Complete laryngotracheal separation after a clothesline-type injury: A case report
Abstract
This case report presents management of a complete laryngotracheal separation after a ‘clothesline’ type injury. Laryngeal trauma to some extent was suspected but the diagnosis was confirmed after massive subcutaneous emphysema occurred after seemingly successful intubation. The airway was secured with a tracheostomy and secondary laryngotracheal anastomosis was done.
1 INTRODUCTION
Severe laryngeal injury is rare – it accounts <1% of all trauma cases and is usually associated with high-velocity traumas.1-3, 5 Depending on the severity, laryngeal injuries are classified by the Schaefer Classification System.1, 3 Complete laryngotracheal separation (CLS) – group 5 injury – is a critical laryngeal injury and, if undiagnosed, might rapidly lead to airway loss and death. Its prevalence remains unknown because over 75% of patients with non-penetrating neck injuries die at the site of the scene or are dead upon arrival.2, 3 For those who reach the hospital alive, first the symptoms might not correlate with the severity, which can lead to a delayed diagnosis and a bad outcome.1, 2, 4
2 CASE PRESENTATION
A 27-year-old motorcyclist sustained a “clothesline” type injury to his neck by driving into an extended wire. The patient was transported to the nearest peripheral emergency department.
On arrival, the patient was alert and communicated with hand signs. He complained of aphonia, shortness of breath, and neck pain. Neck abrasion and ecchymosis were seen, and he was in a leaning forward position with inspiratory stridor, with oxygen saturation level of 93% at rest with supplemental oxygen. A chest radiograph showed pneumothorax on the right, so a chest tube was placed. His condition deteriorated and emergent intubation was attempted and even though complicated, seemed to be successful. As the patient was stable, he underwent a neck-and-chest computed tomography (CT) scan. However, soon after intubation, oxygen saturation started dropping and stayed around 70%, and he developed massive subcutaneous emphysema extending to his abdomen.
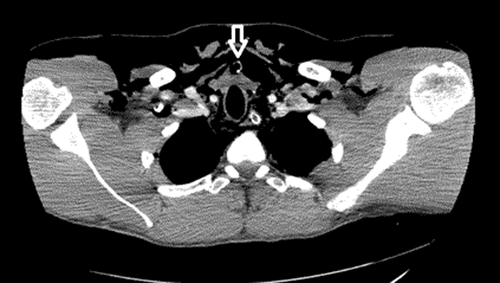
The CT scan showed the following: massive subcutaneous emphysema, bilateral pneumothoraces, pneumopericardium, and pneumomediastinum. Below the subglottis, the endotracheal tube had passed into the soft tissues, thus creating a false passage (Figure 1).
Another chest tube was placed. It was then decided that the patient was too unstable for transportation. A team of surgeons was brought from the nearest university hospital, and the patient was taken to the operating room for an urgent tracheostomy.
After the airway was secured, the patient was transported to the university hospital’s intensive care unit. The postoperative course was uneventful, and the patient was transferred to the ENT ward the next day. Flexible endoscopy, done for the first time, showed both vocal cords fixed in paramedian position, laryngeal edema.
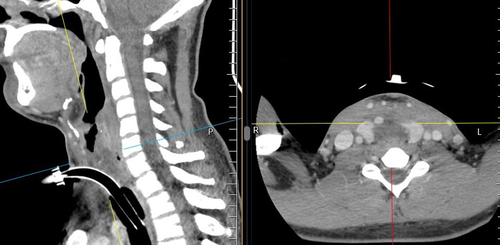
The second CT scan showed the following: subcutaneous emphysema and subsided pneumothoraces, no sign of pneumopericardium, a comminuted fracture of the anterior part of the cricoid cartilage, first and second tracheal rings deformed and pushed posteriorly without a lumen (Figure 2).
Two weeks after the trauma, tracheal resection and anastomosis were performed. Intraoperative findings noted total stenosis above the tracheostomy site (Figure 3). The anterior part of the cricoid was in fragments, the posterior part – intact, but fully separated from the remaining trachea, first and second rings pushed behind the cricoid. The stenotic segment and anterior part of the cricoid cartilage were resected. The thyroid cartilage and the remaining posterior part of the cricoid were reapproximated with the trachea. Recurrent laryngeal nerves were not visualized. A tracheostomy tube was placed below the anastomosis. After resecting the stenosis, the patient could speak with a hoarse voice when plunging the tracheostomy tube. The postoperative period was uneventful, and after 8 days, the patient was discharged.

On follow-up 2 weeks after the discharge, the patient had no complaints. Endoscopy through the stoma showed a nicely healing anastomosis with no relevant stenosis (Figure 4).

On follow-up after 4 months, the patient had no complaints except hoarseness. He had no problems breathing with a plunged tracheostomy tube. Decannulation was performed following flexible endoscopy, which showed fixed vocal cords, the space between them about 4 mm. The option of posterior cordectomy or laterofixation was discussed, but the patient refused further surgical procedures, because he was satisfied with his breathing and did not want to further reduce the quality of his voice.
3 DISCUSSION
Laryngeal injury should be suspected in any case of blunt or penetrating trauma to the neck. Ecchymosis, loss of thyroid prominence, and tracheal or laryngeal deviation are the signs of laryngeal trauma, which can be variable. The presence of subcutaneous emphysema should be telltale sign that there is a disruption of the airway integrity.1-5
Not all of the patients suffered CLS from a high-velocity trauma. There were case reports of CLS after attempted suicides by hanging,3 stab wounds,5 or workplace injuries.1
Considering the most important task – securing the airway, most case reports agree intubation, especially unguided by fibrobronchoscopy, should be avoided as it may displace the airway and create a false passage.1, 3, 5 Cricothyroidotomy in CLS serves little purpose, moreover, it can complete a partial laryngotracheal separation, and was attempted in only one case report.2 If possible, Schaefer recommended tracheostomy as a first-choice intervention.1, 5
After securing the airway, the patient should be inspected for other injuries. Interestingly, none of the patients in the reviewed case reports had skull base or intracranial injuries.1-5 Associated injuries were bilateral pneumothoraces,2, 4 pneumopericardium,2 common carotid dissection,4 and esophageal injuries.5 Our patient had bilateral pneumothoraces, which were treated with chest drains, and pneumopericardium, which subsided without intervention.
In this case report, secondary anastomosis was performed. Since only case reports regarding CLS are available, there is little research into whether primary or secondary anastomosis is more beneficial in long term. Most case reports opted for primary anastomosis, however, all had problems with granuloma formation and site stenosis.1, 3-5
Unsurprisingly, after laryngotracheal fractures, most patients suffer from vocal fold paralysis.1, 3, 5 In our case, the patient had bilateral paralysis. Interestingly, even though the vocal folds remained in an adducted position, over the months the space between them widened, which resulted in the removal of his tracheostomy tube.
4 CONCLUSION
Laryngeal injury should be suspected in any case of blunt neck trauma. At first, the symptoms might not correlate with the severity of the injury. The airway should be assessed firstly. In case of CLS, endotracheal intubation should be avoided. After securing the airway, the patient should be inspected for associated injuries.
AUTHOR CONTRIBUTIONS
Gintare Ciburaite composed the manuscript and made and gathered figures. Marius Kaseta, primary surgeon, revised the manuscript.
ACKNOWLEDGMENT
None.
CONFLICT OF INTEREST
The authors have no conflict of interest to disclose.
ETHICAL APPROVAL
Regional bioethics committee approval was obtained for this case report.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report and the accompanying images.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.




