Soluble CD206 levels correlate with disease deterioration and predict prognosis of anti-MDA5 antibody-positive dermatomyositis related interstitial lung disease
Yan Li and Xiaoqin Liu contributed equally.
Abstract
Introduction
The prognosis of anti-MDA5 antibody-positive dermatomyositis/clinically amyopathic dermatomyositis-associated interstitial lung disease (MDA5-DM/CADM-ILD) is poor. This study was to evaluate the effect of serum soluble CD206 (sCD206), a biomarker of macrophage activation, on predicting the interstitial lung disease (ILD) deterioration and prognosis for MDA5-DM/CADM-ILD.
Methods
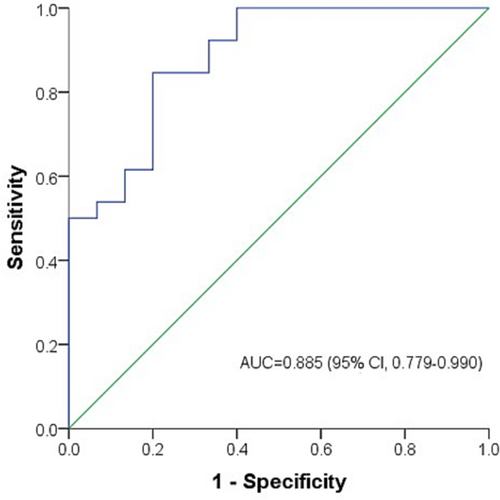
Forty-one patients diagnosed with MDA5-DM/CADM-ILD were retrospectively included. The clinical data were analyzed. Serum sCD206 levels were measured in 41 patients and 30 healthy controls. The relation between sCD206 levels and ILD deterioration was assessed. Receiver operating characteristic (ROC) curve was generated to determine the optimal cut-off value of sCD206 for predicting outcome. The association between sCD206 and survival was examined.
Results
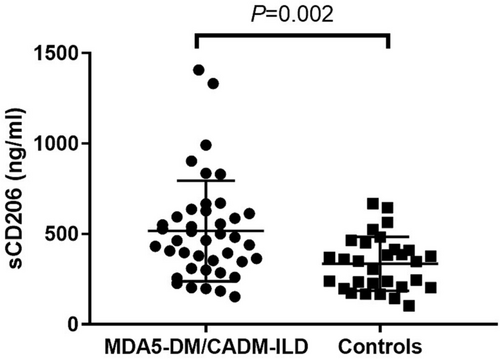
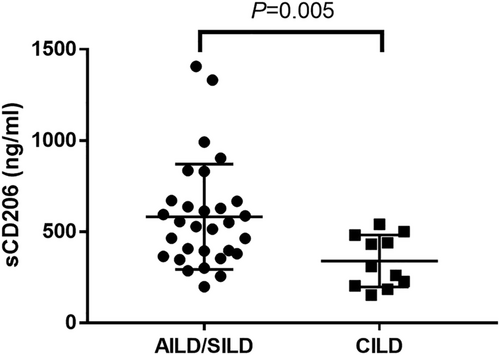
The median serum sCD206 level in patients was significantly higher than healthy controls (464.1 ng/mL vs. 349.1 ng/mL, P = 0.002). In DM/CADM patients, the sCD206 level was significantly higher in patients with acute/subacute interstitial lung disease (AILD/SILD) than those with chronic interstitial lung disease (CILD) (539.2 ng/mL vs. 309.4 ng/mL, P = 0.005). The AUC of sCD206 was 0.885 for predicting mortality (95% CI 0.779–0.990). Patients were divided into two groups: sCD206 high level group (≥400 ng/mL) and sCD206 low level group (<400 ng/mL). Patients with sCD206 high level had significantly decreased survival rate than those with low level (25% vs. 88%, P < 0.001). The adjusted hazard ratio of sCD206 for mortality was 1.003 (adjusted for age and gender, P < 0.001), with sCD206 high level associated with higher death risk (HR 4.857, P = 0.006).
Conclusion
Serum sCD206 might be a potential predictor of ILD deterioration and prognosis for Chinese patients with MDA5-DM/CADM-ILD.
