Promising effects of corticosteroid treatment in combination with antifungal agents in a patient with Aspergillus meningitis
Funding information
None
Abstract
Although Aspergillus meningitis is poorly responsive to current guidelines for treatment, we describe a dramatic response of Aspergillus meningitis in a patient to treatment using a combination of corticosteroids with guideline’s suggested antifungal agents. Administration of corticosteroids in patients with Aspergillus meningitis is rarely reported in previous studies.
1 INTRODUCTION
About 10%–15% of cases of Invasive Aspergillosis (IA) affect the central nervous system (CNS) as neuroaspergillosis.1 Being immunocompromised is the major risk factor for IA of the CNS with reported mortality rate of approximately 90% (compared with 10%–20% in immunocompetent individuals); and developing a proper medical approach for the treatment of neuroaspergillosis is very challenging because of its poor response to treatment.2 This could be due to intrinsic or acquired antifungal resistance, which is an emerging problem in current era, and even with current guideline of using new antifungal agents, outcomes of patients with this condition are not promising.3 Patients with neuroaspergillosis present with a variety of signs and symptoms such as fever, headache, dizziness, seizure, lethargy, altered mental status, gait disorders, visual impairment, and diplopia.4 One of the main manifestations of previously reported cases of IA involving the CNS is mass lesions seen in infectious meningitis.5
Herein, our case report describes a rare case of neuroaspergillosis in Iran, in which a dural aspergillus abscess is identified in cerebral aqueduct, and corticosteroid therapy is added to guideline's suggested antifungal agents.
2 CASE REPORT
A 41-year-old female patient was admitted to the emergency department of hospital with chief complaint of frontal headache. Initially her headache had an on/off pattern that started 10 days earlier and progressed over time. She reports having fever and chills before onset of the headache and around 2 days prior to referring to our hospital. She developed delusion at the time. Her headache did not follow any specific patterns.
In her past medical history, she mentions being hospitalized due to a severe burn involving 35% of total body surface area around 5 months ago. Two months later, deep vein thrombosis developed in her right leg and rivaroxaban was prescribed as the treatment. She did not report any notable habitual and familial history as a predisposing factor for a specific headache pattern.
No signs of loss of consciousness and seizures were present. In neurological examination, only papilledema was observed. There was no sign of neurologic deficit.
A head computed tomography (CT) scan was taken, which showed mild triventricular hydrocephalus. The results of hematologic and cerebrospinal fluid tests are described in Table 1.
| Test | Result | Unit |
|---|---|---|
| Basic hematology tests | ||
| Quantitative CRP | 42 | mg/dl |
| CBC | ||
| Hemoglobin | 10.4 | gr/dl |
| MCH | 28.49 | pg |
| MCHC | 31.52 | % |
| MCV | 90.41 | FL |
| Red blood cells | 3.65 | 106 cells/L |
| White blood cells | 5.7 | 103 cells/L |
| Platelet | 246 | 103 cells/L |
| Hematocrit | 33 | % |
| Biochemistry tests | ||
| Blood sugar | 112 | mg/dl |
| BUN | 10 | mg/dl |
| Creatinine | 0.71 | mg/dl |
| K | 3.7 | meq/L |
| Na | 142 | meq/L |
| LDH | 44 | U/L |
| Alkaline phosphatase | 148 | U/L |
| Alanine transaminase | 7.6 | U/L |
| Aspartate transaminase | 8.1 | U/L |
| Ca | 8.85 | mg/dl |
| Phosphorus | 5.8 | mg/dl |
| Coagulation assay and PT | ||
| PTT | 35 | Seconds |
| INR | 1 | |
| PT | 13 | Seconds |
| CSF analysis | ||
| Anaerobic culture | No bacterial growth | - |
| Appearance | Clear | - |
| Aerobic culture | No bacterial growth | - |
| Color | Color-less | - |
| Direct smear | PMN = 0 | - |
| Glucose | 19 | mg/dl |
| Gram stain | No bacteria were seen | - |
| Protein | 87 | mg/dl |
| RBC | 0 | - |
| WBC | 0 | - |
| Other tests | ||
| RT PCR for SARS-CoV-2 | Negative | - |
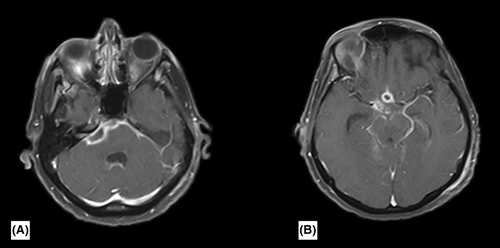
Based on the clinical and para-clinical suspicion of inflammatory or infectious meningitis, additional tests were performed for the patient and following results were obtained: PCR for Cryptococcus neoformans was negative, CSF and serum angiotensin converting enzyme (ACE) were normal, chest CT-scan showed no abnormality, tuberculosis (TB) PCR, CSF molecular-based (MTB) PCR, and PPD tests were negative. Malignancy work-up showed no abnormal results. Nested PCR6 of the CSF was positive for Aspergillus flavus. Therefore, a non-contrast magnetic resonance imaging (MRI) of the brain was taken, in which a basal leptomeningeal enhancement in the area of pons and medulla, and a rim-enhancing lesion in the right cerebellopontine angle (CPA) was observed (Figure 1). Thus, a high degree of certainty for diagnosis of CNS aspergillosis was achieved. The antifungal susceptibility test was performed by the broth microdilution method using four antifungal agents, including voriconazole (VCZ; Merck, Germany), itraconazole (ICZ; Merck, Germany), fluconazole (FCZ; Merck, Germany), and amphotericin B (AMB; Merck, Germany). Based on the Clinical and Laboratory Standards Institute (CLSI) M38 3rd ed.,.7 Candida parapsilosis (ATCC 22019) was chosen as a quality control strain.
