Artificial intelligence and digital health in improving primary health care service delivery in LMICs: A systematic review
Abstract
Aim
Technology including artificial intelligence (AI) may play a key role to strengthen primary health care services in resource-poor settings. This systematic review aims to explore the evidence on the use of AI and digital health in improving primary health care service delivery.
Methods
Three electronic databases were searched using a comprehensive search strategy without providing any restriction in June 2023. Retrieved articles were screened independently using the “Rayyan” software. Data extraction and quality assessment were conducted independently by two review authors. A narrative synthesis of the included interventions was conducted.
Results
A total of 4596 articles were screened, and finally, 48 articles were included from 21 different countries published between 2013 and 2021. The main focus of the included studies was noncommunicable diseases (n = 15), maternal and child health care (n = 11), primary care (n = 8), infectious diseases including tuberculosis, leprosy, and HIV (n = 7), and mental health (n = 6). Included studies considered interventions using AI, and digital health of which mobile-phone-based interventions were prominent. m-health interventions were well adopted and easy to use and improved the record-keeping, service deliver, and patient satisfaction.
Conclusion
AI and the application of digital technologies improve primary health care service delivery in resource-poor settings in various ways. However, in most of the cases, the application of AI and digital health is implemented through m-health. There is a great scope to conduct further research exploring the interventions on a large scale.
1 INTRODUCTION
The Alma Ata declaration articulated the need for intersectoral action in improving the delivery of primary health care (PHC) services. Technology provides a platform to improve health and its determinants. Artificial intelligence (AI) embodies the use of computers with the ability to adapt their actions to prevailing circumstances and aggregate these experiences for improved responses.1 However, AI is not just about computers performing a broad range of intelligent actions, akin to the human mind. While this form of AI is classified as general, the ability of computing systems to perform singular tasks exceptionally is classified as narrow AI.1
AI's potential for health innovations is well recognized to bridge equity gaps,2 improve quality health care delivery, and promote rapid response to outbreaks,1 among other applications. Despite these benefits relevant to rapidly improving health in meeting sustainable development goals (SDGs), there has been a dearth of AI applicability in low and middle-income countries (LMICs).1, 2
In contrast, the wide deployment of m-health characterizes advancements in digital health innovation in LMICs. This is largely fueled by the explosion of mobile technology globally. m-health encompasses technology that leverages mobile telecommunication infrastructure in improving health.1 Its applications transcend mobile phones to smart devices, which by use of telecommunication technology have empowered m-health tools in monitoring and data generation, both in medical and personal settings. Consequently, the scope and potential for the scale of m-health innovation are ever-increasing. Examples range from strengthening demand and supply-side aspects of the health systems to developing extensive datasets in improving health delivery.3, 4
This presents an opportunity for LMICs as PHC delivery is seen as a vehicle for achieving universal health coverage (UHC) and SDGs. Improving the PHC service delivery leads to positive health outcomes, particularly among the most vulnerable. Since PHC focuses not only on holistic individual care throughout the life course but also on improving relevant social determinants of health, this approach is relevant now more than ever.5, 6 Delivering the SDGs and that within the context of disruptions resulting from the COVID-19 pandemic will be challenging. There is mounting evidence that shows the vulnerability of PHC crises.6-9
In their review, Dodd et al. found that service delivery focused on improved contact for users or their experience impacted PHC positively, but operationalization evidence is lacking.5 In LMICs, this evidence expanding on service delivery from both user and provider perspectives is needed.7 This would serve to consolidate PHC's core pillars of the provision of essential health, strengthened policy, and empowered populace as defined by the Astana declaration.6 At the country level, taking into consideration the diverse socioeconomic country contexts and health system development, certainly a customized approach is indicated.
Both m-health and AI have been deployed to address a wide range of health-focused areas in LMICs. With the promise of increased cost-effectiveness, AI has consequently been applied in diagnostic support, improved access through virtual health provision in remote areas, and task shifting in bridging knowledge and skill gaps.1, 2 These approaches can cross-integrate by mining data generated through m-health.4 Further in the study by Berrouiguet et al., a multidevice intervention utilized both data generation and interpretation in outcome prevention.10 Alternately, the IMIA Telehealth Working Group highlighting AI's focus on simplifying investigation over simple clinical skills questioned true cost benefits and also the unintended contribution to widened economic disparities.2
Despite growing evidence, no systematic review to our knowledge has established the consistency of the impact of AI in health service delivery and at the PHC level. The benefit of this review is to inform the applicability of AI in healthcare services across countries, particularly in LMICs and from differing settings. Therefore, through this evidence synthesis, we aim to contribute to filling up this knowledge gap by systematically reviewing evidence to determine the role of artificial intelligence in improving health service delivery. This is relevant for policymakers in deciding the true potential of scalability of these applications along with the resulting contextual program design, and for future research where there are gaps in evidence at present.
2 METHODS
2.1 Registration and search strategy
The review authors have followed the standard guideline of systematic reviews. The review is consistent with the preferred reporting items for systematic review and meta-analysis (PRISMA) 2020 statement11 and has been registered at “International Prospective Register of Systematic Reviews—PROSPERO” (CRD42021214270).
A systematic review expert having vast experience in search management developed the comprehensive search strategy through discussion with the content experts and review teams. Keywords and medical subject heading (Mesh) terms were combined using Boolean operators. Wild cards and truncations were used for refining the search where applicable. The comprehensive search strategy developed for the Medline database has been provided in Table S1. We have provided the PRISMA 2020 checklist in Table S2. Four electronic databases (Medline through PubMed, Web of Science (core collection), Embase, and Cochrane Library) were searched on October 16, 2020 and updated on June 29, 2023. The comprehensive search strategy was modified as per the guidelines of different databases.
2.2 Screening the study
Retrieved articles were imported to “Rayyan”—a web-based open-source application for managing search and screening of systematic reviews.12 The two-stage screening was conducted using “Rayyan.” Two members of the review team (SI and OO) independently screened the retrieved articles for the title and abstract. After screening, the members discussed and resolved disputes. In case of any conflicting decision, a third reviewer (KMSUR) intervened and decided. Another two members of the review team (TM and JA) independently went through the full texts of included articles for final inclusion. Discrepancies were resolved through the same process by engaging a third reviewer (KMSUR). During the full-text screening phase, we used the prioritization and sequential exclusion technique while reporting the reasons for exclusion.13
2.3 Inclusion criteria and exclusion criteria
Any article describing AI, m-health, and digital health interventions in service delivery at PHC settings was included. Articles describing studies on LMICs were considered only. We considered the LMICs as per the definition of the World Bank.14 The World bank used the following definition for the LMICs for the fiscal year 2023: “low-income economies are defined as those with a GNI (Gross national income) per capita of $1,085 or less in 2021; lower middle-income economies are those with a GNI per capita between $1,086 and $4,255; upper middle-income economies are those with a GNI per capita between $4,256 and $13,205.” There was no time limit for the study period. Articles published in English were considered only.