1 INTRODUCTION
Dermatomyositis (DM) is an idiopathic inflammatory myopathies (IIM) affecting multiple organs including skin, muscles, and lungs.1 Clinically amyopathic dermatomyositis (CADM) is a unique subtype of DM presenting with typical rash but without muscular manifestations. DM often affects the lungs and presents with interstitial lung disease (ILD), especially in patients with CADM.2 ILD is the leading cause of death from DM/CADM.3, 4 Notably DM/CADM patients with antimelanoma differentiation-associated gene 5 (anti-MDA5) antibody positive frequently develop a rapidly progressive form of ILD with fatal outcome.5 Especially those patients presenting with active disease pattern may die of respiratory failure in very short term and need to be identified timely in order to take better clinical management. Serological markers can be measured noninvasively, even in patients severely ill. Useful serum biomarkers would be helpful to evaluate the ILD deterioration and predict prognosis for patients with anti-MDA5 positive DM/CADM-related ILD (MDA5-DM/CADM-ILD).
Macrophages involving in the pathogenesis of DM/CADM-related ILD (DM/CADM-ILD) has received increasing interest during recent years. There are two types of macrophages: M1 type (classically activated) and M2 type (alternatively activated).6 M1 macrophages have proinflammatory functions, whereas M2 macrophages show anti-inflammatory characteristics.7 The macrophage mannose receptor (CD206) is a 180-kDa transmembrane glycoprotein and mainly expressed by M2 macrophages. CD206 has been considered a biomarker of activated M2 macrophages. CD206 can be cleaved from macrophage membrane and released into periphery circulation, called soluble CD206 (sCD206). Similar to membrane form, sCD206 has the function of altering the innate and adaptive immune responses.8 Serum sCD206 has been highlighted as a noninvasive biomarker in infectious diseases.9, 10 However, the value of sCD206 in MDA5-DM/CADM-ILD has not been fully examined.
This retrospective study was conducted to evaluate the effect of sCD206 on predicting ILD deterioration and prognosis for MDA5-DM/CADM-ILD patients. Meanwhile, the clinical features were assessed to better understand this unique disease.
2 MATERIALS AND METHODS
2.1 Subjects
Patients with newly diagnosed DM/CADM-ILD at the Department of Respiratory Medicine of Nanjing Drum Tower Hospital between 2016 and 2018 were retrospectively reviewed. Bohan and Peter criteria were used to make the diagnosis of DM.1 Patients who met the definite or probable DM criteria were included. The diagnosis of CADM referred to the Euwer and Sontheimer criteria.11, 12 The diagnosis of ILD was based on the presence of symptoms such as cough and exertional dyspnea, and requisite high-resolution computed tomography (HRCT) abnormalities. Only DM/CADM-ILD patients with anti-MDA5 antibody positive were recruited. Healthy controls were chosen from health screening conducted at Nanjing Drum Tower Hospital within the same time period between 2016 and 2018. A total of 41 MDA5-DM/CADM-ILD cases and 30 healthy controls were identified in the current study. The study adheres to the amended Declaration of Helsinki criteria. The research protocol was approved by the Ethics Committee of Nanjing Drum Tower Hospital. Regarding serum conservation, written informed consent was obtained from each subject. Regarding the data analyses, informed consent was waived because this study was analyzed retrospectively using anonymized clinical data.
2.2 Data collection
Full medical record abstraction for each patient was conducted and the following baseline clinical variables were collected: Age, gender, smoking status, DM/CADM diagnosis, clinical symptoms, chest HRCT manifestations, treatment modalities, available pulmonary function test results, laboratory results, and other medical conditions.
2.3 Evaluation of ILD deterioration
Regarding ILD deterioration, patients were divided into two groups: Acute/subacute interstitial lung disease (AILD/SILD) and chronic interstitial lung disease (CILD). Patients presented with rapidly progressive ILD and dyspnea within 3 months from onset of respiratory symptoms were grouped as AILD/SILD. Patients presented with stable or slowly progressive ILD and dyspnea more than 3 months from the onset of respiratory symptoms were grouped as CILD.13, 14 The evaluation of ILD deterioration was made blindly without knowledge of the sCD206 levels.
