Chinese expert consensus on an innovative patient-centered approach to diagnosis and treatment of cancer
Hongnan Mo and Ruiqi Zhong contributed equally to this study and shared the co-first authorship.
Abstract
Patient-centered care (PCC) is an innovative approach to the diagnosis and treatment of malignancy that aims to improve patients' experience during the management of their disease. However, despite growing interest, the concept and specifics of PCC remain unclear. This consensus document addresses this gap by providing a literature review and a clear definition of PCC and outlines its main components as observed in real-world practice. These components include daytime diagnostic and treatment procedures, in-hospital and community-based infusion centers, home-based diagnostic and treatment services, smart healthcare solutions, and integration of traditional Chinese medicine. This document delves into the implementation of PCC and explores its potential benefits.
Abbreviations
-
- CDT
-
- convenient diagnosis and treatment
-
- DDT
-
- daytime diagnosis and treatment
-
- EBM
-
- evidence-based medicine
-
- MDT
-
- multidisciplinary team
-
- PCC
-
- patient-centered care
-
- PROs
-
- patient-reported outcomes
1 INTRODUCTION
The Central Committee of the Communist Party of China and the State Council implemented the “Healthy China 2030” plan on October 25, 2016, with the aim of promoting the Healthy China Project and enhancing the well-being of the Chinese population. The outline emphasizes the need for comprehensive management of chronic diseases to be available for the entire population throughout their lifespan and aims to increase the overall 5-year survival rate for patients with malignant disease by 15% by the year 2030. Cancer is one of the major health concerns worldwide. Notably, China has consistently had the highest incidence of cancer and cancer-related mortality worldwide, with a staggering 4,820,834 new cases and 3,208,516 cancer-related deaths in 2022 [1].
Current medical services for patients with cancer have several main features. First, diagnosis and treatment take place primarily in large tertiary hospitals, while primary and secondary hospitals contribute only a small fraction of these services. Second, as a result of technological advances in diagnosis and treatment, cancer has gradually become a chronic disease for which patients often need to undergo multiple rounds of chemotherapy, radiotherapy, biological therapy, and other treatments and require long-term follow-up. Third, treatment of cancer is becoming increasingly specialized. Fourth, treatment may be associated with adverse reactions that require intensive monitoring and timely intervention. Fifth, therapeutic strategies for cancer are evolving rapidly. Therefore, patients diagnosed with cancer are required to travel frequently to larger medical facilities to undergo standardized treatment and assessment. However, factors such as travel-related fatigue before and after treatment, registration and examination procedures, and the requirement for nursing care during treatment impose a heavy financial burden and physical and psychological stress on patients and their families and may affect their compliance with treatment and its outcomes.
Patient-centered care (PCC) is an innovative approach to diagnosis and treatment. This approach is consistent with the objectives of the Healthy China Project, one of which is to provide safe and effective treatment for patients with cancer, address additional needs that may arise during treatment, improve the quality of medical care, and facilitate the rational allocation of medical resources. However, there is currently no standardized definition of PCC. Some of the definitions offered in previous studies have emphasized the need for active involvement of patients in healthcare discussions and decision-making in order for services to align with their values and maximize their satisfaction with treatment [2]. Other studies have defined PCC as a people-oriented approach that entails the provision of optimal diagnostic and treatment procedures and care for patients with cancer based on solid evidence and practices that aim to prolong patients' survival and alleviate their physiological and psychological distress [3, 4].
In current global clinical practice, PCC for patients with cancer takes place primarily in daytime care centers (including ambulatory clinics, day-stay surgery, and ambulatory wards), infusion centers (both within and outside the hospital setting), home-based medical services, and internet-based healthcare.
To promote the development of PCC and serve patients better, we have engaged in in-depth discussions with experts to identify consensus issues, independently collected experts' opinions by questionnaire, and summarized the key insights. This consensus document aims to clarify the concept, operation, and management of PCC and related issues in China and provides a reference for research on PCC and its implementation.
2 CONCEPTS/APPROACHES TO DIAGNOSIS AND TREATMENT OF CANCER: CURRENT STATUS AND TRENDS
2.1 Transition from a disease-centered approach to a patient-centered approach
2.1.1 Evolution of concepts and approaches to diagnosis and treatment of cancer
Historically, lack of awareness about screening for cancer and limited diagnostic techniques often resulted in the discovery of the disease in its late stages, resulting in predominantly palliative treatment. Technological advances in diagnostics, local and systemic treatments, and surgery have enabled earlier diagnosis and more effective treatment. Consequently, there have been notable improvements in survival rates and quality of life in patients with late-stage cancer. At the same time, the medical service approach for patients with cancer has undergone a shift from single-discipline to multidisciplinary teams for evaluation and treatment and a transition from centralized services in large hospitals to services across multiple medical facilities. The shift to multidisciplinary teams focuses on disease-centered care, while the latter marks a shift from a disease-centered approach to PCC. Disease-centered care and PCC are compared in Table 1. In brief, disease-centered care aims to provide comprehensive treatment for cancer by teams at general hospitals, whereas the PCC approach aims to meet the needs of patients that arise during treatment, improve their quality of life, and provide cost-effective healthcare services by building a better healthcare system, improved policies, and utilization of social support systems. Under the premise of ensuring that patients receive reasonable treatment, PCC is not only more convenient for patients than the disease-centered care approach but also promotes further rational allocation of medical resources and more sustainable development of hospitals at all levels.
| Approach | Patient-centered care | Disease-centered care |
|---|---|---|
| Client | Patients and their caregivers | Patients |
| Provider | Healthcare professionals, as well as patients themselves and their caregivers | Healthcare professionals in relevant clinical specialties |
| Stages | Entire process from diagnosis to the end of treatment | Main treatment stages |
| Aim | Treat the disease and improve the quality of life for patients | Treat the disease |
| Focus | Physical and mental health of patients and caregivers | Disease only |
| Direction | Medical services and social support | Limited to the medical field |
| Disciplines | Interdisciplinary, including clinical medicine, nursing, social governance, public health, psychology, economics, and artificial intelligence | Limited to medical disciplines |
2.1.2 Disease-centered approach to diagnosis and treatment and its existing problems
The disease-centered approach to diagnosis and treatment of cancer, which is primarily biomedical, emphasizes effective treatment but often overlooks patients' quality of life, leading to the perception of “doctors seeing diseases but not people.” In the past, doctors have proposed treatment plans for patients based on their specialty, and the emergence of multidisciplinary collaboration has led to more comprehensive diagnostic and treatment procedures. However, this has increased patient dependence on services provided by large hospitals, hindering the development of smaller medical facilities and worsening the uneven distribution of resources for the treatment of cancer.
2.1.3 Measures to tackle problems with the disease-centered approach
The limitations of disease-centered diagnosis and treatment have been recognized in recent years, and there has been an increasing focus on patients and their families. A study of the perceptions of adjuvant chemotherapy in elderly patients with breast cancer found that 58.5% of women preferred to make their decisions about chemotherapy in collaboration with a clinician. Lack of social support is one of the reasons for patients declining chemotherapy.
Research has shown that increasing medical needs and expenses impact the decisions made by patients with cancer and potentially jeopardize the quality of life for themselves and their families. Furthermore, according to several studies on “financial toxicity,” namely, the objective financial consequences of cancer and subjective financial concerns [5-7], this burden affects outcomes for patients, including health-related quality of life, psychological distress, symptom burden, compliance, and even survival [8-12]. Therefore, there is an urgent need for the delivery of more comprehensive and cost-effective medical services for patients with cancer.
The medical community has implemented several effective measures, including daytime diagnosis and treatment facilities, infusion centers (both inside and outside hospitals), home-based services, internet-based medical services (especially for follow-up), extended prescriptions, and expansion of pharmacist services. These measures have markedly reduced the financial burden and inconvenience faced by patients with cancer and reduced the workload of large hospitals to some extent.