The A. flavus strain showed resistance to FCZ, ICZ, with minimum inhibitory concentration MIC>16 and MIC>1 μg/mL, respectively. Furthermore, susceptibility to voriconazole (MIC 0.313 μg/mL) and amphotericin B (MIC 0.313 μg/Ml) was noted in this study.
Based on the result of antifungal susceptibility tests and, intravenous (IV) VCZ, intrathecal, and IV AMB were prescribed for the patient, and IV dexamethasone was added to her antifungal treatment.
Brain CT-scans taken on consecutive days showed a progressive triventricular hydrocephalus, and brain non-contrast MRI showed progression of the leptomeningeal enhancement to basal and suprasellar cisterns (with pressure effect on the optic chiasm). In addition to the CPA, rim enhancement progressed to the right internal auditory canal (IAC) and enhancement of the basilar and circle of Willis vessels were also observed. Because of the patient's hydrocephalus and rise of ICP neurosurgery consult was obtained following which an external ventricular drainage (EVD) was placed in patient's left lateral ventricle to drain excessive CSF.
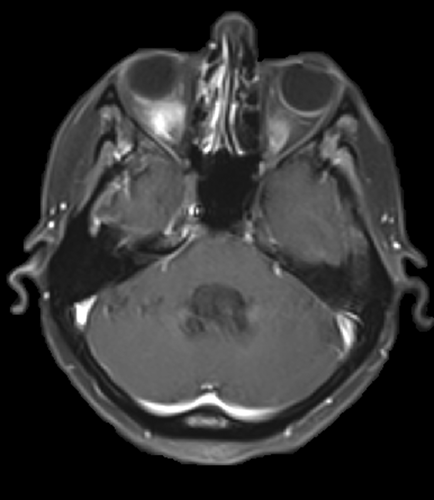
After 5 weeks on the mentioned combination therapy, resolution of lesions was observed on imaging (Figure 2), and a few days later, the patient's hydrocephalus reduced, so her condition improved dramatically.
3 DISCUSSION
Among all the reported sites of IA, CNS is considered to be the most devastating, which accounts for 10%–15% of cases of aspergillosis1; and using corticosteroids to manage a fungal infection-mediated hydrocephalus is a controversial.8 Previously, the initial treatment of choice for IA affecting the CNS was systemic antifungal treatment with AMB, but now guidelines have switched to VCZ as the initial treatment, given that VCZ is more capable of reaching the proper concentration required for antifungal activity in the CSF. It also has lower toxicity potential compared with AMB.1, 9 Also, ICZ and isavuconazole (ISZ) were used in some previous cases; Tattevin et al. reported 3 patients with neuroaspergillosis and underlying diseases, receiving ICZ in combination with other agents. One of the patients (a known case of wegener granulomatosis) was cured with AMB (29 days) + ICZ (410 days), another individual (suffering from laryngeal cancer) receiving AMB (25 days) + ICZ (13 days) died, and the last one (a case of systemic lupus erythematosus and end-stage renal disease) was cured by receiving liposomal AMB (44 days) + VCZ and ITZ (380 days).10 Taking into consideration that outcomes of monotherapy vs. combination therapy could be an important point of comparison in previous reports of neuroaspergillosis, Karthic et al. reported an expired case that was treated with VCZ,11 Haroon and colleagues mentioned another expired case who received AMB,12 but the overall results of combination therapy were more promising; Gruter et al. reported a neuroaspergillosis patient (who also had thyroid cancer) receiving VCZ+ AMB+ ISZ who was cured.5 Leroy et al. 13 and Turki et al.14 both reported cured cases of neuroaspergillosis treated with VCZ + liposomal AMB, and of 5 cases described in Tattevin and colleagues' study, 3 were cured by combination therapy.10
In addition to the above-mentioned antifungal agents, using corticosteroids draws attention which is rarely reported previous cases. Although not recommended in current guidelines, corticosteroids may improve outcomes in Aspergillus-related meningitis presenting with hydrocephalus; even with consideration of the fact that corticosteroids have an anti-inflammatory nature and may apply a minimizing effect on immune cells. Hiraga et al. reported a case of meningitis caused by Aspergillus infection in an immunocompetent woman that was complicated by respiratory failure, which was dramatically cured by VCZ and corticosteroids and no relapse was observed.15 The mentioned study and our experience of positive outcomes with combination therapy using corticosteroids and antifungal agents may provide an evidence for potentialities of this combination therapy to treat fungal meningitis. Surgical debridement is considered to reduce mass effect caused by abscess, and EVD may be placed to treat hydrocephalus.10
AUTHOR CONTRIBUTION
PA has made substantial contributions to conception and design, revised, and gave final approval of the version to be published. EL has made substantial contributions to conception and design and participated in drafting the manuscript. KR Involved in collaboration between hospital and laboratory and participated in drafting the manuscript. AF involved in conception and revise of the manuscript. FA agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SO involved in conception and revise of the manuscript. AM involved in drafting the manuscript.
ACKNOWLEDGEMENTS
Published with written consent obtained from the patient.
CONFLICTS OF INTERESTS
There are no conflicts of interest related to this case report.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images and videos. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Research
DATA AVAILABILITY STATEMENT
Data are available on request.