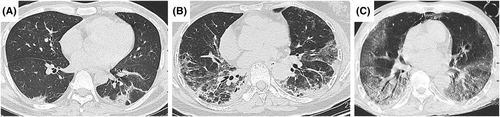
2.4 Classification of HRCT manifestations
Chest HRCT images at the time of diagnosis from all included patients were reviewed. HRCT manifestations were categorized through direct interpretation and analysis by an experienced ILD specialist (HR Cai) and a thoracic radiologist (KF Zhou). According to the guidelines for interstitial pneumonias,15 patients' HRCT manifestations were classified as following four types: Organizing pneumonia (OP), nonspecific interstitial pneumonia (NSIP), OP combined with NSIP, and diffuse alveolar damage (DAD). The disagreements were resolved by consensus agreement.
2.5 Detection of serum anti-MDA5 antibody and sCD206
Anti-MDA5 antibody and sCD206 were detected using the stored serum samples collected at the diagnosis. Anti-MDA5 antibody was tested by anti-myositis antibody profile IgG detection kit (EUROMIMMUN Medizinische Labordiagnostika AG, Germany).16 Serum sCD206 levels were measured by ELISA (Raybiotech Human CD206 ELISA Kit). Experimental procedures were performed according to the manufacturer's instructions.
2.6 Statistical analyses
Data are presented as medians (observed ranges) or numbers (percentages). For continuous variables, Mann–Whitney U test was used. For categorical variables, either chi-square test or Fisher's exact test was used according to the sample size. Spearman's rank correlation was used to evaluate the correlations between sCD206 and other continuous variables. Receiver-operating characteristic (ROC) curve was generated to determine the optimal cut-off value of serum sCD206 for predicting patients' outcome. The point that had the highest value of Youden index (sensitivity + specificity − 1) was selected as the optimal cut-off value.
Survival status was identified by reviewing the medical records or telephone follow-ups. Overall survival (OS) time was calculated as the period (months) from DM/CADM-ILD diagnosis (the date of blood draw) to death. Survival was assessed up to December 30, 2018. Patients still alive on December 30, 2018, were censored. Univariate and multivariate Cox hazards models were used to evaluate the prognostic impact on survival for clinical variables. The Kaplan–Meier method with the log-rank test was used to compare the survival difference between patient groups.
Analyses in this study were performed with SPSS (version 22.0, SPSS Inc., Chicago, IL, USA) and GraphPad Prism (Version 7, GraphPad Software, San Diego, CA, USA). The P values were two sided and at a significance level of 0.05.
3 RESULTS
3.1 Baseline characteristics
Serum sCD206 level was significantly elevated in MDA5-DM/CADM-ILD patients compared with controls (median level: 464.1 ng/mL vs. 349.1 ng/mL, P = 0.002; Figure 1). Out of 41 patients, 26 died of respiratory failure. The patients' baseline characteristics are presented in Table 1. There was a higher ratio of CADM (58.5%). Thirty patients (73.2%) presented with AILD/SILD. Regarding chest HRCT manifestations, 34.1% (14/41) showed DAD, 29.3% (12/41) showed NSIP, 26.8% (11/41) showed OP combined with NSIP, and 9.8% (4/41) showed OP. The representative chest HRCT images were shown in Figure 2.
