Adult-onset still's disease and budd-chiari syndrome: A case report
Abstract
Adult onset still's disease (AOSD) is a rare autoinflammatory disease displaying with a wide range of non-specific symptoms and budd-chiari syndrome (BCS) is an uncommon disorder characterized by obstruction of hepatic venous outflow. We present the case of a young patient who presented with persistent fever, sore throat, elbow, hand fingers and knees arthralgia with abdominal pain. The patient's symptoms had started 7 days before the referral. Imaging and laboratory data led to the diagnosis of BCS in the context of AOSD. The patient treated with corticosteroid in combination of warfarin with favorable outcome and complete improvement of signs and symptoms. We came to this conclusion AOSD complicated with BCS is a rare but potentially life-threatening entity. Clinicians should be aware of this complication.
1 INTRODUCTION
Adult onset still's disease (AOSD) is a rare autoinflammatory disease displaying with a wide range of non-specific symptoms. This disorder is associated with symptoms of muscle pain, high fever, salmon pink maculopapular rashes, liver enlargement, splenomegaly, lymphadenopathy and leukocytosis. In most cases, patients have spiking fever, arthralgia, rash and high leukocytosis but AODS is characterized by the triad of fever, muscle pain and salmon-colored bumpy rash. The exact cause of Still's disease is unknown, yet it is believed to be the result of an immune disorder, in which the immune system attacks healthy cells and tissues, such as Adenoviral infections may cause complications in autoimmune diseases.1, 2 This disease is considered a diagnosis of exclusion.3 Cardio-respiratory complications are primarily represented by pleural and pericardial disorders.1 In this entity rheumatoid factor and anti-nuclear antibody tests are usually negative, but ferritin increases sharply; however, the diagnosis is clinical and not serological.4 The prognosis is usually good, but can affects the lungs, heart and kidneys and causes life-threatening complications.5
This entity is initially treated with glucocorticoid such as prednisone, and when prednisone does not respond as the first line of treatment, interleukin-1 blockers such as Anakinra can be used.6 Flare-up of the disease is in the form of severe fatigue, lymphadenopathy and rarely fluid accumulation in the lungs and heart. Other life-threatening complications includes hemophagocytic lymphohistiocytosis, fulminant hepatitis, and sensorineural hearing loss.7
Herein we reported a rare case of youthful woman who presented with fever, sore throat, arthralgia, and acute hepatitis and eventually the diagnosis of AOSD complicated with budd-chiari syndrome (BCS) was confirmed.
2 CASE PRESENTATION
A 23-year-old woman presented to the emergency department with persistent fever, sore throat, joint pain in elbow, fingers and knees with abdominal pain. The patient's symptoms had started 7 days before the referral. On admission, the patient was alert and oriented. The fever was 39°C. Other physical examination was unremarkable. Laboratory tests were performed according to the symptoms and absence of a specific infectious source. The laboratory tests are listed in Table 1.
| Laboratory tests | Result |
|---|---|
| LDH | 1207 IU/L9 (40–280) |
| EBV IgM (VCA) Ab | Negative |
| CMV IgM Ab | Negative |
| ESR | 98 mm/h (0–290) |
| CRP | 79 mg/L (0–10) |
| ALP | 410 IU/L (44–230) |
| AST | 120 U/L (8–33) |
| ALT | 170 U/L (4–36) |
| Bili T | 0.6 mg/dl (0.3–1.2) |
| Bili D | 0.3 mg/dl (<0.3) |
| BUN | 13 mg/dl (6–24) |
| Cr | 0.9 mg/l (0.7–1.3) |
| Na | 133 meq/l (135–145) |
| K | 4.4 mmol/L (3.5–5) |
| INR | 1.1 |
| PT | 12 s (11–19.5) |
| WBC | 13,800/mcl (4000–11,000) |
| PMN | 89% |
| Hb | 11.9 gr/dl (>13) |
| PLT | 162,000 (150,000–4500) |
| U/A: WBC | 2–3 |
- Abbreviations: ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate aminotransferase; Bili D, direct bilirubin; Bili T, total bilirubin; BUN, blood urea nitrogen; CMV, cytomegalovirus; Cr, creatinine; CRP, C-reactive protein; EBV, Epstein–Barr virus; ESR, erythrocyte sedimentation rate; Hb, Hemoglobin; INR, international normalized ratio; K, potassium; LDH, lactate dehydrogenase; Na, sodium; PLT, Platelet Count; PMN, polymorphonuclear leukocytes; PT, prothrombin time; WBCs, white blood cells.
According to the persistent fever, arthralgia and abdominal pain, serum rheumatologic tests performed, which were within normal ranges. Because brucellosis is endemic in our region, the wright, coombs wright and 2ME tests were performed, which all were negative. According to the elevated liver enzymes, a panel of hepatitis tests including HBS Ag, IgM anti-HBC, HCV Ab, IgM anti-HAV, IgM anti-CMV, and IgM VCA for EBV, were requested and all were reported negative. The HIV test was also negative. Considering that the patient was under 40 years old, a ceruloplasmin level test was sent, and the test result was negative. Serum protein electrophoresis (SPEP) was not abnormal except for a slight increase in gamma protein (polyclonal gammopathy).
Thyroid tests were also within the normal range. The patient's ferritin was reported as high as 1760. Due to high liver enzymes, she underwent abdominal and pelvic ultrasound, which was normal. Considering, elevated liver enzymes and prolonged patient's fever, the patient underwent Doppler ultrasound to access the portal, hepatic and splenic veins, which confirmed the presence of thrombosis in the small hepatic veins. According to gastrointestinal counseling, the diagnosis of BCS was made.