At the same time, patient-reported outcomes (PROs) have become an increasing focus of attention in clinical research and follow-up [13, 14]. Unlike objective outcomes, which center on the biological effects of treatment, PROs primarily assess subjective symptoms, feelings, quality of life, treatment-related adverse events and adverse effects, and other patient-related indicators [15]. PROs enable early identification of symptoms and may facilitate timely interventions to improve management [16]. With the introduction of patient feedback interventions in modern oncology practice, several randomized controlled trials have revealed the advantages of PROs. According to a meta-analysis, patients with cancer in whom feedback interventions were implemented reported significantly improved health-related quality of life (Cohen's d = 0.23, 95% confidence interval (CI): 0.11–0.34, p < 0.001) and mental functioning (Cohen's d = 0.14, 95% CI: 0.02–0.26, p = 0.02) in comparison with those receiving usual care [17]. By investigating PROs, we can better understand the needs of individual patients, which may assist doctors and patients to make treatment decisions together and further improve the well-being of patients with cancer. For example, in previous surveys on PROs, some women scheduled for radical mastectomy have reported experiencing severe psychological distress [18]. Such women may prefer neoadjuvant treatment before surgery to increase the likelihood of breast conservation and may benefit psychologically from early arrangements for breast reconstruction surgery. Notably, there has been some research in China in which PROs were used to assess chemotherapy-induced peripheral neuropathy (CIPN) [19, 20]. These studies found that CIPN was more severe in patients who received albumin-bound paclitaxel than in those who received docetaxel. Additionally, patients who had lower pretreatment blood sodium and higher blood chloride concentrations were related to paclitaxel-induced CIPN.
Technological and pharmacological advances in treatment, including drug formulations that can be administered orally or subcutaneously, have created conditions conducive to PCC. Many patients with cancer can now receive medication in a more convenient setting within a shorter timeframe, thereby improving their satisfaction with treatment. These advances have also contributed to the development of a tiered diagnosis and treatment system, whereby patients in good condition can have their chemotherapy drug injections completed in primary hospitals so that the medical resources of tertiary hospitals can be made available to more patients in need.
2.1.4 Recent policies, consensus documents, and guidelines
Several recently published expert consensus documents have played a role in shaping policies relevant to PCC. In 2021, the General Office of the State Council issued the “Opinions on Promoting the High-Quality Development of Public Hospitals,” which proposed daytime surgery to improve the utilization of medical resources. Daytime diagnostic and treatment procedures, which refer to a novel medical approach whereby patients are diagnosed and treated in the hospital during the day and return home at night, are now available at approximately 60% of tertiary hospitals in China. On November 23, 2022, the National Health Commission released the “Provisional Regulations on the Quality Management of Daytime Medical Care in Medical Institutions,” which outline the basic requirements for daytime medical care. In the same year, the “Chinese Expert Consensus on the Operation and Management of Daytime Operating Rooms in Comprehensive Hospitals (2022 Edition)” was published, presenting policies aimed at regulating daytime operating rooms [21]. Before these publications, documents such as the “Consensus of Anesthesiologists for Daytime Surgery” [22], “Expert Consensus on Postoperative Analgesia in Adult Daytime Surgery” in 2017 [23], “Expert Consensus on Standardized Writing of Daytime Surgical Medical Records” [24], and “Chinese Expert Consensus on Day Surgery in Breast Surgery (2021 Edition)” were issued [25]. Following the release of the “Breast Cancer Follow-up and Accompanying Diseases Comprehensive Management Guidelines” in 2019, the “China Cancer Follow up and Health Management Guidelines” was released in 2022, which recommended the use of PROs in clinical practice and recommended different PROs for different patients [26, 27].
The China Oncology Day Diagnosis and Treatment Collaborative Group has released the “Expert Consensus on Day Care Cancer Diagnosis and Treatment in China (2022 Edition)” [28], with the “Shanghai Municipal Hospital Daytime Chemotherapy Management Consensus” being released in 2023 [29]. Numerous supporting expert consensus documents related to PCC have also been published, including the “Expert Consensus and Technical Operation Guidelines for Clinical Application of Implantable Intravenous Infusion Port in Breast Cancer Patients (2017 Version)” [30], “Expert Consensus on Standards and Pathways of Family Pharmacist Services” [31], “Expert Consensus on Managing the Whole Process of Home Care for Pancreatic Cancer Patients in China” [32], and the “Expert Consensus on the Construction and Application of Internet Medical Intelligent Assistance Prescription Review System” [33]. These documents serve as a framework for promoting daytime diagnostic and treatment services for patients with cancer as well as home-based healthcare.
Owing to the increasing demand for daytime chemotherapy services, governments in certain provinces and cities have introduced medical insurance coverage for daytime chemotherapy services. There are four payment methods: project-based, single disease-specific quotas, diagnosis-related groups, and diagnosis intervention packets. Requirements regarding the qualifications of physicians administering daytime chemotherapy and the settings in which it can be provided have also been established [34].
The above guidelines provide a foundation for PCC, including standardization of daytime diagnostic procedures and treatment, guidelines for management of home-based healthcare and the service standards of staff, establishment of smart healthcare, and improvements in health insurance. This consensus document clarifies the basic definitions, core concepts, and key points of service in the PCC approach, describes current challenges pertinent to PCC, and proposes approaches to address these challenges within the current context in China.
2.1.5 PCC and the diagnosis and treatment of cancer
The concept of PCC and how it should be used for the diagnosis and treatment of cancer remain unclear. This section discusses these topics in detail.
2.1.5.1 Definition of PCC for the diagnosis and treatment of cancer
The expert group reviewed existing practices and the relevant research and discussed and formulated the following preliminary definition of PCC in terms of the diagnosis and treatment of cancer.
PCC involves engaging in discussions and developing plans for the diagnosis and treatment of cancer as well as individually tailored long-term management plans. It integrates evidence-based medicine and considers the needs of the patient at the same time as respecting the wishes of the patient and their family members. PCC also considers the patient's social, psychological, and physical circumstances. This approach fully leverages the roles of medical institutions and nursing service personnel at all levels, aiming to maximize the benefits for patients with cancer.
2.1.5.2 Core concepts of PCC in the setting of cancer
In line with the above definition, the core concept of PCC for the diagnosis and treatment of cancer is to prioritize and respect the needs and wishes of patients while adhering to scientific evidence. This can be achieved by effective communication between medical service providers and patients, resulting in the formulation of comprehensive medical service plans. The involvement of medical institutions and healthcare professionals at all levels is integral to the service system, aiming to address the diverse needs of patients throughout diagnosis and treatment.
2.1.5.3 Key components of PCC in the diagnosis and treatment of cancer
The key components of PCC in the diagnosis and treatment of cancer are as follows: (1) accurate multidisciplinary evaluation of the patient's condition; (2) offering treatment options based on evidence-based medicine, explaining in detail the potential benefits and risks; (3) detailed explanation of the financial and living costs associated with the various options; (4) ensuring that patients and their families can make choices regarding treatment based on detailed information provided by healthcare professionals; (5) utilization of daytime and infusion services by hospitals and third-party institutions; (6) maximization of the role of integrated health care systems, community hospitals, and primary healthcare providers in hierarchical diagnosis and treatment; (7) delivery of home-based diagnostic and treatment services by medical institutions at all levels, including third-party facilities; (8) harnessing the potential of advanced treatment technologies; and (9) judicious use of the Internet, smart medical services, and remote follow-up.
