Delayed COVID-19-induced cytokine storm after root canal therapy with favorable response to plasmapheresis, tocilizumab, and methylprednisolone pulses therapy: A case report
Abstract
COVID-19 showed different characteristics, and many cases showed clinical manifestations that could not be attributed to other conditions. We present a 22-year-old woman who had an uneventful recovery from COVID-19, and after that, she developed a cytokine storm and a worsening clinical condition 2 days after dental root canal therapy.
1 INTRODUCTION
The novel coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), emerged in Wuhan, Hubei province, China, in December 2019, and was declared a pandemic by the World Health Organization in March 2020.1, 2
COVID-19 causes a broad range of clinical features, from asymptomatic infection to symptoms including fever, fatigue, cough, myalgia, headache, nausea, and diarrhea, to severe forms of disease such as septic shock and acute respiratory distress syndrome (ARDS).3, 4 ARDS-induced respiratory failure is one of the significant reasons for death in COVID-19, with an incidence of 67% among patients with severe illness.5 ARDS is associated with an imbalance of the inflammatory response known as cytokine storm (CS).6, 7
CS is a life-threatening hyper-inflammatory condition that is characterized by excessive levels of circulating inflammatory cytokines containing tumor necrosis factor-a (TNF-a), interleukin-6 (IL-6), and interleukin-10 (IL-10).6, 8-10 CS may lead to organ injury (e.g., acute cardiac injury (22%), kidney injury (8%), arrhythmias (44%)), and even death.4, 11, 12
Due to the critical course of patients with CS, effective therapeutic approaches for COVID-19-induced CS are urgently needed. Different approaches such as cytokine-targeted therapies and extracorporeal cytokine removal therapies have been considered potential strategies for managing CS.13-15 However, their efficacy and safety still need validation in further clinical investigations.
The present report describes a 22-year-old female with delayed COVID-19 cytokine storm after root canal therapy who experienced a dramatic clinical improvement after combined use of plasmapheresis, tocilizumab, and methylprednisolone pulses.
2 CASE PRESENTATION
A 22-year-old woman was hospitalized in the emergency department of Shahid Sadoughi Hospital, Yazd, Iran, suffering from COVID-19 symptoms progressively worsening over the past 7 days.
She was positive for SARS-CoV-2 on the reverse transcription-polymerase chain reaction (RT-PCR) test 26 days before admission. After receiving the COVID-19 therapeutic regimen, she got better, but 2 days after root canal therapy owing to irreversible pulpitis, her COVID-19 manifestations recurred. She had no history of other underlying diseases.
On admission, her RT-PCR test was positive for SARS-CoV-2. On examination, she had a fever of 38.3°C, blood pressure of 122/82 mmHg, and pulse of 85 beats per minute. She was in mild respiratory distress with a respiratory rate of 19 breaths per minute, and oxygen saturation was 92% on room air.
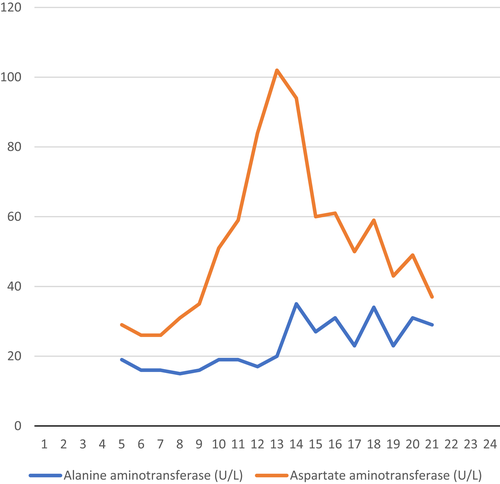
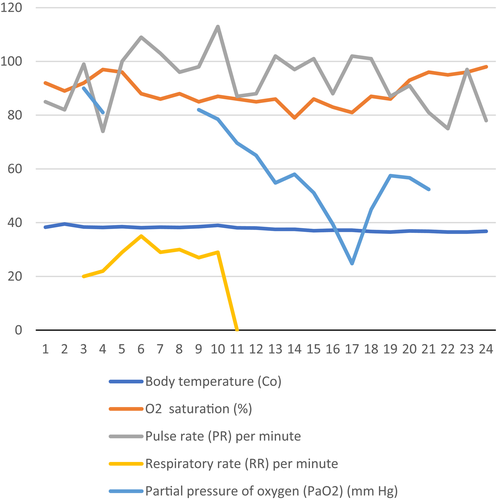
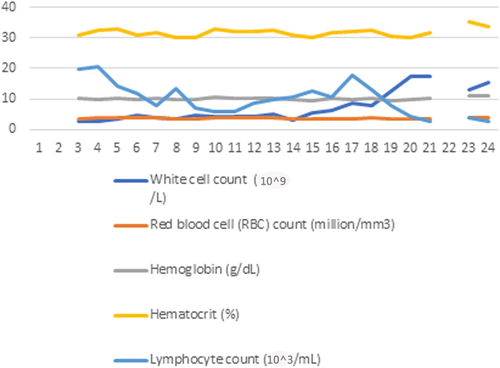
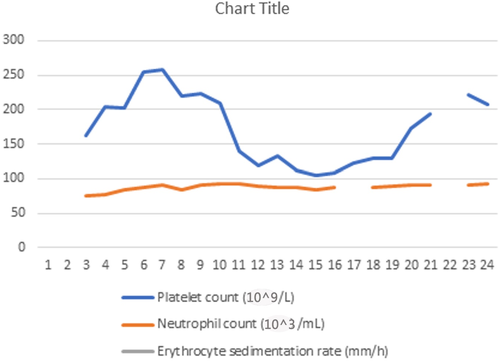
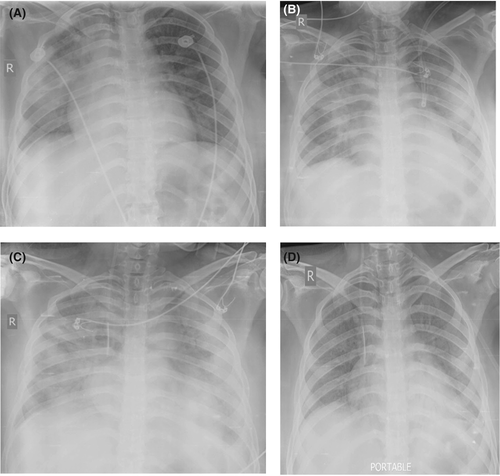
C-reactive protein (CRP) was 67.3 mg/L, and erythrocyte sedimentation rate (ESR) was 94 mm/h. Information about clinical and paraclinical data is shown in Figures 1-4. Chest radiograph showed peripheral and lower opacities in the right lung, Figure 5 (A). A chest computed tomography (CT) scan on admission (Figure 6) showed alveolar opacities and dense consolidations with air bronchogram affecting the right upper and middle lobes, central alveolar opacities in the left upper lobe, and mild bilateral pleural effusion.

