Isolated IgG4-related sclerosing cholangitis with normal serum IgG4 levels—A case report
Funding information
This work was supported by the National Natural Science Foundation of China (grant number 81500444).
Abstract
The isolated IgG4-SC that absent from AIP is quite rare and difficult to diagnose. We presented a case of isolated IgG4-SC with the normal serum IgG4 which was hard to differentiate with cholangiocarcinoma. Under such circumstances, liver pathology has a pivotal role in the diagnosis.
1 INTRODUCTION
Immunoglobulin G4-related sclerosing cholangitis (IgG4-SC) is a fibroinflammatory autoimmune disease which is frequently associated with autoimmune pancreatitis (AIP) and elevated serum IgG4 levels. This article presented a case of isolated IgG4-SC with normal serum IgG4 levels and no obvious pancreatic lesion which was difficult to achieve a preoperative diagnosis.
Immunoglobulin G4-related sclerosing cholangitis (IgG4-SC) is a distinct type of cholangitis frequently associated with autoimmune pancreatitis, which is currently recognized as a biliary manifestation of lgG4-related disease.1 It is characterized by the sclerosing and inflammatory of the affected organs which are infiltrated by massive IgG4-positive plasma cells2, 3 and the elevating of the serum IgG4 levels.2, 4 The diagnosis of IgG4-SC is difficult, especially for distinguishing from primary sclerosing cholangitis (PSC) and bile duct cancer.5-7 In this article, we presented a very rare case of IgG4-SC without the elevating of the serum IgG4 levels and other organs affected, who was misdiagnosed as cholangiocarcinoma. The final diagnosis was based on surgery and pathological examination. We provide a very atypical case that may be ignored by us and revealing the pivotal role of the pathology.
2 CASE REPORT
This case was approved by Ethics Committee of Tongji Medical College, HUST. And the informed consent was obtained.
A 58-year-old woman was hospitalized with dark-colored urine, yellow color of skin, and sclera for 1 day. Other symptoms and the history of upper abdominal pain, excessive drinking, and autoimmune disease were denied by this patient. On admission, the laboratory examination revealed that her total bilirubin, aspartate aminotransferase, alanine aminotransferase, and globulin level were normal, whereas the direct bilirubin, alkaline phosphatase, and γ-glutamyl transferase were elevated to 11.3 mmol/L, 160 and 216 U/L, respectively. The total protein and albumin decreased. The serum level of IgG4 was within normal range (1.51 g/L). Blood routine test, kidney function, serum amylase, and lipase were all normal.
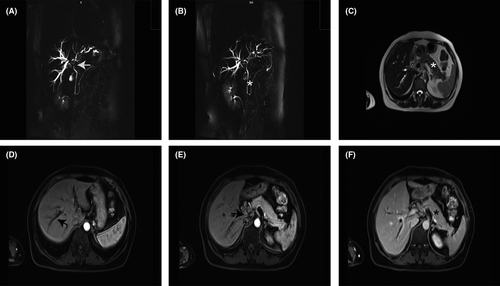
The contrast‑enhanced computed tomography (CT) presented the liver's Glisson sheath widening and stiff with the dilated intrahepatic bile duct, while the gallbladder, pancreas, spleen, and kidney were normal in both morphology and CT attenuation value. Enhanced magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) (Figure 1) indicated that strictures of the bile duct in the hilar hepatic lesions including the left, right, and main hepatic bile ducts were significantly thickened with the catheter slightly narrowing. The DWI diffusion of the hepatic bile ducts was restricted and continuous reinforcement on the enhancement scanning continued to strengthen, while the main pancreatic duct and the main bile ducts were normal without enlargement or abnormal enhancement in the area of the pancreas. In addition, there were plenty of lymph nodes in the hilar hepatic area. Based on the presentation above, cholangiocarcinoma was clinically suspected.
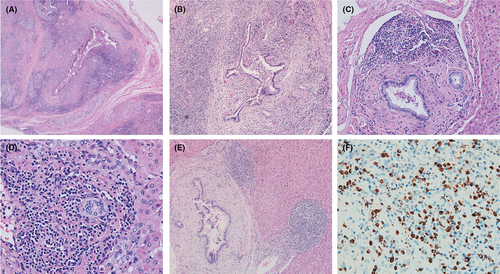
Therefore, the right hepatectomy and cholecystectomy with hepatobiliary duct formation and high hepatobiliary jejunostomy were conducted. The pathological examination of surgical specimens revealed the manifestation of the IgG4-SC. The portal bile duct was deformed and branched with peripheral fibrosis and massive plasma cell infiltration (Figure 2A,B). The basement membrane of the medium-sized septal bile duct was thickening with the peripheral fibrosis (Figure 2C). Meanwhile, the cholangitis granuloma which was similar to primary biliary cholangitis (PBC) was present in the interlobular bile duct (Figure 2D), and the large bile duct was destroyed and surrounded by concentric fibrosis, while the small bile duct was hyperplasia and surrounded by the inflammation (Figure 2E). The immunohistochemistry revealed infiltration of 40-150 IgG4-positive plasma cells per high-power field in the liver tissue (Figure 2F). Based on the pathological results, this patient was diagnosed with IgG4-SC. After that, our patient underwent colonoscopy, and only a small transverse colon polyp was found. No indication of inflammatory bowel disease was found which further supported the diagnosis of this case.
