Brain abscess due to Nocardia asiatica in a 63-year-old patient with adult-onset still disease: A case report
Abstract
Cerebral nocardiosis is a rare and opportunistic cerebral infection caused by Nocardia spp., a gram-positive, aerobic bacteria of the Actinomycetes order. Patients with cell-mediated immunodeficiencies are often targeted by this microorganism, for which early diagnosis and therapeutic approach are essential.
1 INTRODUCTION
Nocardiosis is an infectious disease caused by a gram-positive, aerobic bacterium of the order of Actinomycetes; they behave as opportunistic microorganisms and are commonly found in soil, water, and organic matter, with more than 90 species identified and 54 associated with human diseases.1, 2
Infection by Nocardia often occurs in immunocompromised hosts, in particular those with a history of organ transplant, including BMT (Bone Marrow Transplant) and solid organ recipients, in which there is a high risk of mortality in the first year after transplantation.1, 3
The prevalence of nocardiosis is considered rare worldwide, and in Ecuador, it still remains unknown.
Here, we present a case of a patient with medical history of adult-onset Still's disease (AOSD) who developed neurological symptoms; further imaging testing revealed signs of infection in the brain that lead us to consider Nocardia as the etiological agent responsible for his condition.
2 CASE REPORT
A 63-year-old Ecuadorian male patient with a history of type 2 diabetes mellitus (T2DM) and adult-onset Still's disease (AOSD) was admitted to a local hospital for presenting chronic fever and fatigue. AOSD was diagnosed approximately 3 years ago and treated with 2 cycles of Etanercept, oral corticosteroids, and methotrexate. His symptoms were attributed to the usage of monoclonal antibodies. However, after completing the treatment, his condition continues to decline with persistent daily fevers.
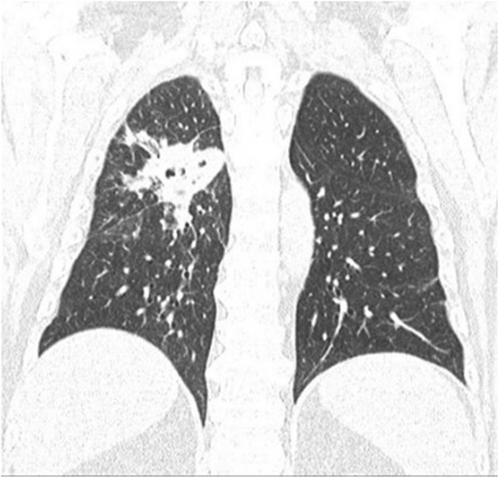
On clinical examination, the patient presented Cushing's like fascia (“moon face”) and subdermal nodules in the left hypochondrium and left forearm. A chest computed tomography (CT) scan revealed consolidation in the right lung vertex (Figure 1).
Based on the patient's immunosuppression history, tuberculosis was initially suspected, but all test results were negative, including the sputum culture.
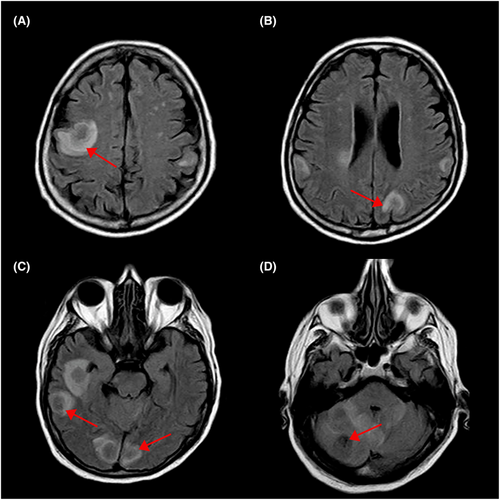
Subsequently, a fiber bronchoscopy was performed with negative results, and the patient was started on a course of Piperacillin/tazobactam and quinolone. During hospitalization, the patient became lethargic and within less than 24 h he presented left-sided hemiparesis. The neurology department was consulted to assess for a cerebrovascular accident (CVA). The brain CT scan showed hypodense lesions at the level of the anterior limb of the internal capsule and right lenticular nucleus. A magnetic resonance imaging (MRI) of the brain revealed rounded lesions at basal ganglia and bilateral subcortical cortical lesions in the frontal, parietal, and temporal lobes with bilateral cerebellar lesions of different sizes on T2-weighted imaging (T2-WI) and Fluid-attenuated inversion recovery-weighted imaging (FLAIR-WI) (Figure 2). Based on the imaging findings, the diagnostic was leaning toward infection of the central nervous system or brain metastasis.