We excluded articles for the following exclusion criteria:
Studies from high-income countries
Articles not describing AI, m-health, or digital health
Studies not in PHC settings
Articles published in languages other than English
Letters, correspondence, editorials, reviews, conference abstracts
2.4 Data extraction
After the final inclusion, two different teams (ES and MM) independently extracted the data using a prespecified data extraction form. Team members finalized the data extraction through discussion. Specific data were extracted focusing study on authors, year of publication, study design, the setting of the study, study population, interventions, and outcome of the study. The outcomes that we considered are the improvement in health service delivery in terms of decision-making in diagnosis and treatment, referral system, follow-up treatment. We also considered utilization of artificial intelligence in health services and the types of health services that incorporated artificial intelligence.
2.5 Risk of bias assessment
Another two members (IH and NI) independently assessed the quality of the included articles. Conflicting decisions were resolved through discussion with the third reviewer. The cross-sectional studies, analytical studies, quasi-experimental studies, and experimental studies were assessed using the set of quality assessment tools provided by the Joanna Briggs Institution.15 Mixed-methods studies were appraised using the mixed-methods appraisal tool (MMAT).16
2.6 Data synthesis
A narrative synthesis of the studies was conducted demonstrating the characteristics of the studies, interventions, or approaches mentioned in the study, and the study outcome. Studies with similar interventions were grouped and synthesized narratively. A meta-analysis was not feasible due to the heterogeneity of the included studies and interventions. As the meta-analysis was not conducted, assessment of publication bias and certainty of the evidence was not applicable. We did not conduct a subgroup analysis and a sensitivity analysis as meta-analysis was not done. The synthesis was done by lead review author (KMSUR) in discussion with all coauthors.
3 RESULTS
3.1 Search outcome
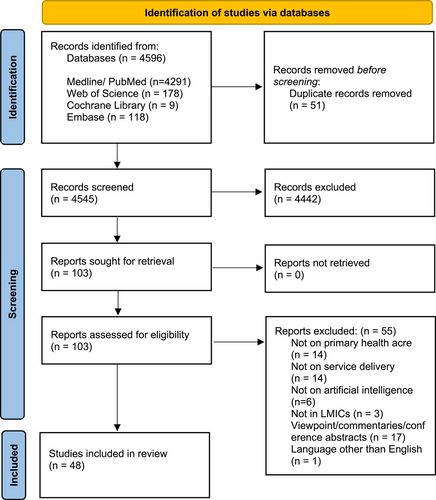
Initial search retrieved 4596 articles from which 4545 articles were screened for title and abstract after deduplication. A total of 103 articles met the inclusion criteria after the title and abstract screening and were reviewed for full text. Finally, forty-eight17-64 articles were included in the systematic review. The search outcome and screening have been demonstrated in the PRISMA flow diagram (Figure 1).
3.2 Characteristics of the included articles
All 48 articles were published between 2013 and 2021 whereas the majority of articles (n = 25) were published since 2018. Among the studies, randomized controlled trials (RCTs) were highest in number (n = 14),17-30 followed by mixed-methods designs (n = 11),31-41 cross-sectional (n = 7),42-48 qualitative study (n = 6),49-54 quasi-experimental (n = 5),55-59 cohort study (n = 2),60, 61 diagnostic accuracy design (n = 2),62, 63 and evaluation time-motion study (n = 1).64 According to the geographic region, one-third of the studies were conducted in Sub-Saharan African countries (n = 16), followed by Latin America (n = 11), South Asia (n = 9), Middle East and North Africa (n = 6), and East Asia (n = 6). The majority of the studies (n = 27) were conducted in rural areas and resource-poor settings, and almost all the studies covered both genders. The main health focus of the included studies was noncommunicable diseases (NCDs) (n = 15); maternal and child health care (n = 11); primary care (n = 8); infectious diseases including tuberculosis, leprosy, and HIV (n = 7); and mental health (n = 6). Characteristics of the included studies have been demonstrated in Table 1.
| Study | Country | Study design | Sample size | Urban/rural | Sex | Age |
|---|---|---|---|---|---|---|
| Alhaidari et al., 201817 | Iraq | RCT | Intervention group 100, control group 150 | Urban setting | Female | Mean age 26.5 years, SD 6.1 |
| Amoakoh et al., 201918 | Ghana | RCT | 176 Health facilities | Remote and nonremote facilities | Female | Mean age 27.1 years, SD 6.4 in intervention arm & 27.3 years, SD 6.3 in control arm |
| Amoakoh et al., 201919 | Ghana | RCT | 307 Phones; of which 74 were shared the rest individual phones | Remote and nonremote health facilities | ||
| Beratarrechea et al., 201920 | Argentina | RCT | 755 (376 Intervention, 379 control) | Poor urban area | 518 Females, 237 males | 40–79 years |
| Gautham et al., 201521 | India | RCT | 144 (16 Health providers, 128 patients) | Rural | Health providers: 8 males and 8 females. 126 patients: 45 males and 81 females | Patients: 69 were adults and 57 pediatrics (age 10 years and below) |
| Harder et al., 201922 | Kenya | RCT | 300 | Rural |
78% Male 22% Female |
38 years old on average |
| Lund et al., 201423 | Tanzania | RCT | 2550 Women, 24 health facilities | 58% Rural | Female | Reproductive age group |
| Modi et al., 201924 | India | RCT | 6493 women | |||
| 22 PHCs | Rural | Female | Mean 24.4 years | |||
| Oliveira-Ciaabati et al., 201725 | Brazil | RCT | 1210 | Urban | Female | 18 and above |
| Peiris et al., 201926 | India | RCT | 62254 | Rural | Both | 40 and above |
| Prabhakaran et al., 201927 | India | RCT | 4270 | Rural | Both | 30 or above |
| Saleh et al., 201828 | Lebanon | RCT | 2359 | Rural and refugee | Both | 40 and above |
| Schuttner et al., 201429 | Zambia | RCT | 33304 | Rural | Both | All ages |
| Souza et al., 202030 | Brazil | RCT | 971 | Urban | Both | 18 and above |
| Diez-Canseco et al., 201831 | Peru | Mixed methods | 755 (733 Patients 22 public health care providers) | Low-income communities | PHCP: all were females. Patients both male and female | Mean age 42.8 years, SD 20.3 |
| Maraba et al., 201832 | South Africa | Mixed methods | 457 | Urban | 42.7% Male | Median age 34 years |
| Nachega et al., 201633 | South Africa | Mixed methods | 109 | Female | 18 to 30 years old | |
| Neupane al., 201434 | South Africa | Mixed methods | 10 Community health workers | Rural | Both/Unspecified | Unstated |
| Odendaal et al., 202035 | South Africa | Mixed methods | 2204 quantitative; 15 qualitative | Rural and semirural | Both | All ages |
| Praveen et al., 201436 | India | Mixed methods | 293 (227 By ASHAs and 69 by physicians) | Rural | Both | Above 35 years |
| Rachmani et al., 202037 | Indonesia | Mixed methods | 123 (22 Leprosy Surveillance Officers and 101 patients) | Rural | Both | All ages |
| Saleh et al., 201838 | Lebanon | Mixed methods | 1390 | Rural & refugee | Both | 40 years and above |