Corticosteroids (oral prednisolone) are recommended for the initial induction therapy of IgG4-SC, but the initial dosage and the maintenance time are different due to the different reports.8-11 In this case, prednisolone was adapted as treatment. But the dosage and the course of corticosteroids treatment about IgG4-SC with normal serum IgG4 levels had not been recommended yet. So, the initial dosage of this patient was 60 mg/d as a case report reported12 and gradually tapered to 5 mg/d which would be maintained for 6 months. After 1-month treatment of prednisolone, the patient was marked improvement in biochemical test and contrast-enhanced computed tomography imaging. The patient was under follow-up to date.
3 DISCUSSION
IgG4-SC is the most common extra-pancreatic manifestation of IgG4-related disease, but it is frequently associated with autoimmune pancreatitis (AIP), sclerosing sialadenitis, and retroperitoneal fibrosis, but not inflammatory bowel diseases.13, 14 Only few cases are reported to be diagnosed with IgG4-SC in the absence of AIP, which are striking male preponderance and hard to diagnose.13, 15, 16 The IgG4-SC can be divided into four types according to the different stricture regions of the hepatic bile duct.17 Due to strictures of the bile duct that are mainly located in the hilar hepatic area, the patient in our case can be diagnosed with IgG4-SC type 4. Considering the liver pathology, radiological imaging, and absence of the inflammatory bowel disease, this diagnosis was confirmed.
Based on the published literature, the clinical presentation of IgG4-SC is often misleading, which should be discriminated from other biliary tract disease such as cholangiocarcinoma or primary and secondary sclerosing cholangitis.5-7 HISORt criteria, which were developed to diagnose the AIP,18, 19 are currently considered as the diagnostic criteria of IgG4-SC. The HISORt criteria form the cornerstone in the diagnosis of IgG4-SC, combining histopathological (H), imaging (I), and serological (S) features including serum IgG4, other organ manifestations (O) of IgG4- related disease, and response to treatment (Rt).18, 19 But some articles reported that the serum IgG4 was slightly elevated or even normal in the IgG4-SC patients who did not have the pancreatic lesions.15, 16 Therefore, the HISORt criteria are limited, especially when the clinical and experimental manifestations are not typical. As in our case, according to the criteria mentioned above, it was hard for us to distinguish from cholangiocarcinoma without the histology evidence. Therefore, the histology is the gold standard19 in atypical patients, and liver biopsy before surgery may be a better way to avoid unnecessary surgery.
As it is reported in our case, serum IgG4 levels of this patient are not elevated. To find the function of the IgG4, some article revealed that the IgG4 had an anti-inflammatory effect in type I, II, and III hypersensitivity reactions.20, 21 In contrast to these classical autoimmune diseases with severe organ damage, IgG4-related disease showed relatively weak immune responses because of the abundant protective IgG4 in IgG4-related disease alleviates the inflammatory damage.22 But it is hard to explain why the serum IgG4 levels are normal in some isolated IgG4-SC. Further investigations are needed. Moreover, an elevation of serum IgG4 levels is not specific for the diagnosis of IgG4-SC. Cholangiocarcinoma and PSC cannot be excluded solely based on an elevation of serum IgG4 levels.8
The main treatment of IgG4-SC is corticosteroids (oral prednisolone), which was recommended by many studies and induced a rapid remission.2, 3, 8-11 According to different studies, the started dosage of prednisolone is 0.6 mg/kg/d,8 20-30 mg daily,10 or 40-60 mg daily,9 gradually reduce to a dosage of 5 mg/d and maintain for 0.5-3 years.8, 11 In our case, after taking the oral prednisolone, the direct bilirubin, alkaline phosphatase, and γ-glutamyl transferase of this patient gradually returned to normal, which confirmed the effectiveness of prednisolone. As for other drugs, there are also some studies mentioned immunomodulator treatment in IgG4-SC; for example, rituximab is shown to be effective in IgG4-SC and is suggested under the circumstances of incomplete remission or corticosteroids dependency.23, 24 However, the immunomodulator do not have reliable data in the induction of remission in the first-line or second-line IgG4-SC treatment.23 The remission rate of corticosteroids treatment is very high,25 and approximately 50%-70% of the patients will relapse.10, 25-27 Therefore, long-time follow-up of IgG4-SC is required.
4 CONCLUSION
In conclusion, isolated IgG4-SC is difficult to diagnose, especially when the serum IgG4 levels and pancreatic imaging findings are normal. Liver pathology is essential to the diagnosis of this type of IgG4-SC. Therefore, to avoid unnecessary surgery, we should cautiously diagnose it by liver biopsy. Corticosteroids are the most effective treatment, and immunomodulator, like rituximab, can be used as a supplement of corticosteroid treatment.
ACKNOWLEDGMENTS
The authors acknowledge the patient for providing consent to share the case.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
YS: involved in data collection and drafting of the manuscript. JC: collected the images of the MRI. JY: managed the patient. XP: analyzed the pathologic pictures and revised the manuscript. All authors read and approved the final manuscript.
ETHICAL APPROVAL
This case was approved by Ethics Committee of Tongji Medical College, HUST, and published with written consent of the patient.