2.1.5.4 Exploration of PCC in breast cancer
The PCC approach to diagnosis and treatment has been explored in many types of cancer. For example, China has carried out a number of investigations of PCC in breast cancer. First, China has promoted multidisciplinary diagnosis and treatment. The “Breast Cancer Multi-Disciplinary Diagnosis and Treatment Standards and Norms (2023 Edition)” focuses on patients and has improved the integrated case management capacity of breast cancer in China. Second, most tertiary hospitals in China actively provide daytime diagnosis and treatment services for patients in good overall condition, aiming for a short treatment time and manageable adverse reactions, which improves bed turnover rates and reduces the amount of time patients have to wait for medical treatment. China has also published the “Chinese Expert Consensus on Daytime Diagnosis and Treatment of Malignant Tumors (2022 Edition),” which standardizes ambulatory services so that the diagnostic and therapeutic procedures implemented in ambulatory wards are the same as those in hospitals. Meanwhile, the costs of daytime diagnosis and treatment are now significantly lower than those of hospital ward-based services. Nowadays, daytime surgery, chemotherapy, and medication are covered by medical insurance in many provinces and cities across China, reducing the financial burden on patients with breast cancer. Third, many regions have initiated regional alliances for breast cancer led by specialized or tertiary hospitals. These alliances aim to seamlessly connect medical facilities at various levels, facilitate the distribution of top-tier medical resources, foster the exchange of cutting-edge diagnostics and treatments, advance implementation of standardized diagnostic and treatment protocols for breast cancer, enable bidirectional referral services among hospitals regardless of tier, effectively mobilize medical resources, and improve patients' access to healthcare. Fourth, novel drugs and dosage formulations have been developed, including targeted therapy for patients with HER2-positive breast cancer. These patients were previously treated by intravenous infusions that took several hours. Efficient dual-target subcutaneous preparations have been introduced and can be administered within minutes, thereby enhancing ease of use and saving time. In the future, more novel agents and dosage formulations are expected to improve the treatment of breast cancer further, allowing patients to access safe and effective treatment in primary hospitals and even community hospitals. Fifth, a digitalized and intelligent healthcare system is being implemented. In the past decade, China has progressively advocated for updates to electronic medical records systems and digital archiving of medical data, results, and laboratory reports. In recent years, China has also piloted medical record-sharing projects in 30 general hospitals in Beijing. It has also established breast disease databases in first-tier cities, including Beijing, Guangdong, and Shanghai, with the aims of establishing a big data healthcare system and promoting the sharing of information regarding diagnosis and treatment. The rapid development of artificial intelligence, 5D, big data, the Internet of Things, and other technologies has gradually brought the diagnosis and treatment of breast cancer into the information medicine era. Doctors can deliver online diagnosis, treatment, and long-term follow-up using intelligent software and equipment, and patients can participate in the management of their disease and decision-making throughout their course using this technology. Sixth, in 2023, China launched the “Chinese Characteristic Patient Report Outcome Scale of Breast Cancer (National Cancer Center-Breast Cancer, NCC-BC),” which allows patients to evaluate their present quality of life, efficacy of treatment, adverse reactions, and other conditions by questionnaire. We aim to promote the use of this PRO scale to engage patients in developing treatment plans that take both therapeutic efficacy and quality of life into account, thereby truly practicing PCC.
2.1.6 Application of traditional Chinese medicine in PCC
Four key recommendations are made for promoting the use of traditional Chinese medicine in PCC for patients with cancer.
2.1.6.1 Use of traditional Chinese medicine to improve the efficacy of conventional anticancer therapy and reduce toxicity
In clinical practice, traditional Chinese medicine is used as adjunct therapy for patients with cancer. By utilizing its dialectical system and integrating internal and external treatments, traditional Chinese medicine can effectively alleviate adverse reactions and complications resulting from surgery, chemotherapy, radiation therapy, and targeted therapy for cancer. Furthermore, to a certain extent, it can inhibit the growth of cancer, prolong patient survival, improve performance status and quality of life, and address both the symptoms and underlying causes of the disease. When integrated with modern medicine, traditional Chinese medicine can help to achieve the objectives of enhanced efficacy and reduced toxicity [35-37]. Researchers have explored the clinical application of traditional Chinese medicine for patients with cancer. A randomized pilot study investigated the effectiveness of Bu-Zhong-Yi-Qi-Tang, a widely used herbal product, in the treatment of cancer-related fatigue. The results indicated that fatigue was significantly less severe in patients treated with Bu-Zhong-Yi-Qi-Tang than in those who were not (−1.1 ± 2.1 vs. 0.1 ± 0.9, p < 0.05) [38]. Another study investigated progression-free survival (PFS) in patients with postoperative recurrence of nonsmall cell lung cancer according to whether they received chemotherapy combined with Shi-quan-da-bu-tang or chemotherapy alone [39]. They found out that the PFS rate was significantly higher in the combination therapy group than in the chemotherapy-only group (p < 0.001). Furthermore, the frequency of adverse events was significantly lower in the combination therapy group (39.1% vs. 81.8%, p < 0.01). These findings suggest that traditional Chinese medicine can enhance the efficacy of chemotherapy in patients with cancer while reducing its toxicity. Large multicenter randomized controlled trials across a broader spectrum of cancers are needed to validate the synergistic and detoxifying effects of traditional Chinese medicine when used in combination with standard oncological treatments.
2.1.6.2 Leveraging the unique advantages of traditional Chinese medicine
Traditional Chinese medicine is based on a distinctive dialectic system. We advocate for the scientific and standardized application of traditional Chinese medicine in the prevention and treatment of cancer, making full use of its clinical advantages of simplicity, effectiveness, and affordability. It is also important to promote eco-friendly therapies, such as acupuncture, moxibustion, and traditional Chinese medicine patches, to reduce the need for complex medications in patients with cancer and mitigate the adverse reactions in the gastrointestinal tract, liver, and kidneys associated with conventional anticancer agents [35, 40].
2.1.6.3 Active use of traditional Chinese medicine to “support the good and eliminate evil”
The fundamental concept of traditional Chinese medicine is based on a holistic perspective and differentiation and treatment of symptoms. This approach has a positive impact on patients with cancer across various stages. Notably, it has demonstrated effectiveness in the treatment of both precancerous and cancerous lesions as well as in the prevention of recurrence and metastasis of cancer. The efficacy of traditional Chinese medicine in the prevention and treatment of cancer lies in the principle of “supporting the good and eliminating evil.” Traditional Chinese medicine is tailored to various aspects during the different stages of cancer, achieving a dynamic balance of yin and yang through its regulatory effect on the body [41-43].
2.1.6.4 Significance of promoting the development of traditional Chinese medicine for PCC
People-oriented differentiation and treatment of symptoms are the essence of traditional Chinese medicine, which aligns with the principles of PCC. By prioritizing the diverse needs of patients and providing a spectrum of treatment options, PCC facilitates the use of traditional Chinese medicine for the diagnosis and treatment of cancer, which is in line with the objectives outlined in the 14th Five Year Plan for the development of traditional Chinese medicine and the goals of the Healthy China Project. This approach also elevates the status and influence of the traditional Chinese medicine industry, as well as fosters its ongoing development [44].
- a.
The mode and concepts of diagnosis and treatment of cancer are evolving toward PCC, aligning with the nationwide Healthy China Project.
- b.
While the disease-centered diagnosis and treatment approach has brought benefits and fostered the development of clinical oncology, its limitations have gradually surfaced. These limitations are evident in the escalating financial burden on patients, inconvenience in their day-to-day lives, and nonrational use of medical resources.
- c.
In response to the evolving paradigms and concepts in the diagnosis and treatment of cancer, corresponding industry norms and medical insurance policies have been progressively introduced. These measures serve as assurances in the development of patient-centered diagnosis and treatment approaches, known as PCC.
- d.
PCC involves discussing and developing plans for the diagnosis, treatment, and long-term management of cancer in collaboration with patients and their families, fully leveraging the role of medical institutions and nursing service personnel at all levels and maximizing the benefits for patients. PCC is based on the circumstances of the individual patient, the principles of evidence-based medicine, and the reasonable needs of the patient. All these components are addressed while respecting the expectations of the patient and their family and their social, psychological, and physical situation.
- e.
The core concept of PCC is adherence to scientific evidence while addressing the needs and preferences of patients. Healthcare professionals and patients communicate to collaboratively formulate medical service plans. This involves integrating medical institutions and healthcare professionals at all levels into the service system to address the diverse needs of patients with cancer during diagnosis and treatment.
- f.
The key features of PCC are as follows:
-
each patient's condition is assessed by a multidisciplinary team;
-
patients are presented with treatment options grounded in evidence-based medicine with a detailed explanation of potential benefits and risks;
-
the financial and living costs associated with different options are considered;
-
patients and their families are encouraged to make informed decisions regarding a rational diagnosis and treatment plan with input from healthcare professionals;
-
daytime infusion services offered by hospitals and third-party institutions are maximized;
-
the capabilities of integrated health care systems, community hospitals, and primary healthcare professionals are harnessed in the hierarchical diagnosis and treatment of cancer;
-
home-based diagnosis and treatment services are promoted by encouraging medical institutions at all levels to offer services, including home visits;
-
the potential of advanced treatment technologies is unleashed;
-
the Internet, smart medical care services, and remote follow-up services are used actively and judiciously.