Given that these findings suggest the superimposed bacterial pneumonia process, she started empirical broad-spectrum antimicrobial therapy. Complementary microbiological screenings were done on the fourth day of admission, and all results were negative. The course of the disease is shown in Table 1.
| Day | Clinical course | Laboratory test | Treatments | Other considerations |
|---|---|---|---|---|
| Aug 25, 2021 |
Fever Dry cough Headache Myalgia |
RT-PCR SARS-CoV-2 positive |
9-day course conservative treatment then 5-day course remdesivir 200 mg intravenously (on the first day) then 100 mg intravenously daily (for up to 4 additional days) + dexamethasone (6 mg intravenously once daily) |
|
| Sept 8 | Symptoms remission | |||
| Sept 11 |
No COVID-19 manifestations Tooth decay and toothache due to irreversible pulpitis |
Root canal therapy (left mandibular first molar tooth) | ||
| Sept 13 |
Fever Dyspnea Hemoptysis |
symptoms worsened over the following days | ||
|
1st day of admission (Sept 20, 2021) |
Persistent fever (38.3°C) Chills Sweating Dyspnea Hemoptysis Shortness of breath Productive cough Mild respiratory distress |
RT-PCR SARS-CoV-2 positive |
Empiric broad-spectrum antimicrobial therapy started with linezolid (0.6 g, bid, iv) plus meropenem (1 g, tds, iv) for 7 days | |
| 4th day of admission |
Fever Oxygen requirement |
Microbiological tests including blood and sputum culture, pan fungal PCR assay, Coombs test, Wright's serum agglutination, 2-mercaptoethanol (2-ME), quantitative PCR for P. jirovecii, fourth-generation human immunodeficiency virus (HIV) enzyme-linked immunosorbent assay, and PCR testing for M. tuberculosis, influenza virus, polyomavirus, BK virus, Pneumocystis jirovecii, Nocardia, and C. difficile bacteria | non-rebreathing mask (oxygen flow of 10 L/minute) |
Admitted to ICU No endobronchial lesions observed in bronchoscopy |
| 7th day of admission | No clinical improvement | Autoimmune and serological tests reported normal |
Three-day consecutive course of IVIG therapy (500 mg/kg/day) |
|
| 9th day of admission |
Fever (38.5 °C) She rapidly progressed to acute hypoxemic respiratory failure |
Cytokine storm diagnosis was made | ||
| 10th day of admission |
RT-PCR SARS-CoV-2 positive |
Tocilizumab (0.4 g, qd, iv) + Double filtration plasmapheresis |
Previous therapy was not efficient | |
| 11th day of admission |
The increased need for oxygen Respiratory distress Tachypnea |
Corticosteroid pulse + Non-invasive ventilation in protective-ventilation strategy (FIO2 100%, PEEP 8 mmHg, and pressure support 18 mmHg) |
Normal echocardiography | |
| 12th day of admission |
Tocilizumab (0.4 g, qd, iv) + Double filtration plasmapheresis |
|||
| 13th day of admission | Corticosteroid pulse | |||
| 14th day of admission |
Tocilizumab (0.4 g, qd, iv) + Double filtration plasmapheresis |
|||
| 15th day of admission | Corticosteroid pulse | |||
| 16th day of admission | No fever |
Tocilizumab (0.4 g, qd, iv) + Double filtration plasmapheresis |
favorable clinical response to treatment combined inflammatory cytokine depletion therapy was successful |
|
| 17th day of admission | Corticosteroid pulse | |||
| 18th day of admission |
Tocilizumab (0.4 g, qd, iv) + Double filtration plasmapheresis |
|||
| 19th day of admission | Corticosteroid pulse | |||
| 22nd day of admission |
Weaned off from non-invasive ventilation and transitioned to supplemental oxygen (after oxygen saturation level raised 96%) |
