Long-segment restrictive tear of radial artery under ultrasound guide for arteriovenous fistula by PTA: A case report
Funding information
This work was supported by the National Natural Science Foundation of China (Grant No. 81803967)
Abstract
Considerable calcification and stenosis frequently occur in the radial artery (RA) in diabetic nephropathy. PTA was performed successfully using a balloon to expand and restrictively tear the longitudinal axis of the RA. This approach seems to be a useful measure of promoting the maturation of AVF in diabetic nephropathy.
1 INTRODUCTION
The prevalence of uremia due to diabetic nephropathy (DN) has recently increased and evolved as the primary cause of uremia worldwide.1 Vascular sclerosis, a diabetic complication, involves extensive calcification of arteries triggered by uremia in DN.2 Therefore, the immaturation of AVF in these patients leads to failure, and insufficient lumen causes deficient blood flow; thus, it is not used in treating dialysis. It is challenging to create vascular access in a good vein in DN.3
The traditional percutaneous transluminal angioplasty (PTA) method of AVF is the expansion of the RA using an aortic balloon under ultrasound guidance or digital subtraction angiography. However, the high risk of tearing the RA by PTA in the clinical setting limits the possibility of achieving a satisfactory lumen of the RA. This study shows how to address these challenges using a novel PTA method.
2 CASE REPORT
A 55-year-old female patient was admitted to the hospital with the complaint of uremia due to DN. She was diagnosed with type 2 diabetes 20 years back, and hemodialysis was initiated using the long-term catheter in May 2018 owing to uremia. The patient had developed for 5 days due to a catheter infection. Inflammatory biomarkers c-reactive protein (CRP) increased to 86.1 mg/L, and procalcitonin (PCT) was 1.3 ng/ml. The blood culture revealed the presence of human Staphylococcus. Cefazolin sodium was used for injecting and sealing a long-term catheter. Long-segment stenosis of the RA and palpation appeared similar to firm bands without pulsation. Artificial blood vessel replacement is an optimal choice; however, it could economically be unaffordable to many patients. The patient provided written informed consent for her case report and related imaging studies.
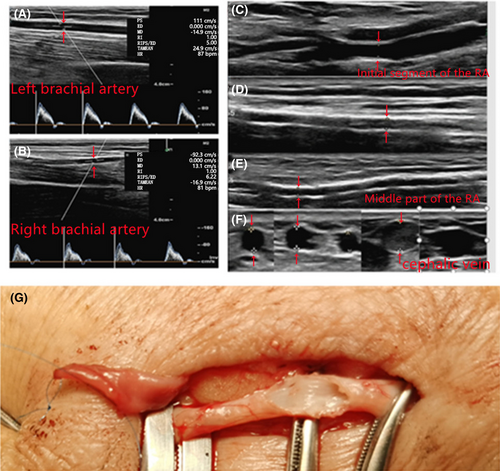
The color Doppler ultrasound of the right upper forearm demonstrated that the inner diameter of the right RA and vena capitis was 1.6–2.44 mm and 3.3–3.4 mm (Figure 1A–F). The right forearm AVF was established 12 days later after controlling infection in December 2019. The RA wall appeared white with poor elasticity and hard texture, and the diameter was approximately 1.8 mm during operation (Figure 1G). The RA was dissected diagonally and elliptically, and the hemostatic clamp could not seal the flow. The port of the RA was anastomosed with the side of the cephalic vein. The postoperative thrill of AVF was anticipatedly weak. Finally, low molecular weight heparin was injected subcutaneously at 3000 IU and papaverine 30 mg for qd X 7 days, postoperatively, and a follow-up visit date was planned 2 months later.
The patient was readmitted to our hospital with repeated catheter infection in June 2020, 6 months later. The value of inflammatory biomarkers returned to high levels: B-type natriuretic peptide >30,000 ng/ml; CRP, 153.5 mg/L; and PCT, 10.5 ng/ml. The color ultrasound demonstrated the distal inner diameter of the cephalic vein of AVF as 1.5–3.1 mm (Figure 2A), which had been diagnosed as sclerosis and stenosis of the RA, and distal cephalic vein stenosis in the AVF segment. Further information indicated that the fistula vein was in good condition; however, sclerosis and stenosis were discovered in a long segment of the RA.

Hence, the first PTA was implemented after brachial plexus block anesthesia. The 6F sheath was implanted using the distal RA as an access point, and the venous fistula was expanded firstly. The AVF tremor was slightly increased after successful dilation. Then, the DR8044 balloon (diameter 4 mm, length 4 cm, pushrod 80 cm length) was transmitted into the proximal RA, where calcification and stenosis were severe, contributing to poor intracavitary imaging and hard advance push of balloon from far to near. When the distal stenosis of the RA was successfully dilated, the balloon appeared to be bursting and filling. After PTA, the blood flow of the brachial artery was increased from 326 cc/min to 872, that of the RA was augmented from 18 to 464 cc/min, and the flow of AVF in the right upper limb had increased dramatically. Meanwhile, the RA of the right forearm and the distal cephalic vein of the AVF segment were wider than before (Figure 2B).
Four months later, she was readmitted in October 2020, owing to severe chills and fever caused by repeated catheter infections. Tremors of palpation AVF were weak. Then, the catheter was extubated, and the AVF dialysis was executed, although with insufficient flow. The color ultrasound demonstrated that calcification and stenosis happened in the distal RA, stenosis occurred at the distal cephalic vein of the AVF segment in the right forearm, and blood flow of AVF was insufficient (Figure 3A).
