Pseudoangiomatous stromal hyperplasia of the breast: A case report
Abstract
Pseudoangiomatous stromal hyperplasia (PASH) is a rare benign breast entity scarcely reported in the medical literature. Its pathogenesis, etiology, and optimal treatment are still unknown. PASH tumors have a broad spectrum of clinical presentations and might be mistaken for malignancies. The authors present six patients diagnosed with PASH.
1 INTRODUCTION
Pseudoangiomatous stromal hyperplasia (PASH) is a rare benign breast lesion, first described in 1968 by Vuich et al.1 It is defined as a mesenchymal proliferation of myofibroblasts of the breast, which can be misdiagnosed as low-grade angiosarcoma or phyllodes tumor.2 PASH has a broad spectrum of clinical presentation, ranging from an incidental microscopic finding accompanying other breast lesions to a fast-growing palpable mass.3 It's mostly found in perimenopausal women.4 The optimal treatment for PASH tumor is still controversial due to its rarity.
In this case series, we presented six cases of PASH. Data for this study were collected retrospectively from patients' files, in Shiraz Breast Diseases Research Center (SBDRC) database. Inclusion criteria were definite pathological diagnosis of PASH, and presence of treatment outcome in patient's documents.
2 CASE 1
A 41-year-old multiparous female came to our breast clinic, complaining about rapidly growing asymmetric bilateral breast enlargement. In physical examinations, multiple soft mobile lumps with thickened and erythematous overlying skin were detected in both breasts. The radiographic evaluations were suggestive of benign solid masses. She was diagnosed with a fibroepithelial lesion in tru-cut biopsy and underwent bilateral excision. Pathology report indicated PASH in left tail mass (12 × 11 × 5 cm) and in lower part, and benign phyllodes at 7 o′clock and 12 o′clock position of the right breast.
She underwent bilateral breast resection one month later (due to discomfort). There were multiple well-defined masses with homogenous and creamy surface in both breasts, suggestive of fibroadenoma with PASH (Largest: Left: 6 × 5 × 3 cm & Right: 4.5 × 4 × 3 cm). After 3 months and one episode of hospitalization due to breast cellulitis and receiving IV antibiotics, the patient underwent a bilateral simple mastectomy due to the high probability of angiosarcoma. In the pathology of right breast, fibroadenoma with fibrocystic disease and PASH were reported, and on the left side, benign phyllodes with fibrocystic disease and PASH were reported. After one year, she came with an 8 × 7 × 4 cm mass in her abdomen (Figure 1). She underwent local excision and pathological assessments revealed ectopic mammary breast tissue with PASH. She has been symptom-free in further follow-ups till the day this report was conducted.

3 CASE 2
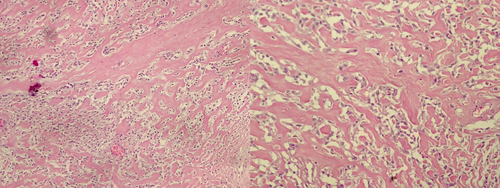
A 30-year-old primigravida woman, breastfeeding for one year, came with a palpable mass in her right breast. She underwent FNA and was diagnosed with Sclerosing adenosis with band-like adenosis. The mass was resected. Four months later due to enlargement of the right breast, ultrasonography was done, and an elliptical hypoechoic focus (65 × 20 mm) at 7 o'clock of the right breast with thin capsule and lateral shadowing was revealed (U-BIRADS 3). Two months later, due to recurrence, following resection of the mass, she was diagnosed with PASH (Figure 2). She has not developed any related symptoms till the day this report was conducted.
4 CASE 3
A 51-year-old multigravida woman came with an enlargement of the left breast. In radiologic evaluation, one large mass in the lateral aspect of the left breast was detected, involving a sub-areolar region composed of multiple masses packed together in conjugate with multiple lesions (180 mm largest diameter) (BIRADS 4). Pathology reported benign fibroadenoma. Every six months patient was visited, and mass was growing fast. So, tru-cut biopsy was done and PASH was confirmed by immunohistochemistry (IHC). There was no sign of recurrence in further follow-ups.