| Tewari et al., 201739 | India | Mixed methods | 1243 Calls to clients (community) and and to staff | Rural | Both | 18 years and above; 28–65 years |
| Yousuf et al., 201540 | South Africa | Mixed methods | 820 | Under served community | Both | 2–15 years; 16–85 years |
| Gong et al., 202141 | China | Mixed methods | Involved in the trial (n = 50); participated in in-depth interviews (n = 27) | Rural | Both | Mean age 46 years |
| Birukila al., 201642 | Nigeria | Cross-sectional | 21,242 | Both urban and rural areas | Both male and female | 66 years and above |
| Lim et al., 202043 | Malaysia | Cross-sectional | 217 | Both Rural and Urban |
71.4% Female 28.6% Male |
Mean age 34.5 years |
|
Maleka et al., 201644 |
South Africa | Cross-sectional | 207 | Urban |
69% 6–8 months 31% 19–36 months |
|
| Ni Z et al., 202045 | Nepal | Cross-sectional | 1130 (17 Community health volunteers; 1113 participants) | Rural | CHW (female); participants (both) | 40–104 years |
| Noureldin et al., 201446 | Egypt | Cross-sectional | 350 | Not stated | Not applicable | Not applicable |
| Sa et al., 201647 | Brazil | Cross-sectional | 96061 | Urban | Both | All ages |
| Wu et al., 201948 | China | Cross-sectional | 25 | Rural | Both | 30–69 |
| Thivant et al., 202049 | Argentina | Qualitative | 29 | Urban area | Both | 18 and above |
| Brandt et al., 2019(50) | Peru | Qualitative | 35 (29 Patients and 6 nurses) | Urban | Patients: females 69% (N = 29). All nurses were female. |
Patients: mean age 60 (SD 9.6, range 47–85) Nurses: mean ages 38 years (SD 6.2, range 31–46 years) |
| Eze et al., 201651 | Nigeria | Qualitative | 3 | Not stated | ||
| Moyano et al., 201952 | Argentina | Qualitative | 24 | 54% Female | 39–66 years old | |
| Schoen et al., 201753 | Brazil | Qualitative | 15 | Not stated | 91% Female | Not stated |
| Zaidi et al., 202054 | Afghanistan & Pakistan | Qualitative | 96 (42 Afghanistan; 54 in Pakistan) | Rural & remote | Not stated | 39 (SD 5.7 Pakistan; 13.3 Afghanistan) |
| Janevic et al., 201655 | Bolivia | Quasi-experimental | 32 | Urban | 78% Female | |
| 22% Male | 58 years (SD 13) | |||||
| Maulik et al., 202056 | India | Quasi-experimental | 22046 | Rural | 85% Male | Mean age 49 years |
| Pichayapinyo et al., 201957 | Thailand | Quasi-experimental | 42 (36 Patients and 6 nurses) | Not stated | Both (mainly female) | 20 years and above |
| Titilayo et al., 201458 | Nigeria | Quasi-experimental | 47 Nurses | Rural | Not stated | Not stated |
| Ugarte-Gil et al., 202059 | Peru | Quasi-experimental | 12 (5 Physicians, 7 nurses) | Urban | Both | Not stated |
| Doocy S et al., 201760 | Lebanon | Cohort | 793 | Syrian refugees and Lebanese | ||
| Doocy S et al., 201761 | Lebanon | Cohort | 793 | Syrian refugees and Lebanese | ||
| Lazuardi L et al., 201362 | Indonesia | Diagnostic accuracy | 19 | Urban | ||
| Sandström et al., 202063 | South Africa | Diagnostic accuracy | 63 | Rural | Both | Mean age 52 years |
| Tierney WM et al., 201664 | Kenya | Evaluation time motion | 32193 | Rural | Not stated | Not stated |
3.3 Quality assessment of included articles
Most of the RCTs were methodologically congruent in terms of reducing the risk of selection bias, performance bias, detection bias, and attrition bias. Only a couple of RCTs were vulnerable to a high risk of bias and did not follow standard statistical methods and measurements.28, 29 Studies using mixed-methods design addressed methodological concerns appropriately with one exception. One study could not rationalize the use of a mixed-methods design and did not adhere to the standard methods of each component.33 Also, most of the studies could not rationalize the use of a mixed-methods design.32-34, 36, 38-40 Quasi-experimental studies were also assessed as good quality except for one where the control group, appropriate measurements, and appropriate use of statistical analysis were questionable.59 There was a lack of congruity between the research question, design, data collection, analysis, and interpretation in two of the qualitative studies.49, 52 The rest of the studies using qualitative design demonstrated methodological rigor. The majority of the cross-sectional studies failed to demonstrate valid and reliable measurement of exposure and outcomes.42, 44, 45, 47, 48 Both the included articles using cohort design were part of the same cohort and did not mention the appropriate measurement of exposure and outcome, dealing with confounders, and did not address incomplete follow-up.60, 61 One brief report demonstrated the automated platelets counter for supporting dengue case detection. The review authors decided to assess the study using the tool for assessing diagnostic accuracy studies. However, methodological issues were not well described in that study.62 The other diagnostic test accuracy study was methodologically congruent.63 The quality of one study could not be assessed due to a lack of an appropriate tool for evaluating studies incorporating time-motion evaluation.64 We have provided the details of the quality assessment in Figures S1–S7.
3.4 Characteristic of interventions using artificial intelligence and digital health
We identified several interventions using AI and digital health technologies. However, the mobile phone remained a popular means by which the majority (n = 42) of the interventions were applied. Twenty-three studies had mobile app-based interventions installed on the phones,20, 21, 24, 26, 27, 31, 32, 34, 35, 39-41, 43, 45, 48, 51, 53, 54, 58-61, 63 while only one study had both phone and computer app installation.53 Also, one study39 provided phone calls to clients in addition to the m-health app while the m-health app was server enabled in one study.40 Only two studies18, 19 applied their interventions by phone calls, SMS, and the internet via mobile phone. Nine studies had SMS-only interventions which were either one way17, 20, 28, 29, 33, 38, 52 or two way.25, 37 Despite using a mobile phone, two studies23, 44 did not state how interventions were applied. Three studies used other methods via the mobile phone, which were interactive voice response system,55 video-sharing,42 and motivational interview.22 The internet-based intervention was found in two studies47, 57 utilizing automated voice calls, email, and web-based systems. An electronic device such as “Tablets” also found their use in two studies.36, 56 The electronic health record (EHR) was used solely in two studies35, 49 and two other studies54, 64 used the mobile phone-enabled EHR. Only two studies were different that incorporated automated platelet counter62 and machine learning.30 Interventions and corresponding outcomes of the included studies have been listed in Table 2.