| Variables | Patients (n = 41) | r | P value |
|---|---|---|---|
| Age, years | 53.0 (32.0–77.0) | 0.251 | 0.113 |
| Female | 24 (58.5) | - | |
| Never/former/current smokers | 28 (68.3)/6 (14.6)/7 (17.1) | - | |
| DM/CADM | 17 (41.5)/24 (58.5) | - | |
| AILD/SILD/CILD | 12(29.3)/18 (43.9)/11(26.8) | - | |
| Fever | 21 (51.2) | - | |
| HRCT findings | - | ||
| OP/NSIP/OP + NSIP/DAD | 4(9.8)/12(29.3)/11(26.8)/14(34.1) | - | |
| Treatment prior to admission | - | ||
| CS alone/CS + IM/None | 18(43.9)/4(9.8)/19(46.3) | ||
| Treatment after admission | - | ||
| CS alone/CS + IM | 5(12.2)/36(87.8) | ||
| FVC, % predicted (n = 17) | 66.09 (36.1–86.2) | 0.230 | 0.374 |
| FEV1, % predicted (n = 17) | 69.6 (41.9–95.2) | 0.252 | 0.328 |
| TLC, % predicted (n = 11) | 71.4 (39.2–84.8) | −0.155 | 0.650 |
| DLCO, % predicted (n = 14) | 58.45 (8.2–81.7) | −0.156 | 0.594 |
| PaO2, torr (n = 37) | 60.0 (44.0–97.9) | −0.399 | 0.014 |
| OI (n = 37) | 258 (56–710) | −0.490 | 0.002 |
| WBC, 109/L (n = 41) | 6.9 (1.9–18.0) | 0.015 | 0.924 |
| PLT, 109/L (n = 41) | 198 (97–347) | −0.210 | 0.189 |
| Lymphocyte count, /mm3 (n = 41) | 700 (200–2500) | −0.484 | 0.001 |
| CD4+ lymphocyte count, /mm3 (n = 36) | 255.5 (37–1169) | −0.392 | 0.018 |
| NK count, /mm3 (n = 36) | 67.5 (13–1060) | −0.277 | 0.103 |
| CRP, mg/L (n = 38) | 11.15 (2.2–79.1) | 0.233 | 0.158 |
| ESR, mm/h(n = 33) | 40 (7–97) | −0.009 | 0.961 |
| CK, U/L (n = 37) | 41.0 (11–377) | 0.264 | 0.115 |
| LDH, U/L (n = 38) | 402 (227–15 743) | 0.602 | <0.001 |
| Ferritin, ng/mL (n = 41) | 1143.9 (38.8–27130.0) | 0.428 | 0.005 |
| sCD206, ng/mL (n = 41) | 464.1 (152.5–1407.2) | - |
- Note: Data are presented as median (observed range) or number (%). All P values are derived from Spearman's rank correlation coefficient. Bold values: P<0.05.
- Abbreviations: AILD/SILD, acute/subacute interstitial lung disease; CADM, clinically amyopathic dermatomyositis; CILD, chronic interstitial lung disease; CK, creatine kinase; CRP, C-reactive protein; CS, corticosteroids; DAD, diffuse alveolar damage; DLCO, diffusing capacity of the lung carbon monoxide; DM, dermatomyositis; ESR, erythrocyte sedimentation rate; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; HRCT, high-resolution computed tomography; IM, immunosuppressants; LDH, lactate dehydrogenase; NK, natural killer; NSIP, nonspecific interstitial pneumonia; OI, oxygen index; OP, organizing pneumonia; PLT, platelet; TLC, total lung capacity; WBC, white blood count.
3.2 Correlations between serum sCD206 levels and clinical characteristics
Correlation analyses showed that serum sCD206 levels were positively correlated with conventional serum markers for disease activity, such as LDH and ferritin (Ps < 0.05), while negatively correlated with PaO2, oxygen index (OI), peripheral lymphocyte count, and CD4+ lymphocyte count (Ps < 0.05). The correlation coefficients and P values are listed in Table 1.
3.3 Serum sCD206 level was elevated in MDA5-DM/CADM patients with AILD/SILD
As presented in Figure 3, the serum concentration of sCD206 was significantly higher in patients with AILD/SILD compared with CILD (539.2 ng/mL vs. 309.4 ng/mL, P = 0.005).
3.4 ROC curve analysis
ROC curve was generated for serum sCD206. The area under curve (AUC) of sCD206 was 0.885 for predicting mortality (95% CI, 0.779–0.990). The optimal cut-off value was determined as 400 ng/mL. The sensitivity was 84.6% and specificity was 80% (Figure 4).
3.5 Prognostic values of serum sCD206
Using the optimal cut-off value of sCD206, 41 patients were divided into two groups: sCD206 high level (≥400 ng/mL, n = 25) and low level (<400 ng/mL, n = 16). Kaplan–Meier curve showed the patients with sCD206 high level had significantly lower survival rate than those with sCD206 low level (25% vs. 88%, P < 0.001; Figure 5).
