Secondary syphilis mimicking sarcoidosis
Abstract
Secondary syphilis may mimic sarcoidosis due to atypical clinical and pathological presentations. Differential diagnosis of these two is critical since the clinical courses and treatments are different. Highly clinical suspicion and utilization of confirmatory tests in high-risk patients are the key for the differential diagnosis.
1 INTRODUCTION
The overall number of reported primary and secondary syphilis cases in the United States increased significantly in recent years.1 The rise in the rate of reported syphilis cases is primarily attributable to increased cases among men who have sex with men (MSM) and due in part to risky sexual behaviors, which are significant risk factors for coinfection of human immunodeficiency virus (HIV). Data from the United States Centers for Disease Control and Prevention suggest that approximately 42% of MSM and 8% of men who have sex with women with primary and secondary syphilis are coinfected with HIV.2
Syphilis has been reported to exhibit atypical clinical and serological courses in patients that are coinfected with HIV.3 We present a case report of secondary syphilis with skin rashes and renal dysfunction that mimics sarcoidosis due to atypical clinical and pathological presentations.
2 CASE REPORT
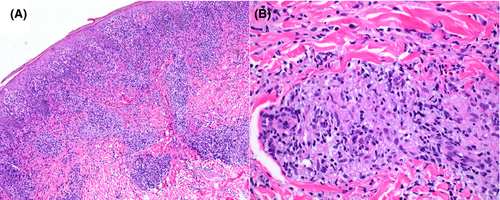
A 24-year-old heterosexual man with a recent diagnosis of HIV infection presented for his first HIV visit upon referral from his primary care physician. He reported a nonpruritic, nonpainful rash on the upper arms with progression to the face, bilateral upper thighs, and scrotum for 2 months. A biopsy of the skin rash from outside institution revealed non-necrotizing granulomatous inflammation consistent with sarcoidosis (Figure 1). He was treated with steroids for 1 week with no response.
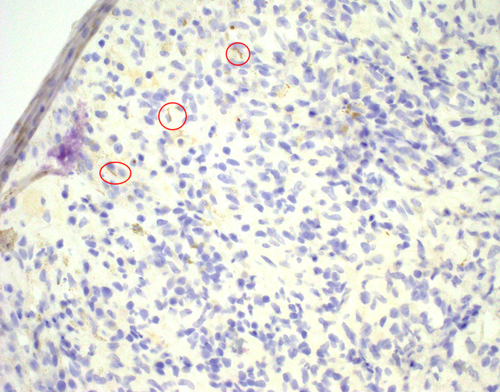
Skin examination revealed indurated papules with a rubbery texture across the lower legs, upper thighs, arms, back, scrotum, soles of the feet, and perioral area. Occasional lesions were annular or macular with intermittent fine scales. As part of the routine evaluation of a new HIV-infected patient, rapid plasma reagin (RPR) test was performed and showed a titer of 1:512. Complete chemistries and metabolic panel were within normal limits other than elevated protein in the urine. The patient was treated with one injection of Bicillin 2.4 million units. The initial skin biopsy was reviewed in our institution, and immunohistochemical stain for Treponema pallidum was then performed and positive (Figure 2). The skin biopsy block was also sent to CDC for T pallidum PCR test, which confirmed the diagnosis of secondary syphilis.
Full resolution of his rash was noted on follow-up visit. RPR titer decreased from 1:512 to 1:64 at 6 months post-treatment with no recurrence of skin lesions. His proteinuria resolved within 1 month after treatment.
3 DISCUSSION
Syphilis has long been known as the “great mimicker” due to the rapid and system-wide vasculitis caused by endothelial invasion of T pallidum.4 This vasculitis and systemic spread occur rapidly after primary infection and mark the beginning of the stage known as secondary syphilis. Rash is one of the most readily observed hallmarks of secondary syphilis. The rash is typically described as macular-papular but endless variations have been described including nodular, annular, pustular, nodulo-ulcerative, and framboeisform.5 Biopsy specimens from the rash often show chronic inflammation with abundant plasma cells; however, atypical findings including granulomatous inflammation with only few plasma cells as presented in the current case can make the diagnosis challenging. These atypical pathologic findings show great similarity with sarcoidosis which is a common granulomatous disease and can present with skin rash.
The skin is only one of the organ systems that syphilis can affect. Renal dysfunction such as was present in our patient is common. Disease manifestations may range from subclinical proteinuria to frank nephrotic syndrome.6, 7 The clinical presentation of secondary syphilis overlaps with some autoimmune diseases. Sarcoidosis is a common granulomatous disease affecting multiple organ systems including the skin and kidneys.8, 9 It has been known itself to mimic other diseases and be difficult to diagnose. Common to this theme, syphilis has been misdiagnosed as a range of autoimmune diseases including Behcet's disease,10 lichen planus,11 and inflammatory bowel disease.12
US guidelines for syphilis diagnosis recommend use of a nonspecific test such as the rapid plasma reagin combined with a T pallidum-specific test for confirmation.13 These tests have imperfect sensitivity and specificity depending on comorbid disease and may still leave doubts as to true diagnosis. When tissue is available, histopathology can aid in diagnosis. Darkfield microscopy is no longer widely available given the need for training and experience. Silver stains, such as the Warthin-Starry, are a common stain to identify spirochetes but have a sensitivity of <50%. Commercial immunohistochemical stains comprised of antibodies specific to T pallidum are now available with improved sensitivity than that of silver stains. Sensitivity is highest when used in conjunction with PCR testing.14-16
In conclusion, we presented a case of secondary syphilis mimicking sarcoidosis due to atypical clinical and pathological presentations. Differential diagnosis of these two diseases is critical since the clinical courses and treatments are different. Highly clinical suspicion and utilization of confirmatory test in high-risk population is the key for the differential diagnosis.
ACKNOWLEDGMENT
Consent statement: Published with written consent of the patient.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
WL: drafted the manuscript. EB and CM: presented the case and revised the manuscript. EP: investigated the case and revised the manuscript.