| Study | Health focus | Intervention | Outcome |
|---|---|---|---|
| RCTs | |||
| Alhaidari et al., 201817 | Maternal health | Weekly text messages on three themes sent to intervention group | Mean clinic ANC visits was higher in the intervention group four times compared to two among control (mean 4.19; 95% CI 3.78–4.59). Improved provider-client interactions. Clients were proactive to ask about their health even from the internet. |
| Amoakoh et al., 201918 | Maternal and neonatal care | m-health support consisting of phone calls, SMS, internet data, and USSD delivered via smartphone | m-health to support clinical decisions did not lead to an improvement in neonatal mortality outcome. The adjusted odds ratio of neonatal deaths was 2.09 higher (95% CI 1.0–4.38) in the intervention compared to control. Neonatal mortality rose from 4.5 to 6.4 deaths per 1000 deliveries in intervention and 3.9 to 4.3 deaths per 1000 deliveries in control. The study asserts that ICT alone is inadequate to determine health outcomes. |
| Amoakoh et al., 201919 | Maternal and neonatal care | m-health clinical decision support system consisted of 4 components: phone calls, SMS, USSD and internet data delivered for 18 months through nonsmartphone to health providers | Request for decision-making information by use of ICT underscores the need to support health facilities to embrace them. Among the most requested were maternal protocols (69.81%, n = 1089) particularly from rural areas, and PPH protocols accounted for 27.22% (n = 450/1653). Regarding neonatal care; prematurity protocols were most requested accounting for 22.6% (n = 168/743). Technology helped to bridge the knowledge gap among providers. |
| Beratarrechea et al., 201920 | NCDs (cardiovascular diseases) | CHW using mobile app to screen CVD risk, SMS reminders to clients regarding clinic appointments, and educational messages in intervention group. Control group CHW screened CVD risk paper-based WHO charts, verbally encouraged to schedule appointment using paper-based system. | 49.4% of participants came for medical consultation within 6 weeks from screening among the intervention group compared to 13.5% among control. Clinical attendance was higher in intervention 59.8% to 22.4% among controls. Mean number of the visit was 1.1 (95% CI 0.9–1.5) compared with 0.4 (95% CI 0.2–0.8) in the control group, and clients lost to follow-up were only recorded in the control group. |
| Gautham et al., 201521 | Infectious diseases | All HP were given smartphones; the app was installed in only HP in control group. | Over 75% of HP appreciated the app and stated that it helped them adhere to treatment protocols. Providers experienced challenges navigating the system as the system was in English. As the study progressed, the control group become aware of the observers hence began to act as expected. |
| Harder et al., 201922 | Alcohol use disorders | Mobile Phone Motivational Interviewing (MI) |
Participants not receiving the mobile phone MI had average Alcohol Use Disorders Identification Test (AUDIT) C score in a month which was 3 points more than the participants receiving the Mobile MI (p < 0005). There was no difference in treatment scores of in-person and mobile use for alcohol users (p > 0.0.5). The alcohol score was found to be decreased in both in-person and mobile MI groups after 6 months |
| Lund et al., 201423 | Maternal and newborn health | Use of mobile phone to prevent perinatal mortality |
The use of mobile phone reduced perinatal mortality with an OR 0.50 (95% CI 0.27–0.93). There was a statistically insignificant reduction in stillbirth (OR 0.65, 95% CI 0.34–1.24). There was a statistically insignificant reduction in child death within 42 days (OR 0.79, 95% CI 0.36–1.74). More women in the intervention group attended recommended four or more antenatal visits 43.8% versus 31.1% among control. |
| Modi et al., 201924 | Maternal and child health |
Use of m-health intervention to improve maternal and child health Use of medical council research framework of Sweden to develop the mobile health intervention application |
The use of ImTeCHO was satisfactory during the study. The visits of neonates were twice in the first week of the intervention. The coverage of home visits in the first week of the childbirth was significantly higher after the intervention (32.4% in the intervention cluster and 22.9% in the control cluster) (95% CI 6.4–14.0, p < 0.001). Care seeking for antenatal and neonatal complications was higher in the intervention group than the control group. There was no difference in the use of ANC provisions by ANM. The intervention group had 90 stillbirths and 104 neonatal deaths and the control group had 107 stillbirths and 102 neonatal deaths. |
| Oliveira-Ciaabati et al., 201725 | Maternal health | Phone SMS system that enabled two-way communication between health providers and pregnant women, that is, in sending health education and health enquiries, respectively | Pregnant women in the intervention group and receiving the intervention (PRENACEL) had a higher relative risk of ANC attendance. RR = 1.12 (95% CI 1.05 to −1.21) |
| Peiris et al., 201926 | NCDs (cardiovascular disease) | m-health app enabling medical decisions in assessing cardiovascular risk | Asides from a slight increase in odds in minimal physical activity, there were no observable differences between intervention and control periods in primary and secondary outcomes. Primary outcome: No differences between intervention and control periods, in the proportion of persons with high CVD risk with a systolic blood pressure of 140 mmHg or less having 41.2% and 39.2%, respectively. OR 1.01 (95% CI 0.76–1.35, ICC 0.004). Secondary outcomes: (1) between intervention and control periods, systolic blood pressure change was −9.3 mmHg and −9.2 mmHg respectively (mean difference 0.28; 95% CI −3.58 to 4.13, ICC 0.014). (2) A slight increase in the odds of minimal physical activity in the intervention compared to control period. OR 1.41 (95% CI 1.16–1.71) 3). Compared to the control period, people consuming a minimum of one BP medication in the intervention period was 53.3% as opposed to 47.9% (OR 1.1; 95% CI 0.90–1.35). |
| Prabhakaran et al., 201927 |
NCDs (diabetes & hypertension) |
Android phone-based application (app) guiding the management of noncommunicable diseases and providing accessible electronic medical records | Primary: By year 1 compared to the baselines and between intervention and control groups, there was no change in mean systolic blood pressure in hypertensive (−1.0 (95% CI −4.6 to 2.7)) (adjusted: −0.3 (95% CI −3.9 to 3.3)). Equally among diabetics, by year 1 compared to the baselines and between intervention and control groups there was no change in mean HbA1C (0.11 (95% CI −0.24 to 0.45)) (adjusted: 0.08 (95% CI −0.27 to 0.44)). Secondary: By year 1 compared to baseline, there were no differences in the mean between control and intervention group in tobacco and alcohol use, fasting plasma glucose, total cholesterol, Framingham score, and body mass index. |
| Saleh et al., 201828 | NCDs (diabetes & hypertension) | SMS-based health education and information system for clients (or their preferred caregiver) and health workers, respectively. | In the posttest compared to the pretest period, the intervention group had odds of controlled blood pressure increase by 28% (OR 1.28; 95% CI 1.00–1.64), but there was no significance statistically in the control groups. In both groups, blood pressure control had lower odds in rural as opposed to refugee areas (Intervention; OR 0.31 (95% CI 0.24–0.40) and Control: OR 0.22 (95% CI 0.15–0.30)). For poorly controlled HBA1C, the odds decreased by 38% in the intervention group comparing the pretest and posttest periods. (OR 0.62 (95% CI 0.15–0.30)). No statistically significant change was observed within the period in the control group. |
| Schuttner et al., 201429 | Primary care | A SMS system utilized to improve client data management, disease diagnosis, and health seeking behavior | 60% outcome by CHWs and 74% increase on follow-up within 4–6 weeks. At follow-up, relief following intervention at the clinic visit occurred more in pediatric and male clients with OR 1.50 (95% CI 1.26–1.79) and OR 1.34 (95% CI 1.13–1.60) compared to other groups |
| Souza et al., 202030 | Mental health (depression) | Machine learning algorithms used to enhance diagnosis of depression | Four of eight algorithms had an average area under the receiver operator characteristic curve (AUROC) at or greater than 0.7. Adaboost performed the worst with an AUROC of 0.58 and had the lowest sensitivity below 0.8, unlike the other seven having sensitivities above 0.8. Rrf demonstrated a good performance in diagnosing mental disorders. |
