Surgical management of severe pediatric blunt abdominal trauma
Abstract
A 3-year-old male patient was brought to the Emergency Department with a traumatic blunt lesion in the liver. Due to hemodynamic instability and a severe lesion of a grade IV liver injury shown on the CT, the chosen conduct was to perform a hepatorrhaphy with oxidized cellulose.
1 INTRODUCTION
Traumatic injuries are responsible for 10%–15% of hospitalizations in pediatric units and pediatric intensive care units.1 Although traumatic brain injury is the most frequent traumatic lesion in the pediatric population, traumatic liver injury has a higher mortality. Traumatic lesions are the leading cause of death among children and adolescents in the United States, accounting for 30% of all deaths in this age group.2 Traumatic liver injury reflects in 5% of traumatic lesions seen in pediatric emergency department.3
The American Association for the Surgery of Trauma classifies liver trauma in six grades, from a mild lesion (hematoma or laceration) in grade I to severe hepatic lesions in grade IV to hepatic avulsions in grade VI. Lesions in grades I to III are the most frequent and are usually treated with conservative approach.4 Grade IV lesions are in the transition point from moderate to severe, and their management is controversial.5 While conservative management is a valid option, the decision of whether to undertake surgery is challenging for pediatric surgeons in emergency units. This paper reports an illustrative case of surgical management of grade IV pediatric liver injury with focus on the difficulty to decide the surgical plan.
2 CASE REPORT
We report a case of a 3-year-old male patient previously healthy with a history of traumatic blunt lesion who was brought to the emergency department after 5 h of the incident. The mechanism of trauma was the falling off a running machine on the abdomen.
Upon admission, the Glasgow Coma Scale was 15/15, heart rate was 120 bpm, and blood pressure was 85/45 mmHg, without external lesions.
Focused Assessment Sonography for Trauma (FAST) evaluation of blunt abdominal trauma: Absence of pericardial effusion. Presence of free liquid in the hepatorenal space, 3.6 cm of thickness. Presence of free liquid in the splenorenal space, 1.0 cm of thickness. Presence of free liquid in the pelvis, 2.5 cm of thickness.
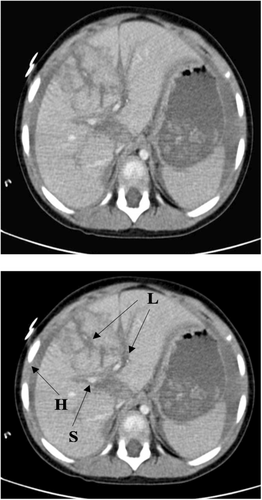
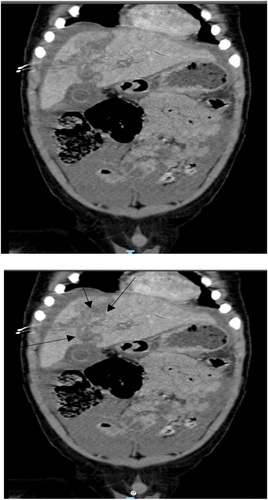
Whole body computed tomography: brain, cervical spine, and chest without any apparent traumas. Abdomen and pelvis: Liver showing extensive traumatic laceration (grade IV), involving segments IV, V, and VIII extending to the hilar region, with signs of active bleeding and a large amount of blood in the peritoneal cavity (Figures 1 and 2).
Laboratory examination at admission: Hemoglobin- 8.4 g/dL; Hematocrit- 24.9%; White blood cells- 24.3.000 mm3; Platelets- 254,000 mm3; Urea- 34 mg/dL; Creatinine- 0.6 mg/dL; Amylase- 67 U/L; Amino aspartate transferase- 643 U/L; Alanine amino transferase- 454 U/L; Prothrombin time- 11.2 s; Partial thromboplastin time- 19.6 s; Activity- 95%; INR- 1.
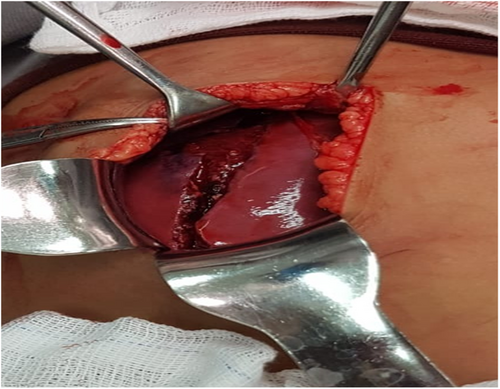
Given the patient's clinical condition and findings upon examination, the exploratory laparotomy was performed. Approximately 800 ml of blood was aspirated from the abdominal cavity. Hematoma and active bleeding were identified during laceration between lobes IV, V, and VI. Hepatorrhaphy was conducted using oxidized cellulose in a laceration path (Figures 3 and 4). The hepatic hilum, the spleen, the small intestine, and the colon were intact, and a Penrose drain was allocated into the hepatic bed. The patient was stable during surgery and was transfused with 400 ml of packed red blood cells. They were immediately referred to the post-operative intensive care unit (ICU).

