Benign or premalignant? Idiopathic granulomatous mastitis later diagnosed as ductal carcinoma breast cancer: Case report and review of literature
Abstract
Idiopathic granulomatous mastitis (IGM) is a rare benign infectious disease of the breast, commonly presenting with a unilateral breast mass. Since GM's clinical presentation and imaging can be very similar to breast cancer, diagnosing GM can be challenging. So far, various reports have demonstrated the probable correlation and co-occurrence of granulomatous mastitis and breast cancer. This report presents a 38-year-old female with invasive ductal carcinoma, previously diagnosed as IGM.
1 INTRODUCTION
Idiopathic granulomatous mastitis (IGM), first defined in 1972 by Kessler and Wolloch,1 is a rare benign disease of the breast, commonly exhibiting unilateral breast mass, nipple discharge, hyperemia, and edema.2 In addition, since the clinical presentation and imaging of GM can be very similar to breast cancer, the diagnosis of GM can be very challenging.3 Furthermore, the management of GM is mainly non-invasive, while patients with breast cancer require more invasive therapies such as surgery and chemotherapy. In this regard, the misdiagnosis of GM can result in unnecessary interventions or delayed treatments.
The exact etiology of granulomatous mastitis is still unclear. Nevertheless, it is assumed that some factors such as trauma, infectious (e.g., tuberculosis), and autoimmune responses (such as granulomatosis with polyangiitis and giant cell arteritis) may be involved in the pathogenesis of GM.4 In this regard, elevated levels of progesterone and estrogen are assumed to be associated with the pathogenesis of GM. As a result, most cases of GM are women of reproductive ages, precisely postpartum or breastfeeding periods.