-
- g.
We recommend the promotion of traditional Chinese medicine in PCC to enhance the efficacy of anticancer agents and reduce their toxicity by adhering to the principle of “supporting the good and eliminating the evil.”
2.2 Convenient diagnosis and treatment (CDT)
CDT is an important aspect of PCC, particularly in the management of patients following major treatment in the hospital. Among the various components of PCC, CDT encompasses the broadest range of medical services and caters to the largest number of people. However, it is also the most vulnerable component of PCC in practice. This section provides a detailed explanation of CDT to enhance understanding of the current situation and related issues in China.
2.2.1 CDT: Definition, services, and approach
There is currently no universally accepted definition of CDT, which is a concept that spans all aspects of clinical medicine. Following discussions by the expert group, CDT has been defined as follows: optimization of medical procedures by qualified medical institutions and professionals in various scenarios, shorter medical procedures, and rapidly implemented medical and nursing services with the aim of enhancing patient convenience. The concept of CDT encompasses the entire process of medical care, from initial entry into a medical institution to completion of diagnosis and treatment. For example, online appointment registration falls within the broad category of CDT.
The narrow definition of CDT used in recent practice primarily includes services offered in centers for daytime diagnosis and treatment, infusion centers within and outside hospitals, home-based diagnosis and treatment, and online medical care. CDT differs from diagnosis and treatment in medical institutions following traditional procedures in that it denotes swift resolution of patients' medical needs.
2.2.1.1 Present difficulties in daytime diagnosis and treatment of cancer
Most tertiary hospitals in China now provide daytime diagnosis and treatment services, including inpatient ward services, surgery, and chemotherapy. Daytime diagnosis and treatment are gradually assuming an increasingly important role in the management of cancer. According to the “Expert Consensus on Day Care Cancer Diagnosis and Treatment in China (2022 Edition),” daytime diagnosis and treatment of cancer are characterized as “short, flat, and fast,” optimizing the use of limited medical resources, reducing the length of hospital stay, decreasing medical expenses, and improving the utilization of hospital beds. Consequently, this approach fosters a win-win situation for both doctors and patients [45].
There is a substantial demand for daytime chemotherapy, but there are significant variations in the structure of daytime chemotherapy systems among institutions and the types of diseases for which they are used [29]. In the United States, 95% of cancer treatment occurs in daytime wards, whereas the proportion of cancer diagnoses and treatments carried out in daytime wards in China is less than 5%. In many regions, daytime diagnosis and treatment are only available as an outpatient service and are not covered by medical insurance, which discourages patients from selecting the daytime option [46]. According to a previous study, the 5-year survival rate of patients with breast cancer in China is at least 80%, with a clinical cure rate that is significantly higher than that of other cancers. However, owing to the uneven distribution of medical resources, some patients with breast cancer encounter difficulties when accessing treatment [45].
2.2.1.2 Infusion centers inside and outside hospitals and related difficulties
Infusion centers originated in the United States, where patients receiving specific drugs can visit individual clinics or direct-to-patient (DTP) infusion centers for infusions or injections. This service optimizes patient medication procedures, shortens the total treatment time, and reduces financial costs. China's first daytime ward infusion center was established in May 2016. Patients do not need to be hospitalized to be able to receive specialized infusion and emergency services at such centers. After infusion and observation, they can return home. The medical costs are 400–500 yuan lower in patients receiving treatment at infusion centers than in those receiving inpatient infusions [47].
Currently, there are three main types of infusion centers: those independently established by a hospital, those jointly operated by a hospital and a third party, and those operated by a DTP pharmacy. The following factors are currently limiting the development of infusion centers: (1) a shortage of qualified doctors and nurses; (2) the cost of supporting the software and hardware required for infusion centers; (3) lack of medical insurance and a related legal policy; (4) the lengthy process required to transfer patients from large or public hospitals to external infusion centers; (5) the uneven distribution of profits in the medical service market; and (6) potential medical risks.
2.2.1.3 Home-based diagnosis and treatment and related difficulties
There is currently a significant demand for home-based diagnosis and treatment services in China. In recent years, these services have experienced rapid growth and gained strong support from the government. On December 14, 2020, the Health Administration Bureau of the National Health Commission highlighted in the “Notice of the General Office of the National Health Commission on Further Promoting the Pilot Work of Internet and Nursing Services” that county medical communities, specialty alliances, telemedicine, secondary and lower-level medical institutions, as well as primary medical institutions should play a more significant role in Internet and nursing services to fully leverage the driving role of high-quality nursing resources in large hospitals and increase the capacity of primary care services provided by urban medical groups.
At present, home-based diagnosis and treatment for patients with cancer primarily involves the management of catheters, administration of certain drugs, palliative care, and psychological and nutritional support, with nursing services as the main components. Although home-based services are very convenient for patients, there are some challenges. First, there are potential risks in terms of legal compliance, determination of responsibility, safeguarding the legitimate rights and interests of patients and healthcare professionals, and supervision of service. Second, ensuring the quality of services provided outside medical institutions is difficult. Third, the costs and benefits of on-site services present a challenge for medical institutions.
2.2.1.4 Online healthcare and its challenges
Online healthcare has undergone rapid development in recent years. The broad definition of online healthcare encompasses all medical-related online services, such as online registration, report viewing, and medication purchases. The narrow definition, on the other hand, involves connecting doctors/nurses and patients through the Internet, conducting consultations, issuing prescriptions, answering medical and nursing questions, guiding patients in rehabilitation or cooperation, and monitoring their condition.
The evolution of online healthcare in China can be roughly divided into three stages: website consultations, virtual hospitals, and mobile Internet [48]. Online medical care facilitates the continuous medical attention required by patients after discharge from the hospital, especially in terms of managing their condition during follow-up after surgery or hospitalization. By using online services, patients can avoid traveling between home and hospital, thereby conserving hospital resources. However, there are several current challenges associated with online healthcare. First, there is a risk of leak of patient information. Second, non-face-to-face diagnosis and treatment may result in incomplete or inaccurate information being obtained, posing significant risks to medical safety. Third, in some regions, despite medical insurance support, many restrictive conditions remain that need optimization and strengthening.
2.2.2 Regulations, government policy support, and relevant consensus/guidelines
The relevant policies and expert consensus for CDT have been outlined in detail in Section 2.1.4. However, deficiencies persist in the realm of supporting laws, regulations, and industry norms. We call upon the relevant government departments and organizations to devise appropriate laws and regulations as soon as possible. We also urge medical professionals to proactively establish relevant norms, consensus, and guidelines to regulate CDT effectively. This proactive approach will enable preventive measures to safeguard patient's lives and health, fostering the orderly development of CDT.
- a.
CDT includes various diagnostic and treatment activities performed by qualified medical institutions and professionals in various scenarios that facilitate patient recovery, optimize medical procedures, shorten medical procedures, and provide rapid medical services. CDT is an integral component of PCC.
- b.
CDT encompasses the entire process of medical care from initial entry into a medical institution to completion of treatment.
- c.
In recent practice, the narrow definition of CDT primarily includes services provided in centers for daytime diagnosis and treatment, infusion centers inside and outside hospitals, home-based diagnosis and treatment, and online medical care.
- d.
The narrow definition of CDT differs from the traditional diagnosis and treatment procedures performed in medical institutions in that it refers to a swift resolution of patients' medical needs by specific diagnostic and treatment procedures.
2.2.3 Current challenges in the diagnosis and treatment of cancer
In recent decades, China's medical capacity has continuously developed, and medical insurance policies now essentially cover the entire population. However, some problems remain to be solved.
