Peutz–Jeghers syndrome revealed by recurrent small bowel intussusceptions in children: A case report
Abstract
Peutz–Jeghers syndrome is a rare but potentially life-threating syndrome. We report here the case of a young girl who presented recurrent small bowel intussusceptions. Laparotomy exploration showed many jejunal polyps leading to jejunojejunal intussusceptions. These were removed via mini enterotomies and pathological examination concluded to Peutz–Jeghers polyps.
1 INTRODUCTION
Peutz–Jeghers syndrome (PJS) is a rare but well-described inherited disease, characterized by specific pigmented freckle-like mucocutaneous lesions, and gastrointestinal and extra gastrointestinal hamartomatous polyps. The most common and concerning manifestation in children and adolescents is the occurrence of small bowel intussusception, which could represent a serious surgical emergency and be life-threatening.1, 2
We report in this paper the case of recurrent intestinal intussusceptions in a child, resulting of hamartomatous Peutz–Jeghers polyps. Our aim was to remind diagnostic and management particularities of this unusual condition and to highlight the importance of regular follow-up for these patients to avoid complications.
2 OBSERVATION
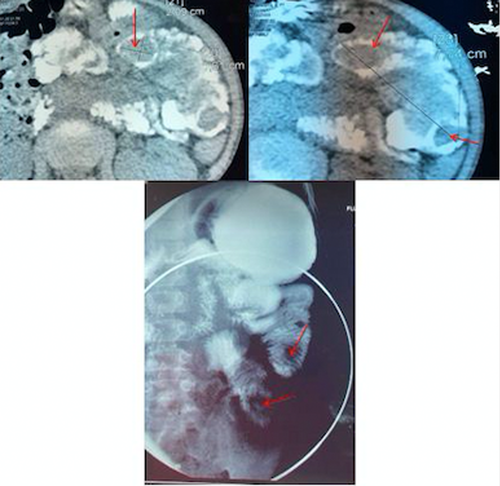
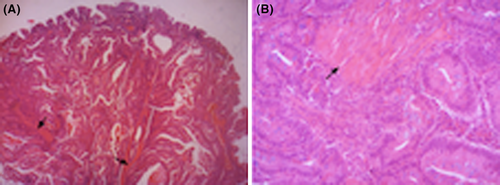
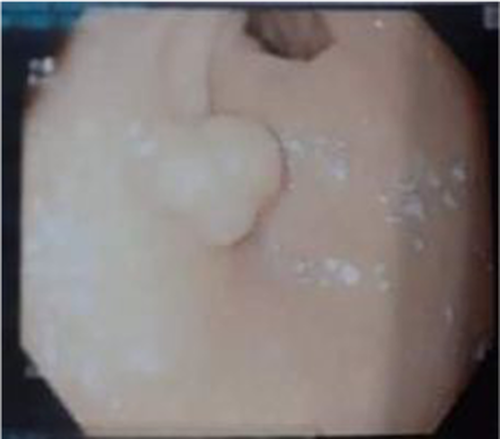
An 8-year-old girl presented to the emergency department of our hospital with recurrent abdominal pain and vomiting, which were suddenly worsened. She had no family history of gastrointestinal pathologies. Upon presentation, the patient had good vital signs. Physical examination showed dark pigmentations of the buccal mucosa (Figure 1) and epigastric tenderness on palpation. Abdominal ultrasound (US) revealed extensive small bowel intussusception. Then, the patient underwent emergent laparoscopic exploration and successful intussusception reduction. One month later, she had once again the same symptoms with recurrence of the small bowel intussusception at US. An abdominal CT scan associated with upper gastrointestinal series was performed showing polypoid lesions inside the intestinal lumen (Figure 2). Laparotomy exploration was achieved to our patient through an upper midline incision. We found and reduced the small bowel intussusception. Then, the whole intestine was checked, permitting the identification at the jejunum wall of multiple intraluminal polypoid formations with a biggest of 3 cm of diameter (Figure 3), which were totally removed through limited enterotomies. Bowel resection was not needed. Pathological examination of the specimens confirmed hamartomas with smooth muscle arborization, compatible with Peutz–Jeghers polyps, without malignancy signs (Figure 4). The postoperative course was uneventful. The patient was then referred to gastrologist for further exploration. Esophago-gastroduodenoscopy revealed two sessile polyps in the stomach, 5 and 12 mm of diameter, which were endoscopically removed. Colonoscopy disclosed only one sessile polyp of 6 mm (Figure 5).

3 DISCUSSION
Peutz–Jeghers syndrome (PJS) was first defined by Peutz in 1921 and Jeghers in 1944, as a familial autosomal dominant disorder, characterized by hamartomatous polyps of the gastrointestinal tract, and specific mucocutaneous hyperpigmentations.3-6 It is an extremely rare disease, with an incidence of 1 in 12–30,000 live births,2, 7, 8 and whose pathogenesis has been related to a germline mutation on the serine/threonine kinase 11 (STK11/LKB1) tumor suppressor gene on chromosome 19p13.3.9
Despite its rarity, PJS has become a well-known entity with specific diagnostic criteria,1, 10, 11 which are both clinical and histological. Recently, Beggs et al proposed to consider the diagnosis in presence of (1) two or more histologically confirmed PJS polyps, or (2) any number of PJS polyps in an individual who has a family history of PJS in close relative(s), or (3) characteristic mucocutaneous pigmentation in an individual who has a family history of PJS in close relative(s), or (4) any number of PJS polyps in an individual who also has characteristic mucocutaneous pigmentation.12
Diagnosis of PJS was attributed to our patient according to the fourth Beggs' criteria, as she had multiple gastrointestinal PJ polyps associated with dark pigmented macula at the lip mucosa. PJ polyps are very characteristic due to their histologic features, looking like an unusual type of hamartomatous polyp. Microscopic aspect is characterized by a tree-like branching of smooth muscle fibers, with a core of smooth muscle arising from the muscularis mucosa and extending into the polyp, covered by mucosal tissue with near-normal appearance.9 Mucocutaneous pigmentations appearing with PJ-affected patients have also characterized aspect and location. They correspond to small, oval or circular and dark brown lentigines,1 and their most common locations are lip and buccal mucosae.