| Mixed-methods studies | |||
| Diez-Canseco et al., 201831 | NCDs, infectious disease and maternal and child health. | Training of health providers, task shifting, technology-based screening app, web-based collection platform, and remainder SMS. | Of the participants screened, 21.7% (159/733) were positive, and the majority 72.4% (92/127) sought specialist care after screening. The screening tool quickened the diagnosis process; however, there were difficulties to understand some conditions, that is, delusion. The unique skill of the health staff is their ability to detect what ICT fails to diagnose- based on clinical parameters. |
| Maraba et al., 201832 | Infectious diseases (tuberculosis) | Training clinic staffs on use of standard m-health application for tuberculosis case identification and treatment | 89.6% wanted to get the result of TB through text message among whom 20.6% failed to receive the result due to user failure (83.1%), data interact failure (8.4%), and application failure (8.4%). There was no statistical difference in m-health and paper-based indicators. A majority of the patients were satisfied with the intervention and were happy for not having to visit the clinic for results. Patients appreciated the maintenance of confidentiality of the report by use of pin-code in accessing the result through text. 68.6% of results were documented at the clinic within 48 h before the implementation on m-health whereas it was found 96.8% after the m-health implementation and time for treatment decreased from 4 days to 3 days (not statistically significant p = 0.5) |
| Nachega et al., 201633 | Infectious diseases (HIV) | Use of short messages on mobile phone as intervention to prevent mother-to-child transmission of HIV |
90% of women used mobile phones and accessed messages. 88.1% were interested in receiving the text messages for this intervention. 95% had shared their HIV status with at least one person they know and nominate as a cDOT supporter. Some doubted whether all cDOT supporters will be available for them all the time when needed. |
| Neupane al., 201434 | Maternal and child health | A mobile phone software (m-health) that generates reports and enables referrals and supervision, as well as evaluation by team leaders |
40% had a high accuracy in transferring data from weekly to monthly data capture forms. But this improved over time. Improvement of referrals on m-health compared with paper and a reported 100% of referrals using the m-health intervention resulting in linkage to facilities. Intervention did not improve supervision, as both paper and m-health did not increase supervision frequency. |
| Odendaal et al., 202035 | Primary care | m-health system enabling health assessments records and bidirectional communication | Health workers using the m-health system had 485 out of 1085, equivalent to 45% successful referrals across the study sites. However, successful recalls were 628 out of 2204 equivalent to 28% within the study sites. Qualitative reports found the system to have potentials as it offers accountability features and is feasible. |
| Praveen et al., 201436 | NCDs (Cardiovascular disease; blood pressure measurement) | Server stored algorithms providing cardiovascular disease risk evaluation guidelines to support nonphysician and physician clinical decisions, accessed by mobile tablets | 35% of screened clients with elevated blood pressure requiring medication according to the guidelines had a follow-up visit within a month. All (100%) commenced or had their medication reviewed at this follow-up visit. |
| Rachmani et al., 202037 | Infectious diseases (leprosy) | An SMS system with two-way communication for Leprosy Surveillance Office (LSOs) to improve leprosy services and one way to clients and their care givers to provide daily reminders to take their multidrug therapy | Fewer leprosy clients were late at leprosy clinic attendances approximately 21.5%, representing a 13.9% decrease from baseline values (OR 2.41 (95% CI 1.93–3.02)). The LSO's managing client data was challenging |
| Saleh et al., 201838 | NCDs (diabetes & hypertension) | SMS-based health education and information system for clients (or their preferred caregiver) and health workers, respectively. | Receiving and reading the SMS sent compared to not receiving and not reading the SMS was more probable in the young between 40 and 50 at 30.3% compared to 14.8%. Particularly among men. Also more probable among highly educated people. Quality of life of improved and compliance increased to 23% |
| Tewari et al., 201739 | Mental health | Mobile phone (m-health) powered clinical decision-making for health staff, also providing phone calls to clients | 78.6% success rate of two-way communication between the community and health staff. Of these, 71.3% of calls to the community were successful compared to 43% of calls to health staff. The tool enabled all patients to be managed by doctors, with the referral of patients with moderate depression. Overall there was increased health service delivery and knowledge in mental health. The electronic decision support systems was found to be feasible |
| Yousuf et al., 201540 | Ear health/ hearing loss | Mobile phone-based (m-health) app (linked to server), used for screening hearing capacity | Children had a 12% screen referral rate while for adults it was 6.5%. In children, the average screening duration was 47.4 seconds. There was no significant difference between the initial referral rates in adults and children. |
| Gong et al., 202141 | NCDs (stroke management) | Primary-care-based integrated mobile health intervention | The intervention was successfully implemented. The village doctors adopted the intervention components. The technology-enabled components were useful in enhancing the implementation of the program and made it successful. |
| Cross-sectional studies | |||
| Birukila al., 201642 | Infectious diseases | Sharing a 4-min video clip by transferring it through mobile Bluetooth | 83.3% of households owned mobile phones, of which over half had multimedia functions. The use of the phoned showed that SMS was least used (2.1%), videos and music use was at 19.4%. There was high acceptability of the 4-min health information videos 85.4% (n = 12,418) among those with multimedia phones. It was unclear to assert that the Bluetooth video increased polio vaccine acceptance; however, videos were shared more than 100 times per day. |
| Lim et al., 202043 | Primary care | Use of m-health among primary care physicians |
77% frequently used m-health apps and 78.3% used it for medical calculation. 30.9% used it to interact with the EHR system; 42.4% never used m-health for interacting with the EHR system. Only 14.3%−22.1% of PCPs recommended m-health apps to patients 45.1% agreed on m-health apps to be accurate and 53.9% agreed the information be updated. 63.6% agreed that their peers used the m-health app but did not receive support from the organization and patients (18%−32%). 76.9% of primary care physicians thought m-health app to improve the health knowledge of patients but only 56.2% believed it would improve the health of the patients or management of chronic disease (67.3%). 38.2% believed it to be easy to recommend it to patients and 39.1% thought it would be easy for the patients to use. 21.2%, 27.6%, 22.5%, and 30.9% accepted that they had enough time, m-health apps to be affordable, had enough data privacy and valid information respectively. over 70% of participants strongly agreed that m-health improves performance |
| Maleka et al., 201644 | Child health | Use of mobile phone for Parents Evaluation Development Status | Similar referral rates were found between mobile data and paper-based testing (51% vs. 51% among 6–18 age children's' group). |
| Ni Z et al., 202045 | NCDs (hypertension: training, blood pressure measurement) | m-health integrated hypertension with basic health training and use of phone to collect data on hypertensive risk factors in clients and send them related information | Total completion of training resulting in measurements of blood pressure and identification of hypertensive. Increased acceptability by CHWs to use the app and increase in the community follow-up. |
| Noureldin et al., 201446 | Primary care | Use of electronic medical records | Compared to paper records, EMRs had a lower completion in history, that is 87.1% compared to 42.1%. EMRs had an average of 65.7% recorded diagnostic accuracy. |