5 CASE 4
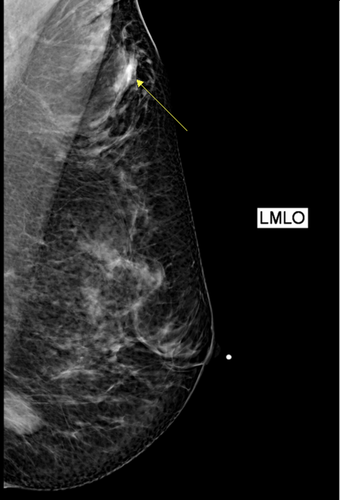
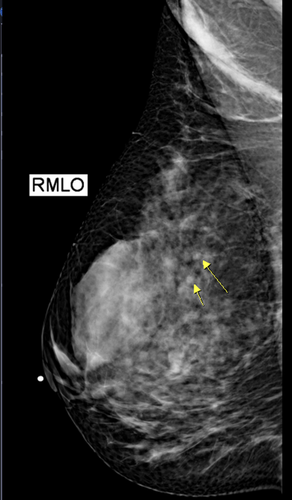
A mass was detected incidentally in the right breast of a 36-year-old single lady in routine examinations. Radiologic studies showed a 44 × 16 mm sharp border hypoechoic mass at 10 ‘o clock position of the right breast (Figures 3, 4). Due to the COVID-19 pandemic, excision was postponed. Five months later in mammography, two sharp border hypoechoic lesions were detected; one, 49 × 19 mm in the upper outer of right breast, the other, 31 × 7 mm in the lower part of left breast, both in favor of fibroadenoma. One month later, the patient underwent bilateral excision. Pathology reported fibroadenoma with PASH.
6 CASE 5
A 12-year-old girl with unilateral left breast enlargement was referred to this center. She has had a growing lesion since she was nine years old. (BIRADS 3) In radiologic studies, the lesion was introduced as a congenital problem with edema. The possibility of Lymphoma could not be rolled out. There was no sign of abnormality in any of the axillary areas. Later, she underwent an incisional biopsy and was diagnosed with PASH. Left simple mastectomy with tissue expansion was done for her. One month later, she was admitted again to undergo reconstruction surgery, but the operation was canceled due to lack of equipment. Five months later, she developed right breast enlargement. She was admitted to the surgery ward and underwent right breast excisional biopsy and left breast prosthesis insertion without mess graft. Pathology reported PASH. Two weeks later, she underwent right breast areola sparing mastectomy, mastopexy with prosthesis insertion. The patient did not develop any further signs or symptoms in later follow-ups.
7 CASE 6
A 25-year-old married woman, with a history of two pregnancies, was referred to our clinic with left breast enlargement. The lesion was excised and in the histologic evaluation, fibrocystic changes were reported. Four years later, she was visited again due to the recurrence of left breast mass. Tru-cut biopsy was done, and fibrocystic changes were reported. After three years, she was referred to our clinic again, due to recurrence of left breast lesion. The lesion was excised, and she was diagnosed with PASH. Later, she underwent left quadrantectomy. She has been fine till the day this report was conducted.
8 DISCUSSION
Pseudoangiomatous stromal hyperplasia (PASH) is rarely reported in the medical literature. Consequently, its etiology and optimal treatment are still controversial. Our patients, presented with different clinical manifestations. Considering previous studies on this matter, we performed Tru-cut biopsy and resection, respectively, for diagnosis and treatment of our patients. Treatment results were satisfactory.
PASH tumors are known to have a wide spectrum of clinical presentations, as reported in previous studies. Non-tumor-forming PASH is rather more common than tumor-forming type. The former is an incidental finding that is mostly identified in histologic studies alongside other breast lesions. However, there are a few reports of PASH presenting as considerable breast enlargement. Abdelrahman et al. reported 35 cm breast enlargement in a 13-year-old female which was later diagnosed as PASH tumor.5 In Koksal et al.’s study, a 13-year-old girl was reported, with a giant mass in her left breast.6 In another report by Willy et al., PASH presented as extreme gigantomastia in a 29-year-old woman.7 PASH tumors rarely mimic clinical presentations of malignant breast entities. In our cases, there were no extremes regarding lesions' size and each case went through a different disease course.
Radiologic findings have been repeatedly reported to be non-specific in differentiating PASH,7, 8 In Raj et al.’s study, radiologic features of PASH are reported to be diverse and in some cases, similar to fibroadenoma.8 In Raza et al.’s study, a 29-year-old lactating woman, presented with a huge firm mass in her left breast and palpable left axillary lymph nodes.9 In various radiologic studies, she was diagnosed with breast malignancy. However, later histopathology results revealed PASH.