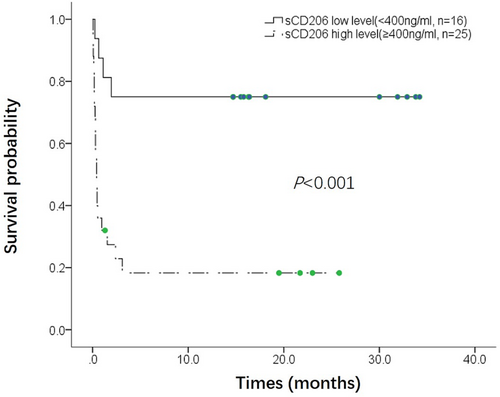
Univariate Cox hazards regression analyses were performed (Table 2). Among the baseline clinical characteristics, older age, patients with AILD/SILD, presence of fever, HRCT manifestation of DAD, elevated CRP, elevated LDH, higher serum ferritin level, and higher serum sCD206 level were all significantly associated with worse prognosis (Ps < 0.05). While combination therapy of corticosteroids and immunosuppressants, higher PaO2, higher OI, higher lymphocyte count, and higher CD4+ lymphocyte count were all significantly associated with better prognosis (Ps < 0.05). Multivariate Cox hazards regression analyses were further performed adjusting for age and gender. The significance of the following variables associated with prognosis remained: patients with AILD/SILD, presence of fever, HRCT manifestation of DAD, combination therapy of corticosteroids and immunosuppressants, PaO2, OI, lymphocyte count, CD4+ lymphocyte count, and sCD206. The adjusted hazard ratio of sCD206 was 1.003 (95%CI: 1.001, 1.004, P < 0.001). The adjusted hazard ratio for patients with sCD206 high level (≥400 ng/mL) was significantly increased compared with those with sCD206 low level (<400 ng/mL) (HR 4.857, P = 0.006). We further performed multivariate Cox analysis adjusting for AILD/SILD, serum ferritin, and lymphocyte count, since they were known prognostic factors for MDA5-DM/CADM-ILD patients. The significance of sCD206 associated with prognosis remained (HR 1.002, 95%CI: 1.001, 1.003, P = 0.007).
| Unadjusted HR | 95% CI | P value | Age and gender adjusted HR | 95% CI | P value | |
|---|---|---|---|---|---|---|
| Age, years | 1.050 | 1.013, 1.088 | 0.008 | - | ||
| Female | 0.678 | 0.313, 1.468 | 0.324 | - | ||
| Former/current smokers | 1.611 | 0.714, 3.633 | 0.251 | 1.324 | 0.490, 3.581 | 0.580 |
| CADM | 0.940 | 0.431, 2.047 | 0.875 | 0.771 | 0.347, 1.712 | 0.523 |
| ILD deterioration | ||||||
| CILD | Ref | |||||
| AILD/SILD | 6.083 | 1.420, 26.056 | 0.015 | 5.047 | 1.146, 22.229 | 0.032 |
| Fever | 2.848 | 1.251, 6.485 | 0.013 | 2.871 | 1.254, 6.572 | 0.013 |
| HRCT findings | ||||||
| Non-DAD | Ref | Ref | ||||
| DAD | 5.456 | 2.318, 12.843 | <0.001 | 6.356 | 2.393, 16.880 | <0.001 |
| Treatment prior to admission | ||||||
| None | Ref | |||||
| CS alone | 0.977 | 0.445, 2.143 | 0.953 | 0.822 | 0.370, 1.829 | 0.631 |
| CS + IM | 0.271 | 0.035, 2.076 | 0.209 | 0.285 | 0.036, 2.259 | 0.235 |
| Treatment after admission | ||||||
| CS alone | Ref | |||||
| CS + IM | 0.298 | 0.101, 0.882 | 0.029 | 0.239 | 0.076, 0.755 | 0.015 |
| FVC, % predicted, (n = 17) | 1.064 | 0.992, 1.141 | 0.085 | 1.054 | 0.976, 1.139 | 0.177 |
| FEV1, % predicted, (n = 17) | 1.045 | 0.990, 1.102 | 0.110 | 1.021 | 0.968, 1.077 | 0.452 |
| TLC, % predicted, (n = 11) | 1.037 | 0.944, 1.139 | 0.447 | 1.112 | 0.942, 1.313 | 0.210 |
| DLCO, % predicted, (n = 14) | 1.026 | 0.969, 1.086 | 0.374 | 1.135 | 0.945, 1.363 | 0.176 |
| PaO2, torr (n = 37) | 0.957 | 0.925, 0.989 | 0.009 | 0.942 | 0.907, 0.978 | 0.002 |
| OI (n = 37) | 0.991 | 0.986, 0.995 | <0.001 | 0.991 | 0.985, 0.996 | 0.001 |