Previous studies indicated that there might be a possible association between breast cancer and GM.5 In a study, Handley6 demonstrated that three out of five sisters with chronic mastitis developed breast cancer during the follow-up.6 Also, various studies have reported the concurrence of GM and breast cancer in the same and contralateral breasts.7 In the current study, we present a case of idiopathic granulomatous mastitis later diagnosed as ductal carcinoma breast cancer. Needless to say, considering the low prevalence of GM, such reports may shed light on the pathology of GM and its ideal management.
2 CASE PRESENTATION
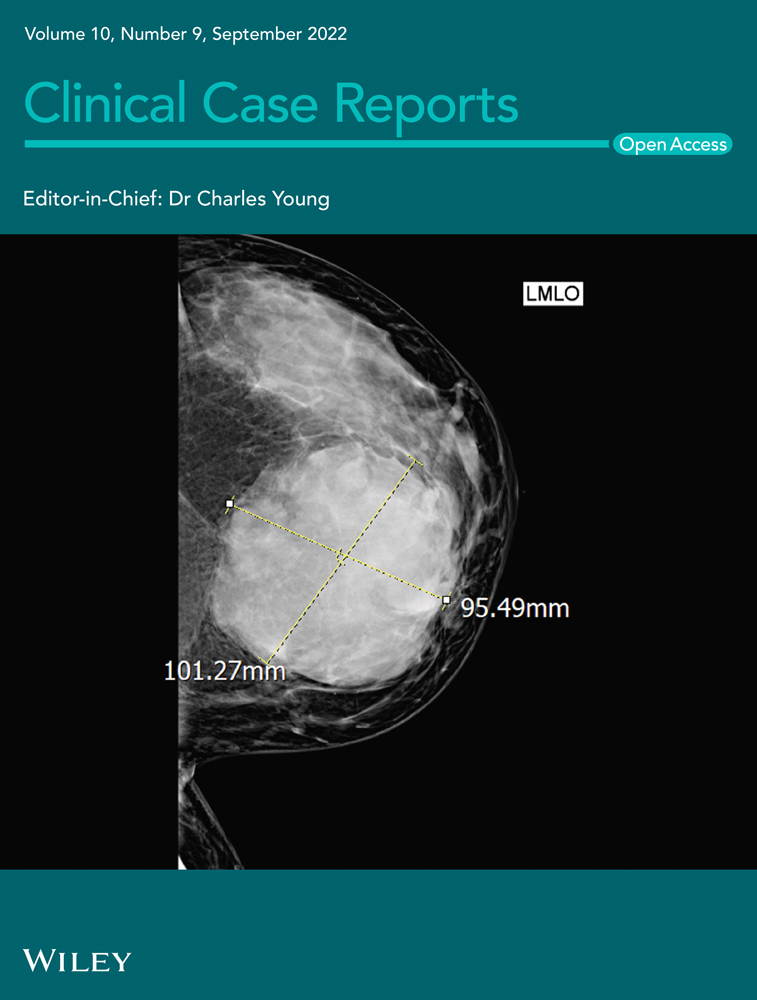
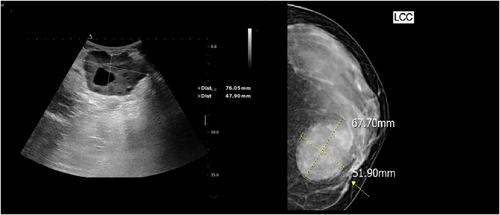
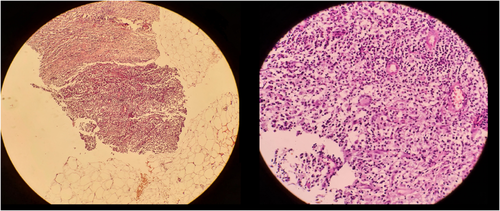
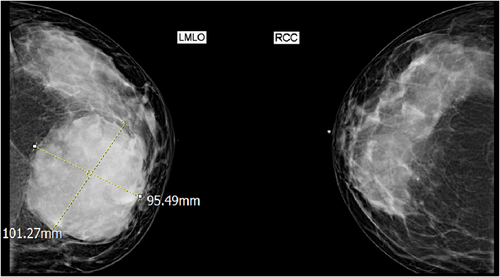
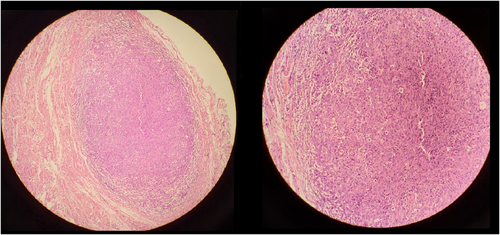
A 38-year-old pre-menopausal female patient was referred to our clinic complaining of a left breast mass. The past medical history was unremarkable except for a palpable mass in the same breast a year previously, which was diagnosed as IGM in pathological assessments through trucut biopsy (Figures 1, 2). It should be noted that our patient had a negative acid-fast stain for mycobacteria. Also, the polymerase chain reaction assessments detected no evidence of a mycobacterial genome. One year ago, she was treated with prednisolone and methotrexate, which exhibited a good response to treatment. During the first 6 months of the treatment, the size of the mass and inflammation decreased.
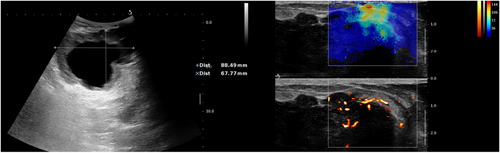
Furthermore, the mass was stable for 3 months with weekly methotrexate and a low prednisolone dose. After that, the tumor increased in size and erythema. Considering the possible relapse of IGM, a high dose of prednisolone was initiated. During the follow-up, she had an inadequate response to treatment, and in the last examination, left axillary lymphadenopathy was detected. In this regard, the patient was referred for a re-evaluation, investigating the poor response to treatment and axillary lymphadenopathy (Figures 3-5).
