Enigma portal: Peritoneal effusion in a patient with a myeloproliferative neoplasm
Abstract
Quiz regarding the cytological analysis of peritoneal effusion in a patient with a history of myeloproliferative neoplasm.
1 CASE HISTORY
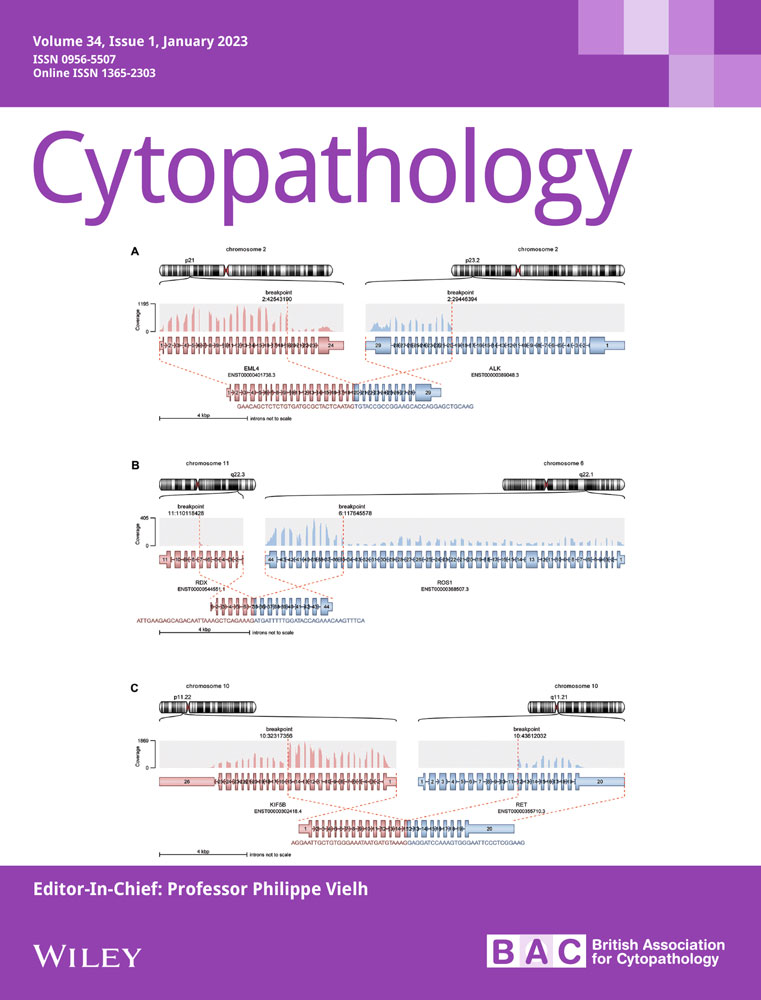
An 81-year-old male patient presented with an essential thrombocythemia with JAK2 p.V617F mutation in 2016. He was treated with hydroxyurea until February 2022, when a tricytopenia was observed. The histological findings of a bone marrow biopsy revealed primary myelofibrosis with diffuse fibrosis and without blasts. In May 2022, he was admitted to the emergency department and an echography detected a splenomegaly (his spleen measured 16 cm) associated with pleural and peritoneal effusions. The peritoneal effusion was aspirated (see Figures 1-4 note that each question below may have more than one correct answer).
2 MORPHOLOGY QUIZ
- Based on Figure 1, the peritoneal effusion contains:
- Macrophages.
- Numerous mesothelial cells.
- Basophils.
- Myeloid precursors including blasts.
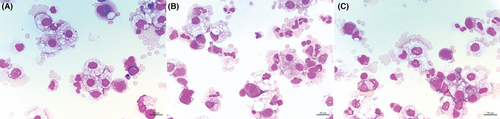
- In Figure 2, the cell indicated by the black arrow is …:
- … a reactive mesothelial cell.
- … a malignant cell corresponding to metastatic non-small cell carcinoma.
- … a megakaryocyte.
- … a giant macrophage.
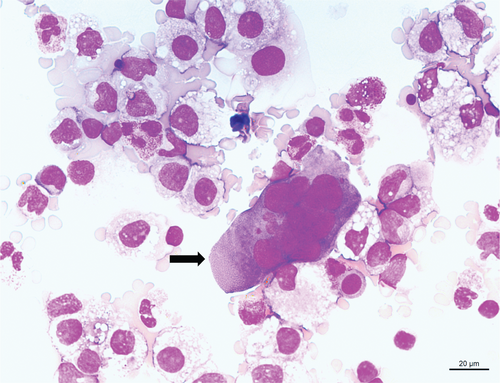
- Based on all of the images, what is the most likely diagnosis?
- Peritoneal extramedullary haematopoiesis.
- Acute leukaemia.
- Peritoneal malignant mesothelioma.
- A rare evolution of primary myelofibrosis.
3 DISCUSSION
For this patient, cytological examination of the ascites revealed that 16% of the cells were myeloid precursors including blasts. basophils represented 8% of the cells. Rare megakaryocytes and erythroblasts at different stages of maturation were also observed. Figure 4 is an annotated copy of Figure 1.

Extramedullary haematopoiesis is a consequence of the sequestration and proliferation of circulating clonal myeloid precursors to atypical sites. It can occur in any organ, but the most frequent ectopic sites are the spleen and liver.1
Ascites caused by peritoneal extramedullary haematopoiesis is a rare evolution of primary myelofibrosis.2 The presence of megakaryocytes in pleural or peritoneal effusion is rare, and it is most commonly associated with myelofibrosis.3 Among 4844 pleural or peritoneal effusions, Kumar et al reported that megakaryocytes were present in five samples. In the case presented in this article, the clinical context helps to establish the diagnosis. without any clinical context and based only on cytological examination, the presence of haematopoietic precursors from three different lineages (myeloid precursors with blasts, megakaryocytes and erythroblasts) is indicative of a haematopoietic pathology. An increased percentage of blasts may indicate leukaemic transformation, and a bone marrow biopsy or aspiration should be performed to confirm the diagnosis.4 In this case, the low percentage of blasts (3%) was more suggestive of myelofibrosis than a leukaemic transformation.
The present report, in addition to documenting a rare case, highlights the pivotal role of peritoneal cytological examination in the diagnosis of such a case. A specialist haematopathology review is recommended to confirm the diagnosis in such cases.
AUTHOR CONTRIBUTIONS
DF, EK, CG and MA: data collection. DF: writing the manuscript. EK, CG, MA, RC and PR: reviewing the manuscript.
ACKNOWLEDGEMENTS
We thank Nathalie Boitano, Corinne Derrien, Christian Brundu and Laetitia Bus for their technical help.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analysed in this study.