On CT scan of the abdomen and pelvis except 126 mm spleen size (upper limit normal, there was no significant abnormality). Considering the hepatic vein thrombosis reported, hypercoagulopathy states were evaluated and protein C, protein S, Antithrombin III, factor V leiden, prothrombin 20,210 mutation were reported as normal.
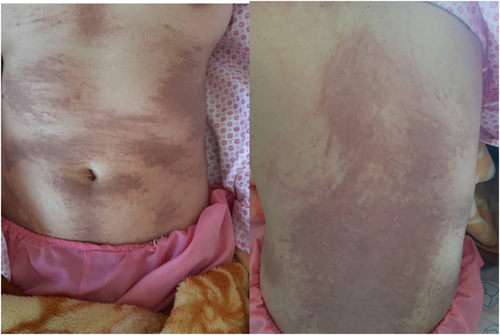
During hospitalization, the patient developed rashes on the abdomen and neck (Figure 1).
Depending on the persistence fever, acute hepatitis and the presence of thrombosis reported, bone marrow biopsy and aspiration were performed based on the hematologic consultation and the result were normal. Also, with regard to fever, sore throat and thrombosis, and high LDH level, paroxysmal nocturnal hemoglobinuria (PNH) tests included CD55 and CD59 were also performed, which were reported as normal.
Finally, given the symptoms, laboratory tests and excluding of other causes, the diagnosis of adult-onset still's disease complicated with BCS was made. Prednisolone was started for the patient and because of the BCS diagnosis we started warfarin. The patient's fever was interrupted. In the follow up, liver enzymes were becoming normal and the patient's symptoms improved completely.
3 DISCUSSION
AOSD is a rare systemic autoinflammatory disease with a prevalence ranging from 1 to 34 cases per million people.8
ASOD affects young people with an average age of 36 years at the time of diagnosis.9
It does not have specific clinical manifestation, but a wide range of symptoms is observed in these patients. Leukocytosis is commonly observed in these patients. No specific laboratory test is seen in these patients, but ferritin increases significantly. In addition to increasing ferritin and leukocytosis, erythrocyte sedimentation rate increases. Also, rheumatic diseases, infections and malignancies should be excluded before the final diagnosis of AOSD.7
According to Yamaguchi's study,10 Diagnosis of AOSD based on three major criteria include fever above 39 degrees Celsius for 1 week or more, arthralgia or arthritis lasting 2 weeks or longer, and leukostasis above 10,000/mm3 or more than 80% of polymorphonuclear and three minor criteria including sore throat, hepatomegaly, rheumatoid factor (IgM), antinuclear antibody negative and exclude infections, malignancies and other rheumatic diseases life expectancy and quality of life in AOSD patients It decreases with some complications.
Lymphohistiocytosis (HLH) occurs in 12 to 15% of AOSD patients, which is associated with increased mortality in these patients. Other complications including pericarditis, pleuritis, disseminated intravascular coagulation, thrombotic microangiopathy, fulminant hepatitis is rarely observed.11
BCS is a clinical condition that manifests itself with hepatic vein obstruction and can be curable or fatal.
This venous obstruction can be from the small hepatic vein to the inferior vena cava.12
An increase in liver enzymes is observed in 92% of patients.13
Compared with other liver diseases in BCS patients, the prognosis is acceptable with the treatment of patients. It is a rare but important syndrome because many disorders including hematologic, malignancy, and rheumatologic diseases are complicated with BCS.14
We emphasize on four points in our patient: First, in every patient with persistent fever and elevated liver enzymes the diagnosis of BCS should be kept in mind as a differential diagnosis. Second, BCS is a very rare entity in the context of AOSD. A few case reports described thrombosis in AOSD including disseminated intravascular coagulation with digital auto amputation,15 coronary artery occlusion,16 central retinal vein,17 portal vein thrombosis,17 deep veins thrombosis with bilateral pulmonary embolism.19 Third, the rashes of our patient were atypical for still's disease presented as flagellate erythema-type appearance. Often the well described typical maculopapular rash is seen in most patients and it is embedded as a major criteria in Yamaguchi criteria as well. However, other atypical cutaneous manifestations of AOSD have been reported.20 Fourth, PNH in this patient was an important differential diagnosis, which is an acquired and life-threatening disorder characterized by the triad of thrombosis, hemolytic anemia and impaired bone marrow function.21 Deficiency of CD55 and CD59 accounts for the intravascular hemolysis. Gastrointestinal complaints such as episodic abdominal pain and dysphagia or odynophagia may be the initial manifestation of the disease in approximately 10% of patients and clinicians should be aware of this manifestation.22
4 CONCLUSION
AOSD is a rare disease with unknown etiology and pathogenesis. This disease is diagnosed with the symptoms of rash, arthritis and fever after ruling out malignancies, infections and rheumatic diseases.
Thrombosis can occur in AOSD patients. BCS is thrombosis of the hepatic veins or inferior vena cava. Spontaneous outcome in symptomatic patients is poor. BCS occurs rarely in AOSD patients but can be a life-threatening disease. Disease pathogenesis is unknown, but the similarity of AOSD and BCS in the dysregulation of innate immunity can be suggested as pathogenesis.
AUTHOR CONTRIBUTIONS
Atousa Hakamifard acquired data, analyzed, and interpreted the data. Mahnaz Momenzadeh wrote the first draft of the manuscript. Mahnaz Momenzadeh, Amir Aria and Atousa Hakamifard revised the manuscript. All authors have read and approved the final manuscript.
ACKNOWLEDGMENT
None.
CONFLICT OF INTEREST
The authors declared no conflicts of interest in this study.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this case report type article as no new data were created or analyzed in this study.




