a 23 mm xenograft (Bio Perimount Magna-Ease Edwards Lifesciences) after reconstruction of the right ventricular outflow tract using an oval autologous glutaraldehyde fixed pericardium patch.
Weaning from the cardiopulmonary bypass was achieved without problems, and the patient could be transferred to the intensive care unit.
The patient showed no signs of right ventricular dysfunction through the operative and postoperative phases.
Perioperatively, the patient was treated with octreotide perfusion (50–100 μg/h) which was increased to a thrice daily regimen of 200 μg after transfer to the normal ward and reduced to a weekly depot injection on discharge. Interferon was omitted preoperatively and paused for 14 days postoperatively to reduce risk of wound infection. The patient was prescribed acetylsalicylic acid post operatively.
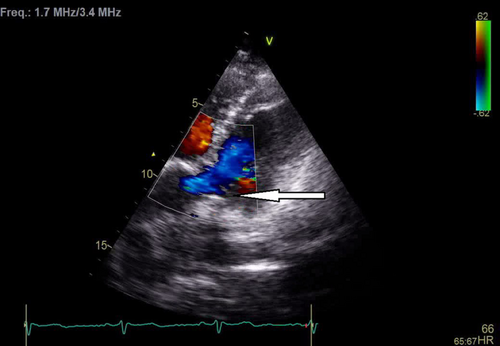
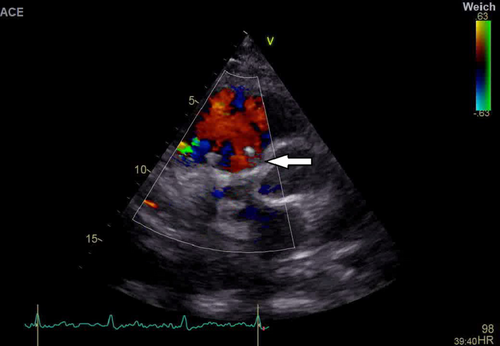
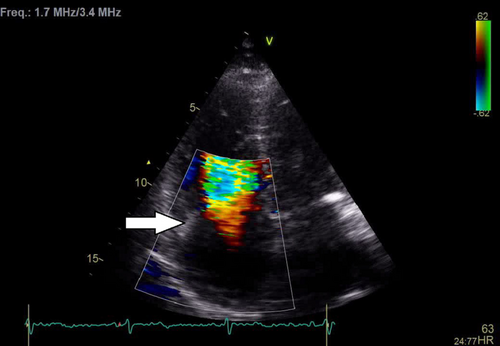
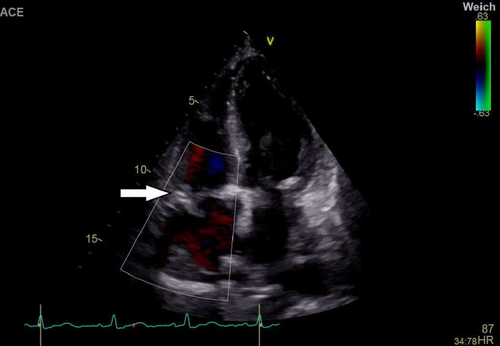
Postoperative Echo showed normal right ventricular contraction with both valve prostheses in a satisfactory position and function. The pulmonary valve showed a Vmax 2.8 m/s, dp max/mean 31/18 mmHg (Figures 2 and 3), and the tricuspid valve had a Vmax 1.5 m/s, dp mean 5–6 mmHg with no relevant paravalvular leakage around either bio prosthesis (Figures 4 and 5). A better flow profile was observed over the pulmonary valve as compared to the preoperative MRI (Figure 6).

There were no major complications postoperatively.
Further oncological follow-up and restaging after 12 months showed two suspected bone metastases in the thoracic vertebrae with a recommendation for a peptide radio receptor therapy. Valve function was uneventful.
3 DISCUSSION
Well-differentiated neuroendocrine tumors (NETs) are rare malignancies with an incidence of 5.25 per 100,000 in the general population.3 Carcinoid heart disease is observed in 3%–4% of all patients with a neuroendocrine tumor with 40%–50% incidence in patients with carcinoid syndrome.4 Simultaneous involvement of right-sided heart valves is a pathognomonic sign (TIPS: Tricuspid insufficiency with pulmonary stenosis) of Hedinger syndrome. Chronic exposure of the cardiac endothelium (esp. the right atrium and ventricle) to secretion of various peptides, vasoactive substances, and hormones secreted by tumor cells (e.g., serotonin, TGF-β1, and connective tissue growth factor) has been proposed as the pathogenesis, resulting in hyaline and mucoid cellular degeneration; accompanied by fibrous changes and focal calcification in the interstitium of the endocardium, as was observed in the valves of this patient.
Regular cardiac monitoring of patients with NETs using transthoracic echocardiography has been recommended by both the European5 and the North American Neuroendocrine Tumor Societies,6 to monitor the onset and progression of carcinoid heart disease. However, the timing for surgical valve replacement is important for the postoperative outcome in such cases. Pre-symptomatic valve replacement was not associated with late survival benefit,1 due to the inherently high mortality associated with tricuspid and pulmonary valve replacements. In the above case, the patient had a postoperative period free from complications.
This may be attributed to the timing of the operative intervention, multidisciplinary team approach, and preoperative stable general condition of the patient. Most cases of Hedinger syndrome are operated after the onset of severe symptomatic right heart failure (NYHA III-IV), onset of pulmonary hypertension, or failure to control/ improve symptoms using medical therapy. However, survival is markedly improved compared to subjects managed solely with medication, with functional symptoms NYHA class II and greater with a survival rate of 10% beyond 2.5 years.7 In this case, the decision for early operative intervention was taken in preparation for further operative therapy on the metastatic mass in the liver. Perioperative medical therapy with octreotide/Lanreotid and interferon alpha may help to reduce tumor activity and after the valve replacement also played a key role in the outcome by reducing the amount of circulating vasoactive compounds.
Both valves were replaced using xenografts, avoiding the need for long-term anticoagulation and the complications associated with it. Vitamin K antagonists can be used for 3 months after surgical valve replacement with biological prosthesis (class IIb recommendation ESC/EACTS),8 but were omitted in this case due to the presence of liver metastasis and planned surgical approach. Follow-up after 1 year showed no change in cardiac function with respect to immediate postoperative findings.
Long-term follow-up is recommended for every patient with carcinoid heart disease to monitor valve function and further treatment of the underlying tumor.
4 CONCLUSION
Patients with neuroendocrine tumors should undergo regular screening using echocardiography to rule out or monitor onset of carcinoid heart disease. Patients with Hedinger syndrome should undergo an interdisciplinary evaluation for operative valve replacement, which should be performed in symptomatic patients (NYHA class II onwards) before the onset of severe right ventricular failure or pulmonary hypertension. Higher mortality of tricuspid and pulmonary valve procedures should be taken into account as compared to other valve replacements. Planned surgical valve replacement in specialized centers may be associated with lower mortality, symptomatic relief, and overall improvement in prognosis.
AUTHOR CONTRIBUTIONS
Presheet Pathare: Conceptualization; data curation; software; visualization; writing – original draft; writing – review and editing. Michael Weyand: Conceptualization; formal analysis; funding acquisition; resources; supervision; validation. Christian Heim: Conceptualization; formal analysis; funding acquisition; investigation; project administration; resources; supervision; validation.
ACKNOWLEDGMENTS
None. Open Access funding enabled and organized by Projekt DEAL.
FUNDING INFORMATION
No funding was provided for this article.
CONFLICT OF INTEREST
The authors have nothing to disclose with regard to commercial support.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