| WBC, 109/L | 1.078 | 0.940, 1.235 | 0.283 | 1.112 | 0.962, 1.286 | 0.152 |
| PLT, 109/L | 0.994 | 0.987, 1.000 | 0.066 | 0.996 | 0.989, 1.004 | 0.327 |
| Lymphocyte count, per 100/mm3 increase | 0.697 | 0.585, 0.830 | <0.001 | 0.717 | 0.593, 0.868 | 0.001 |
| CD4 count, /mm3 (n = 36) | 0.996 | 0.993, 0.999 | 0.006 | 0.997 | 0.994, 0.9998 | 0.037 |
| NK count, /mm3 (n = 36) | 1.00 | 0.998, 1.003 | 0.873 | 1.001 | 0.998, 1.003 | 0.521 |
| CRP, mg/L (n = 38) | 1.020 | 1.001, 1.039 | 0.042 | 1.018 | 1.000, 1.036 | 0.054 |
| ESR, mm/h (n = 33) | 0.990 | 0.971, 1.009 | 0.310 | 0.993 | 0.973, 1.014 | 0.523 |
| CK, U/L (n = 37) | 1.001 | 0.997, 1.005 | 0.704 | 0.999 | 0.994, 1.004 | 0.757 |
| LDH, U/L (n = 38) | 1.0002 | 1.000047, 1.000353 | 0.010 | 1.000 | 1.000, 1.000 | 0.085 |
| Ferritin, ng/mL | 1.00007 | 1.00002, 1.00012 | 0.005 | 1.000 | 1.000, 1.000 | 0.214 |
| sCD206, ng/mL | 1.003 | 1.002, 1.004 | <0.001 | 1.003 | 1.001, 1.004 | <0.001 |
| <400 | Ref | |||||
| ≥400 | 6.486 | 2.201, 19.115 | 0.001 | 4.857 | 1.557, 15.151 | 0.006 |
- Note: Bold values: P < 0.05.
- Abbreviations: AILD/SILD, acute/subacute interstitial lung disease; CADM, clinically amyopathic dermatomyositis; CILD, chronic interstitial lung disease; CK, creatine kinase; CRP, C-reactive protein; CS, corticosteroids; DAD, diffuse alveolar damage; DLCO, diffusing capacity of the lung carbon monoxide; DM, dermatomyositis; ESR, erythrocyte sedimentation rate; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; HRCT, high-resolution computed tomography; IM, immunosuppressants; LDH, lactate dehydrogenase; NK, natural killer; NSIP, nonspecific interstitial pneumonia; OI, oxygen index; OP, organizing pneumonia; PLT, platelet; TLC, total lung capacity; WBC, white blood count.
4 DISCUSSION
This study assessed the clinical significance of the alternative macrophage marker sCD206 in patients with MDA5-DM/CADM-ILD. The serum sCD206 level was elevated in patients with MDA5-DM/CADM-ILD and higher in patients with acute/subacute interstitial lung disease. Besides, our study suggested that serum sCD206 could predict prognosis of these patients, with elevated sCD206 associated with worse prognosis.
Mechanisms for serum sCD206 elevation in MDA5-DM/CADM-ILD has remained unclear. The pathophysiologic process of MDA5-DM/CADM-ILD included proinflammatory cytokines overproduction and alveolar macrophages activation in the lungs.17 Alveolar macrophages in this condition mainly show the characteristics of M2 type.18 M2 macrophages are characterized as immunosuppressive cells, preventing excessive inflammation and regulating tissue repair.19, 20 Activated M2 alveolar macrophages express substantial CD206 on cell surface. Immunohistochemical staining in autopsy specimens has shown alveolar macrophages positive for CD206.21 This membrane form of CD206 can be cleaved and released into peripheral circulation as sCD206. Elevated serum sCD206 might represent activation of M2 alveolar macrophages in MDA5-DM/CADM-ILD, which was in accordance with the disease pathophysiology.