| Sa et al., 201647 | Primary care | A server and web-based system linked to smartphones at primary health care service delivery units to enhance data collection, recall and analysis | Data transmission improved being six times faster from 8.4 to 1.4 days. |
| Wu et al., 201948 | NCDs (cardiovascular disease—stroke) | Android phone-based app, with both an app and database-based server providing guides for secondary stroke prevention | 100% found the app uses easy, with 92% agreeing (some strongly) to continue its use. Consequently, it was acceptable by the village doctors. 92% had no technical problems during the period of the trial. 71% found the app useful in standardizing their activities with 67% in aiding clinical decisions. |
| Qualitative studies | |||
| Thivant et al., 202049 | Health systems | Electronic health record (EHR) allows medical practitioners to focus on reasons why clients sought medical consultation. It proved to be faster and minimizes duplication of records. It however stressed the need to have a paper backup when running EHR system. | |
| Brandt et al., 201950 | Mental health | Patients received phone pop-ups encouraging them to complete behavioral activities (18 sessions delivered 3 times per week for 6 weeks). SMS were equally sent to reminding appointments. Nurses monitored patients using web and by calling periodically. | 93% attributed that the intervention (CONEMO app) helped them emotionally, and 34% assert that it lessened feelings of abandonment. However, clients had challenges reading SMS, responding to phone pop-ups at intervention inception were reported. 33% (n = 27) said that it brought a feeling of being cared for when they received a monitoring phone call from the nurses. 95% appreciated phone-based appointments that reduced time on health consultation and minimizes crowding at facilities. Despite the benefits outlined, 11% of patients (n = 28) still preferred face-to-face monitoring instead of phone calls. Nurses raised concern that CONEMO activities interfered with their routine work and also were concerned about the smartphone being stolen. |
| Eze et al., 201651 | Maternal and child health | Experts believed that integrating m-health in routine immunization will improve immunization coverage, reduce drop-out, and improvement in data quality. They however bemoaned the lack of policies to support use. | |
| Moyano et al., 201952 | NCDs (cardiovascular diseases) | CHW using mobile app to screen CVD risk, SMS reminders to clients regarding clinic appointments, and educational messages in intervention group. Control group CHW screened CVD risk paper-based WHO charts and verbally encouraged to schedule appointment using paper-based system. | 49.4% of participants came for medical consultation within 6 weeks from screening among the intervention group compared to 13.5% among control. Clinical attendance was higher in intervention 59.8% to 22.4% among controls. Mean number of the visit was 1.1 (95% CI 0.9–1.5) compared with 0.4 (95% CI 0.2–0.8) in the control group, and clients lost to follow-up were only recorded in the control group. |
| Schoen et al., 201753 | Primary care | A dual mobile and computer application that enables easy data management and link of data to the central disease databases | The application improved efficiency by enabling health workers time savings spent on paper documentation and in retrieving client information. The hardware and software reportedly had poor quality. The community members had negative attitudes about their utilization. |
| Zaidi et al., 202054 | Maternal and child health | Mobile-based (m-health) application enabling electronic medical record entry and retrieval and also having video communication features for education and awareness | In Pakistan, most of the health workers noted the app was easy to use, as well as in Afghanistan. This ease was attributed to the apps registration and not documentation use in Afghanistan. In both countries, the video component was well received by clients. Also, the follow-ups improved. |
| Quasi-experimental studies | |||
| Janevic et al., 201655 | Mental health (depression) | Interactive voice response (IVR) calls for 14 weeks to the patients of depression. |
IVR completion rate was higher among women (56% women vs. 44% men) and among participants who graduated from secondary school (60% vs. 40% who did not graduate from secondary level). Self-reported health status and depressive symptoms on the first IVR call were nonsignificant (p = 0.66 and 0.60, respectively, for self-reported health status and depressive symptoms). Self-reported health was better among patients receiving first IVR call who had good or better health at baseline (means 2.4 vs. 3.1). 97% of participants were very satisfied with the IVR call. 67% indicated IVR call helped them to manage their depression to great extent. 83% would want to repeat the IVR call system for their depression management. IVR was beneficial to participants- reminders to medication adherence, self-care. Participants preferred human interaction, and they highlighted technology challenges. |
| Maulik et al., 202056 | Mental health | Antistigma campaign, training health providers to use tablet to refer at risk individuals, training of doctors to make decision support using tablets | Self-reported prior use of mental health services increases from 3.3% to 81.2% (OR 133.3, 95% CI 89.0–199.7, p < 0.5). Out of the total population who sought care for mental health, 70% were female. 50% were having emotional stress, depression, and anxiety with suicide risk, who had the clinical condition, out of them, 38.8% visited the clinic for a second time and 4.1% visited the doctor with 3 requiring further treatment. Mean depression and anxiety score reduces significantly after the intervention from 13.4 at baseline to 3.1 after 12 months (95% CI −10.7 to −9.8, p < 0.001) |
| Pichayapinyo et al., 201957 | NCDs (diabetes) | An automated voice call and email system sending interactive messages to clients and staff, respectively. | Mean reduction in HbA1C of 0.9% (p < 0.001) while fasting blood glucose had a mean reduction of 14.9 mg/dL (p < 0.001) |
| Titilayo et al., 201458 | Maternal health | Mobile phone (m-health)-based training platform for nurses | Between the control and experimental groups, the difference in means was significant on m-health knowledge at F = 2.469 df (2.0–90.0) and on its use F = 2.409 df (2.0–90.0) |
| Ugarte-Gil et al., 202059 | Tuberculosis | Accelerated diagnosis of tuberculosis using a mobile phone (m-health) app | Uploading the image occurred in a median of 58% of the time because health workers were too busy to. In general, the main challenge to uploading was a long time, noted in 46.9% of health workers. The workload of health workers had a negative impact on the effective use of the app. |
| Cohort Studies | |||
| Doocy et al., 201760 | NCDs | Training of providers on use of m-health, patient-controlled health record (data storage app), and decision-making support for providers. | Medical records reporting remained was greater compared to clinic medical records (BMI 47.4% to 15.8%, BP 74.5% to 40.7%). However, no change was noted in other indices. Blood sugar test results 39.9% to 34.0%. Patients reported that providers sparingly used the screening application 21.7% (CI: 15.9–28.4). The satisfaction of the health workers’ competencies by the client rose from 11.0% to 89.0%, while the client said providers used time prudently. Provider attitude toward use m-health was mixed; some believed time and wireless challenges. Need for programming and technical repairs on the system to be determined before roll-out |
| Doocy et al., 201761 | NCDs | Training health workers on use of guidelines to support clinical decision-making and m-health app that served as electronic health record. | There was low utilization of the m-health app by providers with only, 154/761 completing interviews using the m-health app. There was a notable increase in BMI reporting from 7.7% (95% CI 6.0–9.7) at baseline compared to end line 15.8% (95% CI 13.5–18.4). Comparison between paper-based records and electronic records showed a higher proportion of recording seen in the m-health app; that is, BP measurement was 74% to 38.6% paper-based and BMI recording in the app was 47% to 15.8% paper-based. By using the app, providers help to schedule appointments and follow-up for the clients, which then increased from 58% (95% CI 47.7–67.8) baseline to 97.8% (95% CI 94.4–99.4) during the m-health phase. Providers offered counseling using the app, that is, for smoking cessation 16.9% compared to 11.4% paper records. Medication compliance improved during m-health phase- antihypertensive medication interruption was high at baseline 9.3% (95% CI 7.3–11.6) to 8.6% (95% CI 6.0–11.7), similarly for type 2 diabetes 7.5% (95% CI 5.4–10.2) to 5.5% (95% CI 3.0–9.0) in m-health. Patient-provider interaction improved signifying the quality of care provided. |