There was no clinical improvement by the seventh day of admission when the chest X-ray, Figure 5B, showed progression of lung involvement with bilateral peripheral alveolar opacities. She was evaluated for autoimmune diseases, and antinuclear antibody tests were sent. At the serologic examination, serum levels of antinuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA), anti-Ro, anti-La, and anti-double-stranded DNA (dsDNA) were all negative, and in the normal ranges.
Intravenous immunoglobulin (IVIG) therapy (500 mg/kg/day) was started, but she remained febrile despite the 3 dayS course of IVIG therapy. On the ninth day of admission, her chest X-ray, Figure 5C, showed a noticeable progression of diffuse alveolar opacities with lower and peripheral predominance.
A diagnostic pleural tap was conducted. The pleural fluid analysis was consistent with an exudative effusion with the protein 1.5 (mg/dL), an LDH of 1432 (U/L), and glucose of 143 (mg/dL). The pleural fluid differential white cell count revealed 80% lymphocytes and 20% neutrophils, incompatible with the bacterial infection process. No microorganism was found in the pleural fluid on culture and PCR. The cytologic analysis of pleural fluid was negative for malignant cells.
On the same day, her laboratory results indicated deteriorating inflammatory markers (IL6 39.1 pg/mL, CRP 90 mg/L.1, LDH 1115 IU, ferritin 459.6 μg/L, and ESR 77 mm/h). RT-PCR test was positive for SARS-CoV-2 for the second time. Her clinical picture indicated the possibility of cytokine storm syndrome, not responding to her recent treatment.
On Day 10 of admission, due to her critical condition and poor response to the previous treatments, administration of five sessions of combined inflammatory depletion therapy, including tocilizumab (0.4 g, qd, iv) and double filtration plasmapheresis (plasma volume was set as 2 L, the substitution fluid was albumin solution, blood flow rate 80–120 ml/min, plasma flow rate on separator 30 ml/min, and waste flow rate 3.0 ml/min) and corticosteroid pulses (250 mg of methylprednisolone for 5 days) were started for the patient. Six days later, after receiving the fourth course of plasmapheresis, favorable improvements in both laboratory and CXR findings were seen in Figure 5 (D).
She remained on non-invasive ventilation until Day 21 of admission, after which her oxygen saturation level rose to 96% on a non-rebreathing mask (oxygen flow of 10 L/minute). Her CXR showed resolution of pulmonary opacities, so she transitioned to supplemental oxygen. She was discharged after 24 days of hospitalization with a recovered clinical condition on supplemental oxygen. At 4 weekS follow-up, she was symptom-free, hemodynamically stable, with oxygen saturation of 96% at rest in room air.
3 DISCUSSION
As far as we know, we reported the first case of COVID-19 with delayed presentation of CS after performing root canal therapy. As noted, this is a rare case because of the prolonged time between the beginning of COVID-19 symptoms and the occurrence of cytokine storm and additionally relapsing the COVID-19-related symptoms after performing root canal therapy. Our patient responded dramatically to plasmapheresis, tocilizumab, and corticosteroid therapy.
CS is one of the leading causes of ARDS, leading to higher mortality in severe types of COVID-19.16 The pathogenesis of CS is still completely unclear. However, some studies explained that Interleukin-6 (IL-6) plays an essential role in the induction of CS by activating the Janus Kinase and Signal Transducer and Activator of Transcription (JAK/STAT) pathway, which causes the production of acute-phase proteins as an essential factor of inflammation.17, 18 CS usually happens 8–10 days after the start of COVID-19 symptoms.19 In our patient, the cytokine storm occurred after the 25th day of the onset of the COVID-19 symptoms. This could be because of the root canal therapy performed 9 days before hospitalization.