His condition continued to decline to a state of stupor and was admitted to ICU. The patient was sedated and put on ventilatory support. Cerebrospinal fluid (CSF) reported adenosine deaminase (ADA): 11 UI/L, proteins: 110 g/dl, glucose: 82 mg/dL, Lactate Dehydrogenase (LDH): 35 U/L, negative liquid cultures, no growth in Chinese ink culture, C-reactive protein (CRP): negative for TB.
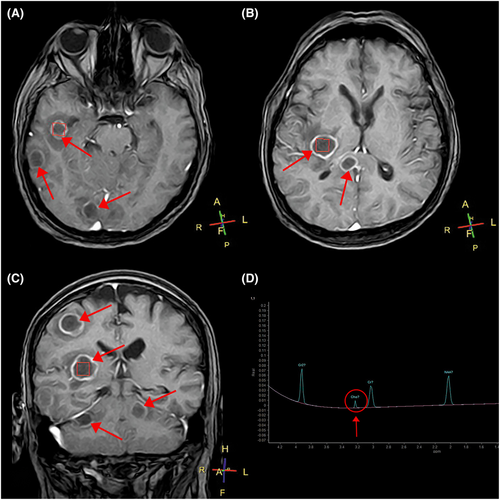
In collaboration with the infectious diseases department, the patient received antituberculous drugs plus a course of broad-spectrum antibiotics. A control brain CT scan revealed an increase in size and number of the aforementioned lesions. Brain MRI with spectroscopy showed a peak of choline that confirmed neuro infection (Figure 3). Despite the treatment, fever persisted, and symptoms were not improving. After consulting the neurosurgery department, a CT-assisted stereotactic brain biopsy of the lesions was obtained with no apparent complications, and samples were analyzed with Kinyoun stain confirming the presence of filamentous gram-positive bacillus compatible with Nocardia (Figure 4). Molecular Biology study: Sanger method Sequencing of the 16 S rRNA gene confirmed 99.83% of Nocardia asiatica. Based on these results, a change in antibiotic treatment with trimethoprim/sulfamethoxazole (TMP-SMX) was decided upon. The patient presented partial improvement; however, further complications consequent to paralytic ileus led to multi-organ failure, and death.

3 DISCUSSION
Nocardiosis is a neglected tropical disease in which microorganisms can be introduced through inhalation, ingestion, or inoculation.2, 4 Most frequently present in pulmonary diseases, followed by extrapulmonary diseases, in which the central nervous system (CNS) is the most common dissemination site due to local effects of granulomas or abscess formation in the brain, spinal cord, or meninges. Intracranial abscesses account for 2% of the cases, with a mortality rate of 31%, greater than other types of infection.4, 5 Nocardia spp. is known for its tropism to brain tissue, leading to neurological symptoms such as headache, nausea, aphasia, and hemiparesis.6
To the best of our knowledge, there is a strong association between chronic glucocorticoid therapy and nocardiosis, attributed to the inherent effects in the host's immune mechanisms, mainly decreasing cellular immunity, making patients vulnerable to these infections.1 This was evidenced in this patient with a 3-year history of AOSD chronically treated with oral corticosteroids (prednisone) and methotrexate, in addition to 2 cycles of etanercept.
In an immunocompromised patient, the infection starts in the lungs before spreading hematogenously to the central nervous system and other organs. According to the case study, the first CT scan of the chest performed on the patient showed consolidative injury on the right pulmonary vertex, corroborating the pulmonary compromise, although the patient never presented respiratory symptoms.
On MRI studies, brain abscesses produced by Nocardia are described as areas of purulent necrosis, observed as ring lesions consistent with abscess formation followed by necrosis, and edema caused by vascular exudation and infiltration.7 In the reported case, MRI images revealed similar results: rounded lesions at the basal ganglia, as well as bilateral cortical lesions in the frontal, parietal, temporal lobes, and cerebellum with different sizes on T2-weighted imaging (T2-WI) and FLAIR-WI. Interestingly, as above-stated the lesions increased in number and size further complicating the patient's state.