In this study, serum sCD206 level showed negatively correlated with lymphocyte count and CD4+ lymphocyte count in MDA5-DM/CADM-ILD patients. The negative correlation between sCD206 and CD4+ lymphocyte count was also found during human immunodeficiency virus infection.10 Peripheral lymphopenia is common in autoimmune disease.22 Reduction of lymphocyte-mediated defense function might cause macrophage activation. The mechanism underlining the correlation of lymphopenia and sCD206 elevation needs to be further clarified.
HRCT evaluation has been demonstrated useful in predicting the presence of anti-MDA5 antibody in DM-ILD23; however, the prognostic value of HRCT manifestations for MDA5-DM/CADM-ILD has not been fully evaluated. Our study showed that DAD manifestation in chest HRCT was significantly associated with worse prognosis. Serum sCD206 was significant higher in patients with DAD manifestation than those without DAD presence (data not shown). The severe damage caused by DAD may trigger the activation of anti-inflammatory alveolar macrophages, leading to more CD206 being released into the peripheral circulation. Meanwhile, our study showed combination treatment of corticosteroids and immunosuppressants was significantly associated with lower risk of death. The immunosuppressants in this study included cyclophosphamide, cyclosporin A, and tacrolimus. Combination therapy of corticosteroids and immunosuppressants has been widely used to treat MDA5-DM/CADM-ILD. Our findings provide useful information for clinical practice regarding these patients.
Serum sCD206 levels were also found significantly correlated with serum ferritin in patients with MDA5-DM/CADM-ILD. CD206 and ferritin are all mainly produced by activated alveolar macrophages. However, only sCD206 proved to be an independent prognostic predictor in this study. In addition, the AUC of sCD206 was 0.885. Serum sCD206 might be a better prognostic predictor than ferritin for patients with MDA5-DM/CADM-ILD.
The limitation of this study is that this is a single-center, small-sample retrospective study, which is common in the studies regarding MDA5-DM/CADM-ILD, since the incidence of this unique disease is very low. Horiike et al previously reported increased sCD206 was associated with worse prognosis in MDA5-CADM/DM-ILD, which was consistent with our result.24 Our study had a bigger sample size about Chinese patients and the relationships between sCD206 and various clinical characteristics were also determined.
5 CONCLUSIONS
The prognosis of MDA5-DM/CADM-ILD patients is poor. Our study showed sCD206 was elevated in patients with acute/subacute interstitial lung disease compared with chronic interstitial lung disease, and higher serum sCD206 level was associated with worse prognosis. Serum sCD206 could be a useful noninvasive biomarker to imply ILD deterioration and predict the prognosis for MDA5-DM/CADM-ILD patients.
AUTHOR CONTRIBUTIONS
Yan Li and Xiaoqin Liu contributed to collecting data, analyzing data, and writing the paper. Min Cao and Hourong Cai contributed to designing the study, interpreting data, and revising the paper. Mi Tian, Ruyi Zou, and Yujuan Gao measured serum biomarkers. Mi Tian and Mei Huang contributed to collecting data and interpreting data. Kefeng Zhou and Hourong Cai contributed to HRCT evaluation.
ACKNOWLEDGEMENTS
This work was supported by the grants from the Natural Science Foundation of Jiangsu Province (No. BK20221168) and Nanjing Municipal Health and Family Planning Commission (YKK22084).
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no conflict of interests regarding this paper.
ETHICS STATEMENT
This study adheres to the amended Declaration of Helsinki criteria. The research protocol was approved by the Ethics Committee of Nanjing Drum Tower Hospital. Regarding serum conservation, written informed consent was obtained from each subject. Regarding the data analyses, informed consent was waived since this study was analyzed retrospectively using anonymized clinical data.
Open Research
DATA AVAILABILITY STATEMENT
Data and materials related to this paper are available from the corresponding authors on reasonable requests.