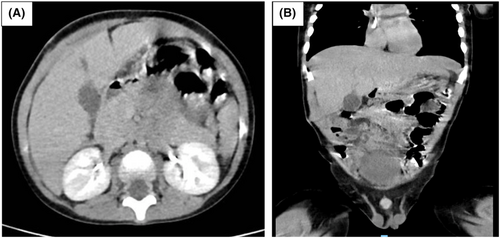
The post-operative evolution in the ICU and infirmary did not have any complications, and further blood transfusion was not necessary. The drain had 50 ml of serous liquid (total bilirubin—8.9; direct bilirubin—4.9; indirect bilirubin—4). A CT scan was performed and did not shown any complications on the 14th day post operation (Figure 5), and the patient was discharged on the same day.
Laboratory examinations at discharge was Hemoglobin: 11.3 g/dL; Hematocrit: 38%; White blood cells: 9000mm3; Platelets: 275,000 mm3; Urea: 24 mg/dL; Creatinine: 0.6 mg/dL; Amylase: 45/U/L; Amino aspartate transferase: 38 U/L; Alanine amino transferase: 40 U/L.
3 DISCUSSION
Deciding whether to pursue to a conservative or surgical approach in cases of blunt abdominal trauma in children remains a challenge. Although there is clear a evidence that conservative treatment reduces morbidity and mortality, the decision to undergo surgery requires multidisciplinary experience from the surgical team, emergency services, Intensive Care Units and hospital transport services, as well as the use of tools such as the American Trauma Surgery Association's scale for grading the severity of liver injuries.
Liver trauma is conservatively treated in 70%–80% of the cases, with no increased risk of mortality.6 Surgical treatment occurs in 20% of the cases and aims to restore physiology and hemostasis with essential resections and temporary stomas (damage control surgery).6
Evaluating abdominal trauma with imaging (FAST, CT scan)7 on admission is important to detect and grade liver injuries with a high sensitivity and specificity. The literature reports ultrasound with a sensitivity between 69% and 99% and specificity between 86% and 100%. The isolated sensitivity for hemoperitoneum diagnosis is as high as 91%–94%.8, 9 The sensitivity and specificity for computed tomography are above 97%.8 In addition to laboratory tests, the child's hemodynamic status complemented the treatment decision.
Bleeding control techniques are employed in cases where there is no severe bleeding during laparotomy. The bleeding can be controlled by isolated compression, cauterization, organic bundle coagulation, topical hemostatic agents, or omentum tamponade. In the presence of intense hemorrhage, more aggressive procedures, such as manual compression, hepatic packaging, or hepatic vascular exclusion, may be necessary.4
In this case, due to the blunt abdominal trauma with extensive hepatic laceration and evidence of active hemorrhage on tomography the trauma was assorted as a grade IV liver injury. We performed hepatorrhaphy with oxidized cellulose in laceration, which have shown to have good results in the hemostasis.9
In cases of liver trauma with intrahepatic bile duct lesions, the priority of the surgeon is to control the bleeding and the leakage of bile through the lesion, which is often self-limiting.10 In our case, the patient had minimal biliary drainage through the drain left in the liver bed, which resolved spontaneously after 72 hours post-operative.
4 CONCLUSION
Surgical treatment of liver trauma consists of bleeding control. Therefore, it is important to choose a surgical method and material that is easy for the team to handle in order to achieve hemostasis, while avoiding complications such as acidosis, coagulation disorder, and hypothermia, that can be fatal to the patient.
AUTHOR CONTRIBUTIONS
Adilson Vidal: Conceptualization; data curation; investigation; methodology; writing – review and editing. Adilson Oliveira: Conceptualization; formal analysis; project administration; supervision; validation. Thais Rossi: Conceptualization; data curation; formal analysis; investigation; methodology; writing – original draft. Bruna de Carvalho: Conceptualization; data curation; investigation; methodology; writing – original draft. Melissa Volpiani: Conceptualization; data curation; investigation; methodology; writing – original draft. Max Scholobach: Conceptualization; data curation; formal analysis; investigation; methodology; validation; visualization; writing – original draft. Fabio Peterlini: Conceptualization; data curation; formal analysis; investigation; methodology; visualization; writing – original draft. Rhuan Silva: Data curation; project administration; writing – original draft; writing – review and editing. Felipe Nascimento: Data curation; methodology; writing – original draft; writing – review and editing. Edna Gouveia: Formal analysis; methodology; writing – original draft.
ACKNOWLEDGMENT
None.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
None.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the Journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