3 DISCUSSION
IGM is a rare, benign, and chronic inflammatory disease of the breast, typically occurring in postpartum or breastfeeding women.9 In addition, IGM can clinically and radiographically imitate breast cancers; therefore, the diagnosis of IGM should be confirmed based on pathologic investigations.10 In this regard, since the management of IGM considerably differs from breast cancer management, the distinction between these two diseases is crucial.11 In this regard, studies suggested that evaluating some inflammatory markers such as interleukin-33 or circulating tumor markers (e.g., PTEN, miR-155, let-7c, and miR-21 levels) may help the differentiation of these two diseases.12, 13
As mentioned earlier in the manuscript, the possible association between chronic mastitis and breast cancer was first indicated in a report by Handley in 1938.6 Similarly, in a report by Mazlan et al.14 in 2012, they presented a case of a 34-year-old female with recurrent experiencing right breast swelling and abscess. This patient was diagnosed as GM in various biopsies. In addition, she responded to antibiotics and corticosteroid therapy. Nevertheless, later the patient developed a distant metastasis of breast infiltrating ductal carcinoma in the brain.14
In another study in 2013, Limaiem et al. reported a 77-year-old female complaining of right breast pain, which was diagnosed as ductal carcinoma concomitant with granulomatous lobular mastitis. To the authors' knowledge, four cases of concurrent GM and ductal carcinoma have been reported in the literature.5, 15-17 Also, two cases of GM and breast cancer in contralateral breasts have been reported.7, 18 Of these two cases, one patient had ductal carcinoma, and the other had multifocal breast cancer. A comprehensive literature review of previous reports regarding the GM and breast cancer is provided in Table 1.
| First author | Year | Age | Initial chief complaint | Remarkable past medical history | Description |
|---|---|---|---|---|---|
| Handley6 | 1938 | 54–45-41 (in order) | Mastalgia-mastalgia-painless mass | None-none-history of contralateral breast carcinoma | None |
| Mazlan14 | 2012 | 34 | Breast swelling and abscess | Repeated course of breast abscess | A case of chronic GM, which was later developed brain metastasis and turned out to be infiltrating ductal carcinoma |
| Limaiem15 | 2013 | 77 | Mastalgia | Hypertension and epilepsy | Concurrent grade II infiltrating ductal carcinoma and granulomatous lobular mastitis |
| Kaviani18 | 2017 | 48 | Bilateral large palpable masses | None | Invasive ductal carcinoma for the left breast lesion and IGM for the right breast |
| Çalış16 | 2017 | 77 | Mastalgia | None | Concurrent high grade ductal carcinoma in situ and granulomatous mastitis |
| Özşen5 | 2018 | 35 | Breast swelling | None | Concurrent granulomatous lobular mastitis and in situ ductal carcinoma |
| Oddó17 | 2019 | 44 | Breast swelling and painful mass | Coronary disease with myocardial infarction | Concurrent granulomatous lobular mastitis with coryneform bacteria and ductal carcinoma in situ |
| Evans7 | 2021 | 39 | Painless mass | Breast abscess | Right multifocal breast cancer and left granulomatous mastitis |
Similar to most patients with GM, our patient was of reproductive age. In addition, similar to the report of Mazlan et al.,14 our patient developed invasive ductal carcinoma 1 year after the diagnosis of GM. Nevertheless, the timely diagnosis prevented the possible metastases. In addition, since our patient responded to prednisolone, and the initial diagnosis was made through trucut biopsies, it is unlikely that the diagnosis was missed. Considering the limited evidence regarding the co-occurrence of GM and breast cancer, inevitably, such reports emphasize the importance of close monitoring and follow-ups in patients with GM for possible malignancy.
Although the role of chronic inflammation in developing Gastrointestinal cancers has been documented, it is still unclear whether chronic mastitis and GM predispose patients to breast cancers. In this regard, the excessive host response following chronic inflammation results in oxidative stress and its consequent structural and DNA damage.19 Additionally, several pathogeneses have been proposed for the role of chronic mastitis in the development of breast cancer, including disrupted microbiome and impaired extracellular matrix of the breast.20
Based on the reported cases and our patient, each breast lesion in patients with a history of IGM should be evaluated for possible breast malignancy. Also, in patients with IGM, it is essential to assess the collateral breast for suspicious lesions carefully. Furthermore, further studies on the possible association between chronic mastitis and breast cancer are encouraged.
AUTHOR CONTRIBUTIONS
VZ, HRN, and FH: conceptualized the data. HN, VZ, and HRN: curated the data. VZ & HRN: wrote the original draft. AR and MSS: edited the draft.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ETHICAL APPROVAL
Written informed consent was obtained from the patients prior to the publication.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
None.