The current challenges in cancer diagnosis and treatment are two-fold. First, there is a need to enhance the utilization of medical resources. Large hospitals are currently overcrowded, while many empty beds are available in primary hospitals. Healthcare professionals in large hospitals are overloaded with work, while those in primary hospitals lack experience, especially in departments that treat severe or difficult cases. Furthermore, community-based medical institutions lack diagnostic and treatment services. Second, there is a requirement to improve patient satisfaction, especially for those with cancer. Such patients often experience both physical and psychological illnesses and are prone to adverse experiences that exacerbate their condition during diagnosis and treatment because of the inconvenience of services. In particular, the quality of life of patients significantly decreases during prolonged treatment, which can lead to reduced compliance with treatment and ultimately affect the prognosis.
Patient needs can be summarized as the desire to receive high-quality medical services while maintaining a reasonable quality of life. The development of services and practices in recent decades means that medical services for cancer can be appropriately allocated among treatment centers. The diagnosis and initial treatment can be performed at major hospitals, and subsequent treatment can be provided at local primary medical institutions. This ensures the quality and continuity of medical services and reduces the adverse impact on the quality of life for patients.
- a.
Currently, the primary issues in cancer diagnosis and treatment include a low rate of use of medical resources and a substantial burden on patients, which adversely affect the quality of medical services and the prognosis.
- b.
Patients' needs can be summarized as a desire to receive high-quality medical services while maintaining a reasonable quality of life.
3 PROMOTION OF INNOVATIVE APPROACHES TO DIAGNOSIS AND TREATMENT OF CANCER IN LINE WITH CHINA'S CURRENT CIRCUMSTANCES
The main purpose of PCC as described in this consensus document is to prioritize patients' needs and resolve the problems of current medical practice in China. PCC aims to facilitate the rational allocation and use of medical resources, ensure the quality of work in large hospitals, foster the development of primary hospitals, enrich and improve the continuity of medical care in the community, and reduce the burden on patients receiving repeated medical services in large hospitals. This approach ultimately enhances patient compliance and improves their quality of life. After discussion by the expert group, this consensus document makes the following proposals for how PCC can be adapted to China's current circumstances.
3.1 Promote the establishment and popularization of CDT
3.1.1 Daytime diagnosis and treatment centers
At present, daytime diagnosis and treatment centers mainly provide surgery, chemotherapy, targeted therapy, and follow-up. Their fundamental setup and management focus predominantly on chemotherapy services. Unified or specialized daytime diagnosis and treatment centers can be established according to the size and specialty of each hospital. Daytime surgery for cancer has also been promoted and achieved promising outcomes by following the current regulations and consensus. This subsection outlines some of the features of these centers.
3.1.1.1 Equipment
The hardware configuration of daytime cancer diagnosis and treatment centers is essentially identical to that of inpatient wards. Namely, conventional medical facilities, instruments and equipment, and emergency supplies must be accessible and kept in good condition for use at any time. The environment should be appropriately designed to improve the experience of patients during treatment. Some hospitals have been granted access to anticancer agents at their daytime diagnosis and treatment centers.
3.1.1.2 Personnel
Centers are often administered and operated by a hospital or a related department, and permanent administrative personnel should be appointed for human resource management. It is possible to set up an attending doctor or specialist to serve patients. Nursing should be provided by resident personnel with adequate experience and qualifications in caring for patients with cancer.
3.1.1.3 Patients
Most hospitals that set up daytime diagnosis and treatment centers have set admission standards for patients, not only ensuring that patients who meet the standards can receive convenient and timely services but also greatly reducing medical risks.
3.1.1.4 Administration
Multiple units have developed clear regulations for daytime medical records, which are currently being explored. The overall principle is to accurately record all the necessary data in a timely manner and include all relevant procedures, including obtaining informed consent. Information platforms or modules for daytime diagnosis and treatment centers can be integrated into existing medical and nursing information platforms. Alternatively, the existing electronic medical records system can be used for 24 h discharges.
3.1.1.5 Medical insurance
Some local policies have included hospital-based daytime diagnosis and treatment services within the scope of medical insurance reimbursement, but this requires further exploration. Centers are advised to communicate fully with regulatory and medical insurance departments before providing daytime diagnosis and treatment services.
It should be emphasized that the setting of a daytime operation room should be the same as that of an inpatient operating room. Daytime diagnosis and treatment centers should incorporate reasonable first-aid processes, devise plans for handling adverse events, and regularly conduct first-aid and fire emergency drills. Medical nursing services in daytime diagnosis and treatment centers should be included in the hospital's quality control procedures. Daytime diagnosis and treatment centers can assist with follow-up, health education, and other activities for patients with cancer to complement those of hospitals and their departments, thereby providing holistic care.
3.1.2 Infusion centers inside and outside hospitals
Medical institutions and retail pharmacies at all levels in China have a wide geographical coverage, providing a solid foundation for administering infusion services. In response to the increasing demand for infusion, infusion centers need to have multiple modes of operation to enable patients to receive services. There are three types of infusion centers. First, independent infusion centers set up by medical institutions can provide convenient infusion services for nearby residents or other patients who would be seriously inconvenienced by hospitalization because they rely on the well-established infrastructure and service standards of medical institutions. Second, medical institutions and third parties can jointly establish out-of-hospital infusion centers equipped with the necessary software and hardware facilities, in particular, adequate first-aid equipment and qualified practitioners. These centers service nearby residents, and suitable locations can be chosen to meet the needs of the local population. The qualifications of third parties should be confirmed by the health administrative department. Third, DTP pharmacies can set up infusion centers internally. In view of the large number of retail pharmacies, it is necessary to set up DTP internal infusion centers rationally according to the demand for infusion services among nearby residents and the number of local DTP pharmacy branches to avoid wasting resources. For patients receiving infusion out-of-hospital, medical insurance policies should provide support. In particular, when patients who were previously hospitalized to receive infusion switch to out-of-hospital infusion, medical insurance should partially reimburse the patient, which would encourage patients to choose out-of-hospital infusion, reduce their medical insurance expenses, and lessen the burden on hospital medical services. It is recommended that government departments expedite guidance to clearly define the nature, qualifications, establishment, and supervision of out-of-hospital infusion centers to promote their development.
3.1.3 Home-based services for the diagnosis and treatment
Patients with cancer that can potentially be cured often require long-term adjuvant, maintenance, and supportive therapy as well as regular follow-up after completion of critical treatment. Similarly, patients with noncurable cancer need supportive, palliative, and psychological therapy. Hospitals usually do not have sufficient resources to provide these treatments, leading to a sharp increase in costs for patients. Some of these treatments are simple, easy to implement, and safe, such as care for tubing and wounds, injections of analgesics, blood sampling during follow-up, and palliative care for patients with advanced cancer. All of these can be implemented in the patient's home [32, 49-53]. The large number of new cancer cases and the current situation of treatment in China indicate that there is a substantial demand for home-based diagnosis and treatment services [54, 55].
Although the demand for these services remains an urgent need for many individuals, the establishment of relevant policies and formulation of regulations require research, discussion, formulation, and publication. At present, there is a lack of specific laws and regulations that provide detailed guidance for home-based diagnosis and treatment services for the elderly. The existing policies are mainly aimed at home-based services. There is also no specific text for clinical medical care services. Only in “Action Plan for Further Improving Nursing Services (2023–2025)” issued by the National Health Commission are they mentioned: “(XII) Expand internet and nursing services… Further expand the coverage of internet and nursing services, gradually increase the number of internet and nursing services of medical institutions and the number of home nursing services to benefit more people” and “(XVI) Strengthen the staffing of nurses… We should effectively strengthen the staffing of nurses in primary medical institutions based on clinical nursing needs and the needs of residents in the jurisdiction for home nursing services and focus on increasing the supply of primary nursing services.” Therefore, the development of current home-based diagnosis and treatment services should be approached with flexibility and gradual exploration, considering local laws and regulations, industry norms, and guidance from regulatory authorities.
At present, home-based diagnosis and treatment services for patients with cancer have the following main roles: hospice care, including skin care, pain management, nutritional support, and psychological support; postoperative wound care and implanted catheter management; management of medication to be taken in the home; supervision and assistance with rehabilitation; and extension of prescription services. Home-based medical services have significantly improved the quality of life of patients while reducing the cost of treatment.
