Musculoskeletal pain in children, should we think about neuroblastoma?
Abstract
A 9-year-old girl with progressive right leg pain, distributed to the pelvis and lower spine, diminished muscle force, and tendon reflex, was worked up thoroughly. Thoracolumbar MRI showed a well-circumscribed homogenous enhanced extradural mass from L3-L4 to S1. After surgery, a firm extradural mass was resected, and the pathologic finding was a neuroblastoma.
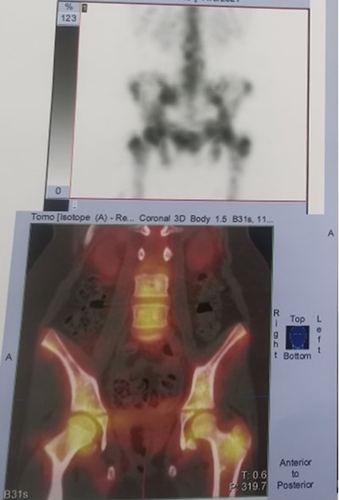
A 9-year-old girl was admitted to our center with only progressive right lower extremity pain from 1 month ago, distributed to the pelvis and lower spine. The patient's pain did not respond to analgesics. She had a history of sudden urinary retention and falling. The positive findings in the physical examination were inability to walk because of pain and reduced muscle force (4/5), diminished deep tendon reflex on the right leg, and tenderness over the lower spinal column. Routine laboratory exams showed no abnormality. Pelvic and thigh X-ray (Figure 1) demonstrated a suspicious diffuse infiltrative lesion in the bony pelvis. Therefore, bone marrow aspiration and biopsy were done, and the result was normal with <1% blast. EMG and NCV revealed bilateral asymmetrical muscle weakness and neuropathy in the L5 and S1 dermatomal areas. A whole-body bone scan suggested diffuse infiltrative skeletal involvement (Figure 2). Thoracolumbar MRI (Figure 3A,B) revealed a well-circumscribed homogenous enhanced extradural mass from L3-L4 to the upper third of S1, in favor of neurofibroma-schwannoma and less likely PNET (primitive neuroectodermal tumors) and lymphoma. The patient underwent surgery, and a firm extradural mass was resected from the area. The pathologic finding was consistent with a high-grade small round cell tumor (Figure 4). After immunohistochemical staining, the sample was positive for synaptophysin, chromogranin, CD 56, S-100, and Ki-67 in about 20%–25% of tumor cells and this IHC panel was supportive of neuroblastoma.


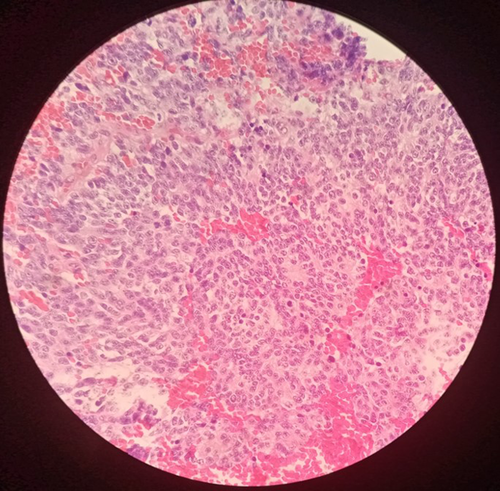
Neuroblastoma as part of small round blue cell tumors is a highly aggressive malignancy that could derive from anywhere in the sympathetic nervous system, including the adrenal gland or in sympathetic ganglia.1 These tumors are often accompanied by changes in blood cell counts or acute phase reactants. But we could not find any laboratory abnormality in our patient.2
AUTHOR CONTRIBUTIONS
PS is the corresponding author and a part of the patient's management team. ZH operated on the patient, and VZ was the patient's management team supervisor. All authors contributed to the article and approved the submitted version.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST
The authors have no conflict of interest.
CONSENT
Written informed consent was obtained from the patient's parents to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Requests for access to the data that support this report should be made to the corresponding author.