| Diagnostic accuracy study | |||
| Lazuardi et al., 201362 | Dengue platelets count | Use of automatic platelets counter for supporting dengue case detection | Compared to a manual count, the automatic system overestimated the platelets count in 5 cases and underestimated in 3 cases. |
| In 59% of the samples, i.e. 11 samples, the result was similar both in the automatic and manual count. | |||
| Sandström et al., 202063 | Hearing health care | Smartphone self-test audiometry | Smartphone self-test audiometry provided reliable and accurate air conduction hearing thresholds for adults. |
| Evaluation time-motion study | |||
| Tierney et al., 201664 | Primary care & HIV | Android phone powered electronic health records system integrated to meet all clinic attendances including HIV | The electronic health records were used for all patients all the time. Of those with HIV, 85% received care. But in two clinics (Burnt Frost and Turbo), the overall time spent within the clinics increased from 37 to 87 min and 56 to 106 min at each clinic visit. |
- ANC, antenatal care; CHW, community health worker; HP, health providers; CVD, cardiovascular diseases; LSO, leprosy surveillance officer; EHR, electronic health record; IVR, interactive voice response; NCDs, noncommunicable diseases; HIV, human immunodeficiency virus.
3.5 Types of outcomes
Outcome measures were grouped on the type of intervention applied. The major outcomes measured across most of the interventions that used m-health, and recommendation of m-health, record-keeping, and documentation, waiting time, efficiency of services, client satisfaction, and quality of service.
3.5.1 Use and recommendation of m-health
Six studies demonstrated the use and recommendations regarding m-health where the participants were health providers, clinical staff, primary care physicians, village doctors, and physicians. A study43 found that 77% of respondents frequently used m-health apps (78.3% for medical calculation, 30.9% for interaction with an EHR system, and 42.4% never used m-health for interacting with an EHR system) but only 14.3%−22.1% of primary care physicians recommended m-health app to patients.43 Another study demonstrated that 71% found the app useful in standardizing their activities with 67% in aiding clinical decisions regarding the care of stroke.48 Another study described that the mobile application facilitates adherence to the treatment protocol.21 A primary-care-based integrated mobile health intervention for the management of stroke was found effective and well adopted by the village doctors.41
It was easy to use and acceptable, where 100% found the app user-friendly, with 92% agreeing (some strongly) to continue its use. Consequently, it was acceptable to the village doctors. Ninety-two percent had no technical problems during the period of trial.48 There were proper confidentiality and privacy,32, 43 for example, the use of pin-code in accessing results.32 A study found that it aided physicians diagnosing the risk factors of stroke,48 whereas another study60 found difficulties in diagnosing some specific conditions such as delusions. Also, a smartphone-based self-test Audiometry was found accurate and reliable.63
3.5.2 Record-keeping and documentation
The m-health was found to have improved medical records reporting and documentation compared to clinical paper-based records in five studies.34, 43, 46, 60, 61 On average, 65.7% of EHR recorded diagnostic accuracy.46 Easy scheduling of appointments was increased from 58% (95% CI 47.7–67.8) baseline to 97.8% (95% CI 94.4–99.4) during m-health phase.61 EHR allowed providers to focus on reasons why clients sought medical consultation and minimized duplication of records. It was, however, stressed the need to have a paper backup when running EHR system.49 Experts also believed m-health integration would improve coverage and data quality and reduce drop-out.51 Faster documentation and retrieval of client information were reported49, 53 while one study64 found increased overall time spent within the clinics from 37 to 87 min and 56 to 106 min at each clinic visit. Also three studies32, 40, 44 found no statistically significant difference in the documentation time with the use of the apps; for example, similar referral rates were found between mobile data- and paper-based testing (51% vs. 51% among 6–18 years age children group).44
3.5.3 The waiting time, satisfaction, efficiency, and quality of services
The m-health shortened the waiting time for clients and service providers31, 32, 43, 50, 60 For instance, 95% appreciated phone-based appointments that reduced time on health consultation and minimized crowding at facilities.50 The majority of the patients were satisfied with the intervention and were happy not to visit the clinic for results. Also, the time for treatment decreased from 4 days to 3 days (statistically insignificant p = 0.5).32 However, 11% of patients (n = 28) still preferred face-to-face monitoring instead of phone calls. Nurses raised concerns that these activities interfered with their routine work and they were also concerned about the smartphone being stolen.50
The competency of the health workers was improved through m-health interventions.31, 60, 61 For example, the satisfaction of the health workers’ competencies by clients rose from 11.0% to 89.0%.60 Also, 93% attributed the m-health app helped them emotionally, and 34% assert that it lessened feelings of abandonment. Another 33% (n = 27) said that it brought a feeling of being cared for when they received a monitoring phone call from the nurses.50 Over 70% of participants in one study43 strongly agreed that m-health improves performance (n = 217). Another study56 found that self-reported prior use of mental health services increased from 3.3% to 81.2%. Around 50% had emotional stress, depression, and anxiety with suicide risk, and the mean depression and anxiety score reduces significantly after the intervention from 13.4 at baseline to 3.1 after 12 months (95% CI −10.7 to −9.8, p < 0.001).
In addition, there were improved clinic attendance, follow-up, and medication adherence.20, 21, 23, 24, 31, 36, 39, 45, 54, 61 For example, pregnant women in the intervention group attended four or more antenatal visits more frequently (43.8%) than the control group (31.1%).23 One study showed that 100% (n = 292) of participants commenced or had their medication reviewed at a follow-up visit.36 There was also improved knowledge of users39, 43, 58 and overall client satisfaction.32, 39, 43, 58
Although the use of m-health helped to improve knowledge among providers,19 it did not minimize the risk of the disease (hypertension and diabetes) or reduce mortality (maternal and neonatal) as reported in some of the studies.18, 19, 26, 27 For instance, compared to the baselines and between intervention and control groups, there was no change in the mean systolic blood pressure in hypertensive people,27 and neonatal mortality rose from 4.5 to 6.4 deaths per 1000 deliveries in intervention and 3.9 to 4.3 deaths per 1000 deliveries in control.18 There was no significant reduction in stillbirth (OR 0.65, 95% CI 0.34–1.24), and child death within 42 days (OR 0.79, 95% CI 0.36–1.74).23 It showed technology alone is inadequate to determine health outcomes.18
The use of text messages improved interaction, information sharing, and clinic attendance,17, 20, 25, 29, 37 and disclosure.33 For example, mean clinic ANC visits were higher in the intervention group up to four times compared to two among the control (mean 4.19; 95% CI 3.78–4.59).17 Also, 49.4% of participants came for medical consultation within 6 weeks from screening among the intervention group compared to 13.5% among the control clinical attendance was higher in intervention 59.8% to 22.4% among controls.20 Text messages were likely to be received and read by men, highly educated and younger people, and increased compliance to 23%.38 Overall relief and satisfaction also have been seen post SMS intervention among children and men with OR 1.50 (95% CI 1.26–1.79) and OR 1.34 (95% CI 1.13–1.60) compared to other groups.29 However, clients were likely to forget information sent.52 One study50 reported clients having the challenge of reading SMS and responding to phone pop-ups at intervention inception.