Therefore, in response to the current needs and problems experienced by patients, we suggest that relevant policies be introduced at the national and provincial levels as soon as possible to provide support and guidance for CDT and that corresponding laws and regulations be introduced to protect both patients and clinicians. At the same time, business documents and guidelines should be drafted based on the early consensus of multiple stakeholders in home-based services to systematically regulate CDT and help clinicians provide services. We recommend establishing a joint supervision system by the supervisory, regulatory, and business entities. This joint approach aims to enhance the quality of CDT services as well as protect both patients and clinicians.
CDT is an example of hierarchical diagnosis and treatment. Medical institutions and practitioners at different levels can provide various types of CDT. Comprehensive and specialized hospitals have the capacity to establish dedicated daytime diagnosis and treatment centers at both the hospital and department levels. These centers should provide high-level CDT services as well as guide and support in-home services. Primary hospitals can set up daytime diagnosis and treatment centers, provide door-to-door services, and offer CDT services for nearby residents. Similarly, community hospitals and individual clinics can also provide door-to-door services for patients, ensuring accessibility to care in their respective communities.
3.1.4 Smart healthcare
Smart healthcare can be described as the in-depth application and practice of advanced Internet of Things technology in medicine and health, enabling interactions between patients, healthcare professionals, medical institutions, and medical equipment. This technology can facilitate a gradual movement from disease treatment to prevention and from traditional medicine to digital medicine and then to information medicine to meet people's personalized medical needs [56]. Smart healthcare includes a smart hospital system, a regional health system, and a home-based health system [56]. Smart healthcare actively manages various medical activities, greatly improving their efficiency and accuracy, and is one of the highest levels of information technology used in medicine and health [57]. Policies designed to advance the development of smart hospitals by integrating medical and industrial projects that utilize 5G, artificial intelligence, big data, and the Internet of Things have been introduced. Hospital intelligence has become an important support tool for modern hospital and patient management and for promoting a hospital information infrastructure and high-level developments. Article 49 of the Basic Medical and Health Promotion Law of China stipulates that the state should promote the informatization of public health and use information technology to popularize and share high-quality medical and health resources. Medical informatization is an important policy in terms of realizing the Healthy China 2030 Plan.
Smart healthcare can play the following specific practical roles in CDT: (1) clinical practice, especially in diagnosis and prediction; (2) follow-up and monitoring, including recording and uploading critical life information by smart terminals worn by patients, which is beneficial for timely detection and handling of adverse events by healthcare professionals; (3) rehabilitation, such as intelligent robots assisting patients with poststroke rehabilitation exercises, and intelligent service platforms assisting patients with chronic diseases in performing long-term rehabilitation exercises at home [58, 59]; and (4) mental health, including collection and processing of diverse mental health data as well as psychological intervention and treatment by artificial intelligence [60], which have been confirmed to yield positive results in multiple studies [61, 62].
3.1.5 Proposed standards for CDT
- a.
It is mandatory for all medical institutions to provide CDT services to patients based on their condition regardless of the level of the institution. Second-level hospitals and above should provide daytime diagnosis and treatment services and, when appropriate, door-to-door services. Community-level hospitals and below should actively carry out home-based services.
- b.
All medical institutions can provide online healthcare services in accordance with local policies.
- c.
All medical institutions should lead or cooperate with other institutions to provide daytime diagnosis, treatment, and infusion services inside or outside the institution.
- d.
When providing daytime diagnosis, treatment, and infusion services, the center should meet the standards of an inpatient ward and be equipped with the necessary facilities and equipment, including but not limited to oxygen, electrocardiographic and oxygen saturation monitoring devices, emergency vehicles, defibrillators, and suction devices.
- e.
When carrying out online medical services, it is necessary to strictly follow the medical guidelines. This involves obtaining a detailed understanding of the patient's condition and needs and providing reasonable nursing guidance.
- f.
When providing home services, reasonable medical care services should be provided that are based on the condition of the patient, and detailed records should be kept.
- g.
All convenience services should comply with relevant laws, regulations, industry norms, and diagnosis and treatment routines as practiced in China.
- h.
Professionals providing all convenient services, including online medical services, should be appropriately qualified and required to strictly follow medical guidelines to provide appropriate treatment and guidance to the patient.
- i.
All convenient services should be provided after sufficient consideration by medical institutions according to local conditions to avoid wasting financial and medical resources.
- j.
Authorities and relevant medical institutions should actively promote CDT.
- a.
The core principle of CDT is that each hospital can provide flexible and diverse CDT for patients according to its circumstances. These services include daytime diagnosis and treatment centers, infusion centers (inside and outside the hospital), integrated health care systems, community hospitals, and home-based nursing care.
- b.
The hardware configuration of daytime cancer diagnosis and treatment centers should be the same as that of inpatient wards. Conventional medical facilities, instruments and equipment, and emergency supplies must be accessible and in good condition for use at any time. Personnel should be flexibly configured and regularly trained to ensure high-quality daily management and professional service.
- c.
There is a high demand for home-based diagnosis and treatment of cancer. Support by policies, regulations, and medical guidelines or consensus documents is urgently needed.
- d.
CDT can significantly improve the quality of life and reduce treatment costs in patients with cancer.
- e.
More specific supportive policies, laws, regulations, and medical guidelines or consensus documents should be adopted as soon as possible.
- f.
Smart healthcare involves use of advanced Internet of Things technology for in-depth application and practice in medicine and public health, enabling interactions between patients, healthcare professionals, medical institutions, and medical equipment. This technology can facilitate a gradual change of focus from treatment of disease to prevention and from traditional healthcare to digital healthcare to meet patients' personalized medical needs. Smart healthcare includes smart hospitals, regional health, and home-based health systems. Smart healthcare intelligently manages and meets the diverse needs of all personnel in the healthcare field and, owing to its high level of system integration, interconnectivity, and intelligent processing, ensures timely access to preventive and therapeutic medical services, enabling individuals to make the best possible decisions. Smart healthcare is one of the highest levels of information technology used in medicine and health.
- g.
Smart healthcare can be used effectively in a range of applications, including clinical diagnosis, disease monitoring, rehabilitation, and psychological support. It can also improve the quality and efficiency of services at various stages in CDT, reduce the burden on patients seeking medical treatment, and may bring dramatic changes to cancer treatment in the future.
- h.
We call on authorities to formulate policies regarding medical insurance reimbursement and corresponding fee standards that are suitable for CDT, accurately reflect the labor value of healthcare workers, and incentivize healthcare workers to provide CDT.
3.2 Implementing PCC
3.2.1 Basis for implementation
According to our definition of PCC, the reasonable needs and specific conditions of patients are the basis for PCC services. It should be emphasized here that meeting the needs of patients in a reasonable manner does not entail disregarding their specific condition. Given that patients and their families often have a limited understanding of cancer, healthcare professionals should develop a diagnosis and treatment plan based on an objective assessment of the condition, fully communicate with patients and their families, and respect the patient's autonomy in regard to decision-making about their diagnosis and treatment. Healthcare professionals have been continuously developing questionnaires and scales for use in clinical practice to understand the needs of patients. When formulating treatment and follow-up plans for patients, clinicians can reference the patient's preferences to some extent [63, 64]. Overall, PCC should be guided by the diagnosis and treatment guidelines for the disease while considering the wishes of patients and their families.