MRS (magnetic resonance spectrum) is optimal for differentiating between brain abscesses, gliomas, and cystic or necrotic foci.5
The core of brain abscesses lacks of the metabolites present in normal brain tissue; therefore, NAA, creatine, and choline levels are low, yet lactic acid is elevated. In addition, valine, leucine, and isoleucine are essential markers to reach this diagnosis; however, their absence does not rule out an intracranial abscess.5
The diagnosis is confirmed with direct observation through microscopy of samples prepared with a special stain such as Kinyoun, where resistant acid alcohol branched filamentous bacteria are identified, but this method is less sensitive than gram staining,8 in which Nocardia is spotted as thin and long microorganism branching with tiny noncontiguous gram-positive beads of varying sizes. Culture sensitivity is 85%–95% and is carried out in a Sabouraud glucose syrup media that generates folded yellowish-white or plaster-like colonies similar to popcorn.4, 8
The gold standard for the identification of Nocardia species is molecular biology with amplification and sequencing of one or two gene(s) among RRs (i.e., the gene coding for 16 S rRNA), hsp65, secA1, and sodA.8 Nocardia PCR testing is recommended only for patients with high suspicion of nocardiosis and no other obvious diagnosis.9
Proteomic profile analysis using MALDI-TOF MS (Matrix Assisted Laser Desorption/Ionization Mass Spectrometry) allows a rapid identification serving as an aid for an early diagnosis and prompt empiric treatment.4
Due to its pharmacokinetics and good penetration into the CNS, Trimethoprim/Sulfamethoxazole remains as the preferred drug for treating Nocardiosis.7 The recommended dose is 25–50 mg/kg per day of oral trimethoprim to the patient for 3 months. However, cost and toxicity with prolonged therapy up to 6–12 months limit its widespread use.4, 10
For less severe cases, swiss guidelines recommend routine usage of this antibiotic, but if there is no positive response or signs of toxicity are evident, switching to imipenem is recommended.
Through-out his hospitalization, our patient received levofloxacin, amikacin, linezolid, and TMP-SMX in standardized doses, that seemed to some degree helped his condition, but his severe immunosuppression was the key factor for his incomplete improvement.
During the Grand Round presented by Derung and colleagues, the usage of interferon-gamma in refractory cases of severe Nocardia infection was suggested, stating that this cytokine at the center of the immunity triggers various antimicrobial effector functions, regulating proteins in support of oxidative, nitrosative, protonated, and membranolytic defense. It also inhibits the intracellular growth of pathogens, improving the course of nocardiosis. Its success depends on the underlying molecular pathophysiology and should only be considered an adjuvant compound.11
Surgical treatment is necessary when there is a significant brain abscess(es) not responding to antimicrobial therapy or if a co-infection is suspected.8 Craniotomy for excision of the entire abscess and capsule is more effective than aspiration. An essential factor in recurrence is the retention of the capsule, so performing a craniotomy to clear both abscess and capsule altogether will avoid it.10 It is important to mention that surgical excision is indicated only when the lesion is located in the non-eloquent brain area. If the lesion is found in the eloquent area, aspiration and drainage are recommended.
4 CONCLUSION
Nocardiosis is a rare bacterial infection and is widely unknown in our country; it requires applied microbiology laboratory techniques to establish its diagnosis in order to provide a specific treatment. The differential diagnosis approach is challenging as this pathology is often confused with other infectious processes that affect the central nervous system.
It has a high incidence among immunocompromised patients in endemic regions and is prone to be misdiagnosed, similar to Tuberculosis.
Unfortunately, compared to the patients in the few previously published studies, this patient had a poor response to antibiotics, resulting in a fatal outcome.
AUTHOR CONTRIBUTIONS
Andrea Emilia Mawyin Juez: Investigation. Jorge Andrés Calderon Navas: Resources. Andrés Santiago Ronquillo Piloso: Conceptualization. Fernando Raul Salazar Reinoso: Supervision; writing – original draft. Gioconda Stefania Romero-Santana: Writing – review and editing.
ACKNOWLEDGMENT
The authors thank Dr. Raul Romero, Dra. Jessica Navas, and Dra Karla Wellington for their valuable contributions to the editing of this paper. Responsibility for any errors remains with the authors. This case and its outcomes are published with the written consent of the patient for educational purposes.
FUNDING INFORMATION
The author(s) received no financial support for the research, authorship, and/or publication of this article.
CONFLICT OF INTEREST
The author reports no conflicts of interest in this work.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy. A copy of the written consent is available for review by the editor in chief of this journal on request.
Open Research
DATA AVAILABILITY STATEMENT
All the findings are present within the manuscript.