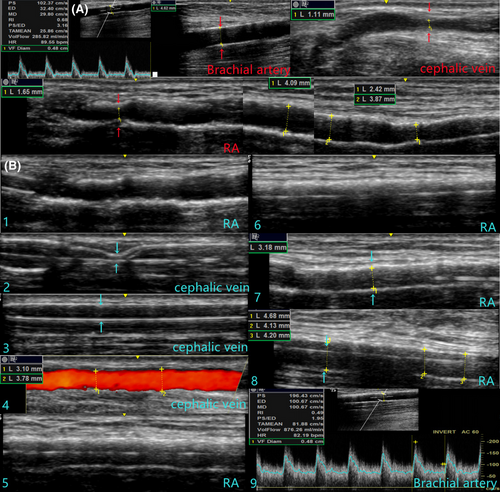
Then, the second PTA was performed. The distal RA was chosen as an access point to implant the 6F sheath, and subsequently, the venous fistula was expanded utilizing the CQ5054 aortic balloon (diameter 5 mm and length 4 cm). Afterward, the tremor of AVF was enhanced slightly. Then, we placed the CQ5054 into the proximal RA and inserted the DR4044 aortic balloon (diameter 4 mm and length 4 cm) to expand the proximal RA with filling balloon pressure up to 24 ATM. Nevertheless, the rebound was obvious after withdrawing the balloon, and no further improvement of the tremor was observed. Moreover, the blood flow was hardly ameliorated, and it was at 437 cc/min without significant increase compared with pre-operative values. Thus, the surgical approach and protocol were modified; we utilized the CQ5054 to tear the proximal RA with a pressure of 20 ATM and moderately dilated a segment with the length of 2 cm. Afterward, the tremor of AVF was enhanced significantly, which extensively reached to elbow, and the blood flow rate (BFR) was approximately 872 cc/min. Meanwhile, the BFR in the brachial artery was increased from 285.82 cc/min up to 876.26 cc/min (Figure 3B), BFR in the RA from 18 cc/min to 415.48 cc/min (Figure 3C).
3 DISCUSSION
The PTA functions primarily based on rupturing plaques, stretching vessel walls, and expanding lumens. PTA is beneficial as it is a minimally invasive procedure with minimal injury. The maximum protection can be achieved for the vascular resources of patients, which could be used for sclerosis and stenosis of artery or vein of AVF.4 Traditional arterial maturation is primarily used for segmental AVF artery lesions to obtain lumen by flattening plaques.5
This case reported a unique PTA alternative, which was operated with restrictive artery laceration in DN. The long section of the stenosis artery was torn longitudinally with a balloon of appropriate size (generally 4–5 mm in diameter). Novel vessels could be formed via partly deriving from the original vessel, which surrounded with deep fascia accompanied the vein, and partial thrombosis components. The balloon pasted can form a novel lumen to provide satisfactory blood flow for a long time. The structure is unstable at an early stage, whereas it would be more stable when the intima is reformed later. Thus, PTA is primarily used for long-segment stenosis in the RA of AVF. A small volume of blood leaks out to the surrounding space, owing to the abundance of fascial tissues around the RA. However, surgical accidents such as large hematoma and arterial dissection might occur if operated crustily.
We would like to make the following suggestions: (1) Noncompliance balloon with a diameter of 4–5 mm is important; (2) the distal access to the RA is convenient; and (3) treatment of lesions should be executed from downstream to upstream. First, the fistula vein lesions need to be treated, the dilated distal end of the RA should be treated subsequently, and proximal of the RA should be treated in last. (4) After the first tear, the blood flow should be opened by sticking a balloon for 30–60 s to allow it to enter the blood vessels and surrounding spaces. Then, the balloon is pressurized again, and the lasting time should be more than 5 min. (5) The brachial artery blood flow should be blocked before the distal RA pressurizing secondly.
4 CONCLUSION
The upper limb arterial lesions of patients undergoing hemodialysis should not be ignored. Restrictive tear of the RA could be used to promote the AVF maturation. We should innovate conventional principles and anticipate the best individualized therapeutic application of PTA alternatives.
AUTHOR CONTRIBUTIONS
JX, JZ, and JF conceptualized and designed the study, and together with SR, were involved in data acquisition and interpretation. XJ, JZ, NM, and SR were involved in the drafting of the article and JF revised it critically for important intellectual content. All authors were involved in the clinical management of the patient and approved the final version of the manuscript prior to submission. SR and JF agreed to be accountable for the article and to ensure that all questions regarding the accuracy or integrity were investigated and resolved. JX and JZ participated equally and should share “first authorship” of this paper.
ACKNOWLEDGMENTS
The authors would like to thank the director of the Department of Nephrology NO. 1, Affiliated Hospital of Chengdu University of Traditional Chinese Medicine, for his permission to publish the paper.
CONFLICT OF INTEREST
None declared.
ETHICAL APPROVAL
Our work has been conducted in accordance with the Declaration of Helsinki (1964). We have obtained written consent from the patient to publish her case and images. In line with our Institutional Ethics and Research Committee (IERC) guidelines, this case report was exempted from full IERC review.
CONSENT
Written informed consent for publication was obtained from the patient.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.