Root canal therapy reduces the inflammation due to the necrosis of dental pulp or irreversible pulpitis.20, 21 Some studies recommend mixed irrigation methods, and finding a proper non-mix method (material, instrument,) should be observed to remove pathogens properly. Root canal pathogens cause an increase in the TNF-α level, an inflammatory cytokine. This could affect the apical papilla stem cells to secrete pro-inflammatory cytokines and matrix metalloproteinase to increase regeneration.22 Bacterial endodontic contents from primarily infected root canals exhibited potent antigenic activity against macrophage cells, leading to cytokine production determined by the secretion of IL-1β, TNF-α, IL-6, and IL-10, with most of them interplaying a network role in the inflammatory process,23 So the importance of dressing between appointments is highlighted in these cases.24 IL8, IL6, MMP9, and chemokines were also introduced as pulpitis biomarkers.25 In cases of endodontic failure, persisting microorganisms in the root canal, IL-17A, IL-1β, TNF-α, and IFN-γ could be increased.26 Not performing proper endodontics protocol in filing and flaring, irrigation and obscuration is a source of inflammation production.27 Some of these inflammatory secretions are similar to ones in cytokine storms. Hence, in the COVID-19 era, this inflammation might be dangerous in the course of the COVID-19 inflammation in the body. In endodontics, calcium hydroxide-based, zinc oxide eugenol-based, and mineral trioxide aggregate-based (MTA) filling materials increased some interleukins in osteosarcoma cell lines,28 So even after successful endodontic treatment, probable inflammation due to dental material might be happening.
Moreover, different bacteria in the root canal could change the inflammatory secreted cytokines in addition to clinical manifestations.29 As it was indicated that the oral cavity's microbiomes might be changed due to COVID-19, it should also be considered that proper irrigation methods that could affect different root canal pathogens are necessary.30 Tocilizumab is an IL-6 receptor blocker that plays a vital role by binding to the membrane and soluble-bound IL-6 (mIL-6R and sIL-6R) receptors and reduces the inflammatory response induced by IL-6.31 Sahni & Gupta hypothesized that elevated levels of cytokines in locally inflamed gingival tissue are associated with elevated cytokine levels in the systemic circulation. The common inflammatory response pathway is possibly associated between periodontitis and COVID-19-related adverse outcomes.32
The systemic inflammation in patients with COVID-19 and the aspiration of periodontopathogens during the root canal therapy could synergize with the coronavirus or modulate the immune response to COVID-19. Periodontal pockets can serve as potential viral reservoirs, and periodontitis or endodontic procedures could increase the viral load.31
Potential strategies such as tocilizumab, corticosteroid, and IVIG therapy are considered to manage CS. Tocilizumab reduces the IL-6 and CRP levels and improves patients' respiratory parameters and clinical conditions. The effectiveness of IVIG therapy for severe forms of COVID-19 is not completely clear.33 Our case experienced no significant improvement after IVIG therapy, and she remained febrile, but the use of tocilizumab and corticosteroid therapy favorably influenced her clinical course.
Plasmapheresis is also an effective potential therapeutic approach for CS in COVID-19 patients. Hashemian et al. expressed the effect of plasmapheresis in the reduction of IL-6 in COVID-19 patients from 8.3 ± 1.8 to 5.7 ± 1.3.34
Our patient responded favorably to the treatment of plasmapheresis and tocilizumab. Decreased levels of IL-6 from 39.1 to 1.36, reduced CRP levels, elevated oxygen saturation, and normal body temperature were observed after treatment.
4 CONCLUSION
This article reported a delayed COVID-19-induced cytokine storm after root canal therapy with a favorable response to plasmapheresis, tocilizumab, and methylprednisolone pulses therapy. The possible effect of dental procedures on people with COVID-19 infection is still unclear, and further investigations are needed. It would be recommended for all medical doctors and dentists to report COVID-19 cases after dental procedures.
AUTHOR CONTRIBUTIONS
MMDB, MM, and HG were responsible for data collection. MMDB, MM, and HG wrote the initial draft and FAM. SM revised the draft. All authors contributed to the draft and approved the final version of the manuscript.
ACKNOWLEDGMENT
The authors are incredibly thankful for all the support from Shahid Sadoughi hospital, its personnel, and the patient and her parents for their consent.
CONFLICT OF INTEREST
There is no conflict of interest to be declared.
ETHICAL APPROVAL
Informed consent was obtained from the patient, and Helsinki 1964 Declaration and its later amendments were observed.
CONSENT
Prior to submission, written informed consent was obtained to publish the case.
Open Research
DATA AVAILABILITY STATEMENT
All the patient data could be accessed upon reasonable request from the corresponding author and the agreement of all research team members.