3.2.2 Process and the main content of PCC
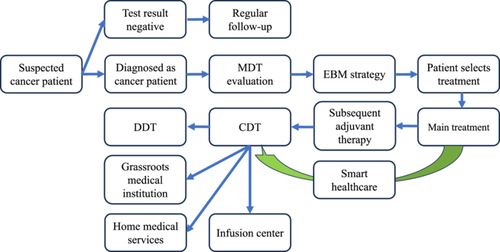
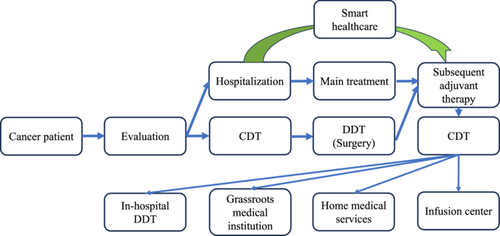
For patients with cancer, PCC involves hospitals, medical institutions, and healthcare professionals at all levels. In terms of primary treatment for cancer, PCC can be roughly divided into curative, palliative, and adjuvant supportive treatment. Curative and palliative treatment are mainly provided in large hospitals, and subsequent adjuvant and maintenance treatments as well as palliative treatment for advanced cancer can be provided by primary medical institutions and by healthcare personnel under the guidance of the oncology department in a large hospital. Therefore, treatment and management plans should be developed to provide PCC for patients with cancer while fully considering the various levels of medical resources required by patients and their families. Patients should receive appropriate care either at a medical facility or in the home according to their needs at different stages of treatment. For example, radical breast surgery is performed in a qualifying hospital, and the first auxiliary treatment after surgery can be delivered in the same hospital. For subsequent auxiliary treatments and follow-up, appropriate medical institutions can be selected near the patient's home, and the required diagnosis and treatment services can be delivered there. During follow-up, if there is a need for home-based nursing, it can be implemented according to the patient's circumstances. Throughout the PCC process, the attending doctor and patient can maintain communication and select appropriate CDT plans and measures. Similarly, for patients receiving palliative treatment, the initial plan can be determined and implemented by specialized healthcare professionals in a main hospital. Subsequent treatments can be delivered efficiently by medical facilities near the patient's home, door-to-door services provided by community medical and health facilities, or nearby clinics. Support during subsequent treatments is recommended, including assistance with mental health and genetic counseling. Figures 1 and 2 summarize the PCC and CDT processes, respectively.
It is important to note that PCC extends beyond the perspective of patients alone. Owing to the highly specialized nature of oncology and the fear commonly experienced when cancer is diagnosed, patients may have limited knowledge about the progress that has been made in cancer therapy. As healthcare providers, we should ensure our communications provide patients and their families with a thorough understanding of the diagnosis, treatment, prognosis, medical expenses, follow-up, and other aspects of their medical experience. We should provide patients with scientifically sound and appropriate diagnosis and treatment plans, communicate the advances in medicine to foster a sense of hope, avoid unnecessary costs, and prevent any significant decline in the patient's quality of life. Importantly, these considerations should be balanced according to the patient's personal experiences and local resources.
3.3 Patient-centered full-cycle health management
In recent years, patient-centered full-cycle health management has received increasing attention. It is an approach to health management that includes the core diagnosis of cancer and its treatment. Its aim is to cover the entire life cycle, seamlessly integrating prevention and screening, early diagnosis, standardized treatment, rehabilitation, and management of quality of life with a PCC approach through interdisciplinary cooperation. Full-cycle management of cancer is structured around three major stages, namely, the precancer stage, acute disease stage (treatment cycle), and postcancer stage (chronic disease) [65]. The precancer stage emphasizes the maintenance of health, prevention and screening for cancer, and promotion of early diagnosis and treatment. The acute disease stage, with hospital treatment as its core, aims to cure the patient or prolong their survival by standardized multidisciplinary treatment. The chronic disease stage is patient-centered and implements interdisciplinary health management. The goal of this stage is to reduce the adverse effects brought about by the cancer itself and its diagnosis and treatment, prolonging survival while emphasizing improvement in quality of life.
The full-cycle management approach focuses on preventing the onset of cancer, raising people's awareness through health education, screening, and early diagnosis and treatment. When cancer is detected, treatment plans are formulated and standardized therapy is implemented. During treatment, healthcare professionals prioritize achieving a high cure rate and longer survival, regularly collect PRO information, focus on improving the quality of life for patients, and effectively manage concomitant diseases. After treatment, rehabilitation and quality-of-life management are implemented to help patients recover their physical and mental health and reduce the risk of recurrence, metastasis, and disease progression. With the development of the full-cycle management approach, many new interdisciplinary fields have emerged, including cardiovascular oncology, onco-nephrology, and onco-fertility [66-68]. The all-round and full-cycle health management approach to PCC is developing rapidly and has made significant progress in the field of breast cancer [65]. Furthermore, disease management specialists are expected to play an important role in PCC for patients with cancer [69, 70]. With the continuous evolution of medical concepts and technological innovation, an increasing number of medical institutions are shifting their focus from treatment of a single disease to the comprehensive health needs of patients.
- a.
PCC should be based on the reasonable needs and specific circumstances of patients, and PRO and patients' preference are important references.
- b.
PCC services should be multilevel and continuous. Medical institutions and personnel at all levels should continuously provide high-quality medical services to patients. Doctors and patients can play a leading role in the main treatment, and other healthcare personnel should actively cooperate.
- c.
PCC does not mean making decisions solely based on patients' wishes. Reasonable demands of patients should be fully integrated with science to reflect both advances in medicine and care at the human level.
- d.
The patient-centered, full-cycle health management approach regards diagnosis and treatment as the core while emphasizing the full process of intervention from cancer screening to final hospice care. This approach aims to provide patients with high-quality medical and nursing services throughout the course of their disease in line with the Healthy China Project.
4 BENEFITS OF PCC
4.1 Effect of PCC on patients
Patients with cancer often experience physical and mental distress, including pain, fatigue, a decrease in physical performance status, and adverse psychological reactions, stemming from the disease itself or the side effects of treatment. They also face significant financial burdens related to travel and the costs of medical treatment, which makes it difficult for patients with cancer to attend hospital for medical services. Consequently, treatment can be a very negative experience, with some patients dropping out of regular treatment. However, PCC makes a difference to their medical experience by eliminating tedious processes and reducing the cost and duration of treatment. The results of several studies have confirmed the advantages of PCC. Arjun et al. assessed the safety and cost-effectiveness of the early supported discharge (ESD) approach in 153,996 patients with colon cancer [71]. ESD is an effective care pathway for less disabled patients in that they can be discharged early to undergo further rehabilitation at home, so is similar to PCC. In that study, ESD was associated with a $4500 reduction in costs and a lower rate of nonelective readmissions (adjusted odds ratio 0.74, p < 0.001). Another study evaluated the long-term cost-effectiveness of ESD in stroke patients using quality-adjusted life years and found that the incremental cost-effectiveness ratio of stroke unit care followed by ESD was £10,661 when compared with a general medical ward without ESD care and £17,721 when compared with a stroke unit without ESD (using a cost-effectiveness threshold of £30,000), indicating that ESD is a cost-effective strategy [72]. Several Chinese researchers have also explored the application of PCC in China. In a report by Tao et al., the average length of stay in a tertiary hospital was 1.83 days for daytime chemotherapy and 4.3 days for chemotherapy in a general medical ward [73]. Implementation of daytime chemotherapy reduces the length of stay significantly, reducing the waiting time to less than 2 days. Furthermore, Lin et al. compared length of stay, cost, outcomes, incidence of adverse events, and patient satisfaction between daytime treatment and treatment in a general medical ward [74]. The results showed that the average length of stay was 2.26 days in the surgical oncology day unit and 4.04 days in the general surgical oncology ward. In terms of average cost, patients in the surgical oncology day unit spent 5682.70 yuan and those in the general surgical oncology ward spent 6124.30 yuan (p < 0.001). In addition, patients were more satisfied with daytime management and their treatment outcomes (97.20% vs. 90.60%, p < 0.05). However, there was no significant difference between daytime treatment and treatment in the general ward in terms of outcomes and incidence of adverse events.
PCC integrates tertiary hospital, primary hospital, community hospital, and home-based care into a convenient medical system that provides patients with the option of receiving effective treatment at various centers in close proximity, which improves their compliance and enables them to receive better medical care services aligned with their diagnosis and treatment plan. A study that analyzed the medication adherence in patients with chronic diseases (diabetes, hypertension, and hyperlipidemia) found that patients who received care in patient-centered medical homes had a higher adherence than those who did not (2.2%, 95% CI: 1.5%–2.9%) [75]. However, research on compliance and adherence with medication in patients with cancer who receive PCC is still relatively limited, and more clinical studies are needed in the future.
4.2 Effect of PCC on hospitals and healthcare professionals
PCC can have a significant diversion effect in that it can divert patients from inpatient wards to daytime diagnosis and treatment centers, from large hospitals to primary hospitals, and from grass-roots hospitals to community hospitals or home-based care. This diversion effect contributes to the development of a tiered system of diagnosis and treatment, addresses the shortage of beds in inpatient departments of large hospitals, and improves bed underutilization in primary hospitals. Therefore, healthcare professionals in large hospitals can devote more energy to patients with greater needs while making primary healthcare professionals available for more patients, thereby achieving a better division of labor in the medical field.