In Nia et al.’s study, 69 patients were diagnosed with PASH in histologic studies.10 They all underwent magnetic resonance imaging (MRI)-guided biopsy analysis. PASH was an incidental finding in all cases, accompanying other breast lesions. Later, authors concluded PASH tumors might have a wide range of features in MRI, and thus, this confirms why they are usually incidental findings. According to this study's results, a region of non-mass enhancement with persistent kinetic features seems to be the most common appearance of PASH in MRI studies. In our cases, imaging results were non-specific.
Core needle biopsy (CNB) is the most acceptable and sufficient procedure till this day to confirm the diagnosis of PASH in a suspicious imaging.4 Histologically, PASH is defined as a benign proliferation of stromal myofibroblasts. It was thought to be a type of breast hamartoma.11 In histologic evaluations, PASH might be mistaken for low-grade angiosarcoma and, IHC is needed for differentiation. Initially, the nature of our first and fifth case breast enlargement could not be specified in radiologic evaluations. In the first case, angiosarcoma could not be ruled out, and consequently, she underwent a bilateral simple mastectomy. Later, in histologic assessments followed by IHC, she was diagnosed with PASH. In the fifth case, lymphoma could not be ruled out in radiologic evaluations, and she was diagnosed with PASH in histologic assessment. In the other four cases, the possibility of malignancy was relatively low.
PASH is more prevalent and more likely to occur in hormonally active women,4, 8 Few male cases have been reported. As in Bowman et al.’s study, they reported two male cases; one was accompanied by gynecomastia, and the other related to hormonal therapy in a transgender male.12
The treatment of PASH tumor depends on the size and growth rate of it. Surgical and non-surgical treatments have been both successfully applied in previous studies. Generally, removing the tumor with minimized damage to the breast is currently agreed upon in medical literature. Considering the role of hormones in the etiology of PASH, anti-hormonal therapy can be a non-invasive treatment alternative. Pain management might be needed according to patient's condition. Thus, it mostly depends on the surgeon to observe the patient's condition and choose the best treatment accordingly. In Yoon et al.’s study, the preferred management of large tumors (>3 cm) or progressively growing tumors was surgical removal or close observation of lesions and deciding accordingly.4 Koksal et al. removed the lesion surgically and in six-month follow-up, no recurrence happened.6 Raj et al. preferred surgery, especially in patients with large tumors and higher risks for breast malignancies.8 Raza et al. treated their patient conservatively.9 Kurt et al. recommended excision, especially for lesions with suspicious features.13 In our cases, we surgically removed the lesions in each case.
There is no evidence of PASH tumors turning into malignant lesions. In Degnim et al.’s study, biopsy-proven PASH cases, with mean of 18.5 years of follow-up, showed a lower incidence of breast malignancies compared with patients with other benign breast lesions.14 Also, compared with the general population, women with PASH tumors in this study did not show higher risks of breast cancer. We visited our patients every four months for two years and after that, once every year. None of our six cases developed with any breast malignancies in their later follow-ups.
9 CONCLUSION
PASH is an uncommon breast entity with diverse clinical presentation and non-specific radiologic features. Histologic assessment is needed for a definite diagnosis. Both surgical and non-surgical treatments have been reported to be effective. Optimal treatment of PASH tumors seems to be depending on patient's condition and surgeon's judgment. Although recurrence did happen among our cases, the overall rate was low. Follow-up visits after excision are recommended.
AUTHOR CONTRIBUTIONS
S.T was involved in patients treatment. M.GJ and A.K were involved in data preparation and in the draft writing. M.A,V.Z, and A.T revised the report, commented on drafts of the manuscript, and approved the final report.
ACKNOWLEDGMENTS
Authors would like to thank all staff members and personnel who aided in the collection of the data at the breast clinic.
FUNDING INFORMATION
This work was funded by Breast Diseases Research Center, Shiraz University of Medical Sciences.
CONFLICT OF INTEREST
All authors declare that they have no conflict of interest.
EHICAL APPROVAL
This project has been approved by Research Ethics Committee of Shiraz University of Medical Sciences. (Approval ID: IR.SUMS.REC.1400.646).
CONSENT
Written informed consent was obtained from the patients to publish this report in accordance with the journal's patient consent policy. One of our patients is 12 years old in which case, written consent was obtained from her parents.
Open Research
DATA AVAILABILITY STATEMENT
All essential data is included in the manuscript.