Our patient presented to the emergency department with recurrent abdominal pain and vomiting which suddenly worsened, likely due to intermittent small bowel intussusceptions. According to literature data, such symptoms are mostly caused by polyp-related complications and often represent the discovery circumstance of PJS in children.10, 13-15 This is certainly due to anatomical characteristics of these polyps. In a large multicenter study, Van Lier et al. reported a cumulative intussusception risk in PJS of 15% by age 10 years and 50% by age 20.16, 17 They also concluded that PJ polyps depend on small bowel in more than 95% of cases, the jejunum being the preferential location, which may act as leading point for the intussusceptions. Moreover, polyp-size was probably an important risk factor for small bowel intussusception, as they were generally caused by hamartomas larger than or equal to 15 mm in diameter.17 In our case, the recurrent aspect of intussusceptions, their jejuna location on US, and presence of dark macula at the lip mucosa led us to suspect the presence of underlying lead point, in particular PJ polyps. That is why we investigated further using abdominal CT scan and upper gastrointestinal series permitting the identification of polypoid lesions inside the jejuna lumen. Referring to the literature, PJ polyps are often detected in US, barium studies, CT enterography, and MR enterography which has the advantage of a lack of ionizing radiation. The sensitivity of video capsule endoscopy (VCE) has also been demonstrated even for detection of small polyps, but it cannot be used in the presence of intestinal obstruction.18, 19
For our patient, all intussusceptions depended on small bowel and were successfully reduced through open surgical approach. For polyps' identification, we checked and palpated the whole intestine wall. They then were entirely removed by small elective enterotomies without need of resection. In a large series, C.Fallon et al demonstrated that children with a lead point such as polyps have increased risk of requiring surgery.20 According to the latest European Hereditary Tumor Group (EHTG) guidelines, laparotomy is the safest option for the surgical treatment of intussusception secondary to PJS. Then, the preferred strategy is the manual reduction, if possible, followed by resection of the polyp that acts as a hypomochlion at its base by enterotomy, without bowel resection. Moreover, entire small bowel should be critically checked by palpation or intraoperative enteroscopy through enterotomy is recommended to find and remove over 15 mm size polyps.10 Laparoscopic approach was also showed to be feasible and efficient in these cases, but should better be combined with upper/lower endoscopy to avoid multiple surgical interventions.10, 13, 21
In general, the gravity of PJS is related to two major complications: small bowel intussusception, with its urgent and even life-threatening character especially in children, and the increased risk of malignancy at adulthood. Several meta-analysis and cohort studies have demonstrated that this risk varies between 55% and 85%.10 That's why patients with confirmed PJS must have regular and periodic surveillance.1, 10
Based on the reviewed literature, recommendations and statements were formulated on clinical genetic, gastrointestinal, surgical, pancreatic, breast, and gynecological management.10
As PJS is inherited in an autosomal dominant pattern, genetic germline screening of the STK11gene is recommended for asymptomatic at-risk children, before onset of symptoms, and for symptomatic patients meeting the clinical PJS criteria, and this regardless age. However, diagnosis of PJS should be considered in presence of clinical criteria, even if an underlying causative germline variant is not identified, because of the important genetic heterogeneity.1, 10
Based on recent recommendations of the European Society of Gastrointestinal Endoscopy, gastrointestinal surveillance should be initiated no later than 8 years in an asymptomatic individual with PJS, and earlier if symptomatic. These investigations include oeso-gastro-duodenoscopy, colonoscopy, and MRI studies or video capsule enteroscopy for the small bowel, and should generally be repeated at least every 3 years. Then, elective polypectomy should be performed for small bowel polyps up to 15–20 mm of diameter, to prevent intussusception.1, 10, 12 Similarly, we have begun a gastrointestinal surveillance program for our patient. She undertook an initial esophago-gastroduodenoscopy and a colonoscopy revealing one colonic and two gastric polyps which were safely removed by endoscopy.
Moreover, according to the American College of Gastroenterology and the EHTG guidelines, adults with PJS should undergo an annual complete blood cell count with physical examination including evaluation of the abdomen, pelvis, breasts, and testes. Lifelong cancer surveillance is recommended, in order to early detect pancreatic, testes, breast, and gynecological tumors.3, 10
4 CONCLUSION
Although PJ polyps are unusual in children, they should be considered as a potential pathological lead points in case of recurrent jejunal intussusceptions, especially in presence of characteristic dark muco-cutaneous macula, or familial history. Besides the risk of serious gastrointestinal polyp-related complications, PJS is associated with an increased risk of cancers. Early identification of this condition is then important for symptomatic or at-risk patients, as it permits to establish a strict and regular systemic surveillance program, which can considerably improve quality of life and prognosis of these individuals.
AUTHOR CONTRIBUTIONS
Chtourou Rahma conceived the idea of the document and contributed to the writing of the manuscript. Ben Kraiem Najoua, Mellouli Manel, Zouari Mohamed, and Dghaies Rim contributed to the literature review and the writing of the manuscript. Ben Dhaou Mahdi, Sellami Boudawara Tahya, and Mhiri Riadh reviewed the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
This work was made and published with the consent of the patients.
CONFLICT OF INTEREST
None declared.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