4.3 Effect of PCC on medical insurance costs
patients.PCC can contribute to the control of health insurance costs. Daytime diagnosis and treatment and home-based medical services are effective approaches that considerably reduce medical expenses. Moreover, PCC reduces excessive medical input and indirectly lowers medical insurance costs. Specifically, widespread adoption of the diagnosis-related group/diagnosis intervention packet payment approach encourages a shift of certain treatments to CDT and decreases the overall medical expenses for hospitalized patients, especially nontreatment-related costs. PCC may also lower the overall medical costs by improving the quality of treatment for patients.
- a.
PCC enhances patient convenience by improving the medical experience and quality of life, enhancing compliance, and reducing the cost of treatment.
- b.
PCC optimizes resource allocation within healthcare systems.
- c.
PCC can promote the development of medical institutions and healthcare professionals.
- d.
PCC is beneficial for controlling medical insurance costs.
- e.
PCC has positive physiological, psychological, and social impacts on patients.
5 POTENTIAL CHALLENGES, SOLUTIONS, AND DIRECTIONS FOR PCC
As mentioned already, although novel approaches have been explored and implemented and some consensus documents have been released, there are still many potential challenges and barriers to PCC in real-world practice. First, the ease of implementation of daytime diagnosis and treatment in-hospital and out-of-hospital infusion centers, home-based services, and intelligent medical care varies significantly from region to region. Furthermore, the level and quality of the infrastructure needed for CDT services vary in different regions and hospitals. Second, there is still a lack of standardized regulations and supervision in the field of CDT, including how to establish, operate, and manage medical institutions providing it, how to allocate and select healthcare professionals, and what training is required, all of which pose potential risks in terms of quality and safety of medical services. Third, the medical insurance system needs modifications to adapt to the application of PCC. In many regions and provinces, medical insurance does not yet cover CDT, which increases the economic burden on patients and limits the promotion of PCC.
- a.
The development of CDT facilities, including the transformation of ambulatory chemotherapy centers into daytime diagnosis and treatment centers and the facilitation of outpatient surgery to provide more convenient services for patients with cancer. Implementation of infusion centers both within and outside hospital settings should be expanded while ensuring standardized operational procedures. The capabilities of county-level hospitals with regard to cancer diagnosis and treatment should be extended through medical networks and telemedicine. Community hospitals, health centers, and independent clinics should be encouraged to provide home-based diagnostic and treatment services. The introduction of supportive policies and financial backing from the National Health Commission could boost the engagement of general hospitals and associated medical institutions.
- b.
Norms, policies, laws, and regulations should be formulated as soon as possible. These should outline the criteria for allocating medical equipment, instruments, medications, and first-aid amenities, as well as the qualifications and training needs of healthcare professionals and management personnel to guarantee the safety and efficacy of CDT. There is also a need to monitor the behavior of patients and clinicians, ensuring the protection of privacy and upholding personal rights.
- c.
Medical insurance reimbursement policies and corresponding fee standards for PCC should be established. These should aim to alleviate the financial burden on patients, promote diversion of patients from tertiary hospitals, acknowledge the valuable labor of service personnel, and increase the motivation of healthcare workers to provide the corresponding services.
Currently, PCC is still in the early stages of exploration, and there are no universally recognized principles, including in China. However, with increasing emphasis on the patient experience, we anticipate that PCC will be adopted more widely in the future. We also believe that this approach will have a profound impact on patients' prognosis and psychological status, their families, healthcare professionals, medical institutions, and even on society.
However, the successful implementation of this approach still requires further clinical and sociological research. This consensus is based on previous studies and China's current practical experience with PCC and provides a summary of the associated issues. We hope that it will encourage active participation in PCC by medical colleagues and other relevant personnel. We also call on departments to accelerate the development of relevant laws and regulations, thereby contributing to the realization of the Healthy China Project.
AUTHOR CONTRIBUTIONS
Hongnan Mo: Conceptualization (lead); writing—original draft (equal); writing—review and editing (equal). Ruiqi Zhong: Conceptualization (equal); writing—original draft (equal); writing—review and editing (equal). Fei Ma: Funding acquisition (lead); project administration (lead); supervision (lead); writing—review and editing (supporting).
ACKNOWLEDGMENTS
The authors wish to acknowledge Ziqi Yao and Moyang Xu (4+4 Medical Doctor Program, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China) for their help in translating this research. They also acknowledge the Expert Committee on Cancer Prevention and Control, Healthy China Research Centre for their academic support to this research.
EXPERT COMMITTEE MEMBERS
Shanshan Chen (National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College), Wanyi Chen (Chongqing University Cancer Hospital), Jiuwei Cui (The First Bethune Hospital of Jilin University), Qinglei Gao (Gynaecology and Obstetrics, Tongji Hospital, Tongji Medical College of Huazhong University of Science & Technology), Jihui Hao (Tianjin Medical University Cancer Institute & Hospital), Hai Hu (Zhejiang Cancer Hospital), Sidan Li (National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College), Jing Liang (The First Affiliated Hospital of Shandong First Medical University), Caigang Liu (Shengjing Hospital of China Medical University), Jian Liu (Fujian Cancer Hospital), Xinlan Liu (General Hospital of Ningxia Medical University), Zhenzhen Liu (Henan Cancer Hospital), Zhihua Liu (National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College), Yue Li (The Second Affiliated Hospital of Harbin Medical University), Yuwen Li (West China Hospital of Sichuan University), Haibo Lu (Harbin Medical University Cancer Hospital), Zhenqi Lu (Fudan University Shanghai Cancer Center), Ting Luo (West China Hospital of Sichuan University), Yahong Luo (Liaoning Cancer Hospital & Institute), Guoyue Lv (The First Bethune Hospital of Jilin University), Xin Ni (Beijing Children's Hospital, Capital Medical University), Quchang Ouyang (Hunan Cancer Hospital), Yueyin Pan (The First Affiliated Hospital of University of Science and Technology of China), Songjie Shen (Peking Union Medical College Hospital), Yuqin Song (Beijing Cancer Hospital), Zhangjun Song (Shaanxi Provincial People's Hospital), Zhenchuan Song (The Fourth Hospital of Hebei Medical University and Hebei Tumor Hospital), Tao Sun (Liaoning Cancer Hospital & Institute), Haibo Wang (The Affiliated Hospital of Qingdao University), Hongxia Wang (Fudan University Shanghai Cancer Center), Shusen Wang (Sun Yat-sen University Cancer Center), Yongsheng Wang (Shandong Cancer Hospital), Yu Wang (Shanxi Cancer Hospital), Zhenning Wang (China Medical University), Jiong Wu (Fudan University Shanghai Cancer Center), Puyuan Xing (National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College), Binghe Xu (Cancer Hospital, Chinese Academy of Medical Sciences), Suisheng Yang (Gansu Provincial Cancer Hospital), Feng Yao (Renmin Hospital of Wuhan University Hubei General Hospital), Herui Yao (Sun Yat-sen Memorial Hospital of Sun Yat-sen University), Feng Ye (The First Affiliated Hospital of Xiamen University), Yongmei Yin (Jiangsu Province Hospital), Xiaohua Zeng (Chongqing University Cancer Hospital), Shuqun Zhang (The Second Affiliated Hospital of Xi'an Jiaotong University), Caicun Zhou (Shanghai Pulmonary Hospital), Jian Zhou (Zhongshan Hospital Fudan University), Qing Zhou (Guangdong Provincial People's Hospital Cancer Hospital), and Aihua Zhuang (Sun Yat-sen University Cancer Center).
CONFLICT OF INTEREST STATEMENT
Professor Fei Ma is a member of the Cancer Innovation Editorial Board. To minimize bias, he was excluded from all editorial decision-making related to the acceptance of this article for publication. The remaining authors declare no conflict of interest.
ETHICS STATEMENT
Not applicable.
INFORMED CONSENT
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.