The use of video-sharing (19.4%) was higher than SMS (2.1%), and highly acceptable (85.4%, n = 12,418) as reported in one study.42 As for mobile phone motivational interviews, participants not receiving the intervention had an average Alcohol Use Disorders Identification Test (AUDIT) C score in a month, which was 3 points more than the participants receiving the intervention (p < 0005). Although there was no difference in treatment scores of in-person and mobile use for alcohol users (p = 0.63). The alcohol score was found to be decreased in both in-person and mobile intervention groups after 6 months.22
One study62 found estimation errors; for instance, compared to a manual count, the automatic system overestimated the platelets count in five cases and underestimated it in three cases but in 59% of the samples, the result was similar both in the automatic and manual count. Using machine learning algorithm techniques, one study demonstrated improved performance in diagnosing mental disorders.30
4 DISCUSSIONS
4.1 Summary of the findings
Artificial intelligence and the application of digital technologies improved primary healthcare service delivery in resource-poor settings in various ways. However, in most cases, the application of AI was limited to m-health. We found EHR assisted to find the causes of medical consultation at the primary care level in LMICs. m-health improved medical reporting and record-keeping compared to the traditional paper-based system. It made appointment scheduling easier for patients at primary care facilities. However, the association between using m-health and the length of documentation time was not clear. Client satisfaction rose steeply for health providers using m-health, even in mental health services through increasing knowledge of users and providers, emotional support, clinic attendance, information sharing, and medication adherence. m-health was also useful to standardize service activities at the primary care level. Shortening waiting time is another important implication of using m-health in the health system. It also reduced crowding at facilities. We also found that the applications used at the primary care level were user-friendly, and health providers were motivated to continue using the application. However, m-health did not help to curb the risk of hypertension and diabetes and the burden of maternal and neonatal mortality. On the other hand, the machine learning algorithm improved the diagnosis of depression.
4.2 Agreement and disagreement with available studies
The use of AI in primary care settings is mostly confined to m-health interventions in LMICs. However, several studies conducted in high-income countries demonstrated the successful implementation of artificial intelligence and digital health interventions in primary care.65-67 Our study reported artificial intelligence and m-health rose clients’ satisfaction with the services. Another systematic review aiming to assess patient experiences with technology-enabled care documented most respondents were satisfied with the technology-based services.68 We found that m-health improved service activities by shorting waiting time, reducing crowding, and improving diagnosis. Similarly, a systematic review reported EHR improved access to medical consultation to specialty care, avoiding unnecessary visits and shorting waiting time.69 A recent scoping review mentioned that AI can be used to address health inequalities in primary care.70 Other literature reviews in high-income settings have found that m-health reduced hospital admission, increased doctor-patient relationships, and improved risk assessment.71-73 We found mobile applications and texting increase clinic attendance. A similar systematic review documented a consistent improvement of clinic attendance at healthcare appointments by text message reminders irrespective of types of healthcare level.74 Deloitte Center for Health Solutions found using the mobile application in health systems made scheduling easier. We also found that m-health made scheduling appointments easier for the patient at the primary care level. Deloitte Center for Health Solutions also found that m-health systems increased efficiencies of documentation and supply chain management.75 Our study documented that reporting quality improved significantly using EHR or m-health. Our finding suggests that m-health did not reduce the prevalence of hypertension. We did not get any similar studies. However, a literature review found that m-health increased the doctor-patient relationship, assisted in transferring data, and participated in medical decision-making.72
4.3 Research implication
Our analysis suggested that the m-health introduction assisted to improve health service deliveries. Most of the articles on m-health we analyzed were conducted at an individual level on a small scale in the LMICs. Large-scale and multisetting study designs are crucial to better understanding the implication of m-health at the primary care level. Research studies on the application of AI at the PHC level are scarce in LMICs. However, all studies we included showed significant implications in improving health service delivery. Different systematic reviews found that in developed countries, the internet of medical things, smart wears,76 and machine learning were keeping a huge impact on clinical decisions, managing databases, early diagnosis, and monitoring.77, 78 AI doctors can come up with health advice on common health problems.79 Digital health coaching and fully AI-based automated text coaching for patients with chronic diseases reduced hospital visits. An automatic speech recognition system can document patient information on EHR during the conversation between patient and physician. However, we found limited studies apply these in LMICs. Future research is required to examine the effectiveness of the intervention in LMICs.
4.4 Policy implication
Technology has become a crucial part of our health systems. Before implementing any artificial intelligence in health systems, the government should ensure a smooth interface between new technology-based systems and existing systems. First, the government needs to engage the user to build their trust and awareness about the benefit of this new tool. It was one reason for the limited response to Google Health.80 Sensitization to technology for both healthcare providers and patients is important. Commitment from both central and local governments is essential to implement artificial intelligence successfully. Our finding suggests most of the implementation of artificial intelligence was at the individual level. The government should intervene in those at a wide scale and nationally. Policy adaptation to secure data privacy and security is needed. Regular monitoring of the quality of infrastructure is also important.
4.5 Strength and limitations
The main strength of our study was following the method of systematic review in every step rigorously. Screening, data extraction, and quality assessment of included studies were conducted in duplicate. We included both quantitative and qualitative studies and assessed the quality of the included articles.
However, our study has some limitations. We only used literature from the English language. Other language studies might have important implementations of AI. However, a study reported that language restriction in systematic reviews did not produce significant bias.81 Some studies were with a small population size. Furthermore, the overall quality of many included studies was not convincing. Precaution is needed to interpret the findings. Another limitation was we searched only Medline through PubMed, the Web of Science, and Cochrane Library databases. Searching more databases including gray literature might retrieve more articles.
5 CONCLUSIONS
The use of AI and digital health has got a promising response to improve PHC service delivery. Further explorations to identify the best practice in different contexts will strengthen these interventions. The commitment of the government and the donor agencies is required to test these interventions on large scale.
ACKNOWLEDGMENTS
Open access funding provided by IReL.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
FUNDING INFORMATION
There is no funding for this study. None of the authors are linked or affiliated with any industry.
ROLE OF THE FUNDING SOURCE
There was no funding for this systematic review. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.




