Computerized nailfold video-capillaroscopy in type 2 diabetes: A cross-sectional study on 102 outpatients
计算机化甲襞视频毛细血管镜在2型糖尿病中的运用: 对102例门诊患者的横断面研究
Abstract
enBackground
Type 2 diabetes (T2D) is a chronic disease that negatively affects vascular health. A careful assessment of chronic complications, including microcirculation, is mandatory. The computerized nailfold video-capillaroscopy (CNVC) accurately examines the nailfold microvasculature, but its suitability in T2D is currently under investigation.
Aims
To describe nailfold microvasculature in T2D patients regarding the level of glucose control and chronic microvascular and macrovascular complications.
Methods
This is a cross-sectional study on 102 consecutive and unselected outpatients with T2D who had undergone CNVC examination. The examination was carried out by using an electronic video-capillaroscope with 300x magnification. Capillaroscopic appearance and capillary changes were described according to well-established parameters. Capillaroscopic parameters were compared between patients with poor glucose control (HbA1c ≥7%) and those with better glucose control (HbA1c <7%) and between patients with chronic complications and those without. Chronic complications were deduced from the anamnestic, laboratory, and instrumental data and the five-item International Index of Erectile Function (IIEF-5) questionnaire.
Results
Nailfold capillaries in patients with HbA1c ≥7% were thicker (p = .019) and longer (p = .021) than in those with better glucose control. Ectasias (p = .017) and microaneurysms (p = .045) were more frequently observed in patients with HbA1c ≥7.0% than those with HbA1c <7.0%. Patients with ED, compared to those without, had a lower frequency of bizarre-shaped capillaries (p = .02). Microaneurysms (p = .02) were more frequently described in patients with carotid stenosis (>20%) than those without.
Conclusion
Relevant nailfold microvascular alterations were observed in T2D, most of which were associated with poor glycemic control, ED, and carotid stenosis. Further investigation is needed to recognize the role of CNVC in predicting the onset and evolution of chronic complications and monitoring the effectiveness of antihyperglycemic treatments on microcirculation.
摘要
zh背景: 2型糖尿病(T2D)是一种对血管健康产生负面影响的慢性疾病。对慢性并发症、包括微循环的仔细评估是必须的。计算机化甲襞视频毛细血管镜(CNVC)能够准确检查甲襞微血管,但其是否适合用于T2D尚待研究。本文旨在描述T2D患者的甲襞微血管,探讨血糖控制水平以及慢性微血管和大血管并发症对其的影响。
方法: 这是一项针对102名连续且未经筛选的T2D门诊患者的横断面研究,所有患者均接受CNVC检查。使用电子视频毛细血管镜以300倍的放大率进行检查。根据已确定的参数描述毛细血管镜下外观和毛细血管改变。将毛细血管镜参数在血糖控制不佳(HbA1c≥7%)和血糖控制较好(HbA1c<7%)的患者之间以及有慢性并发症和无慢性并发症的患者之间进行比较。慢性并发症根据病史、实验室和仪器数据以及国际勃起功能指数(IIEF-5)问卷进行推断。
结果: HbA1c≥7%患者的甲襞毛细血管较厚(p=0.019)且更长(p=0.021),与血糖控制较好的患者相比。HbA1c≥7.0%的患者中毛细血管扩张(p=0.017)和微动脉瘤(p=0.045)的发生率高于HbA1c<7.0%。与无ED患者相比,有ED的患者奇异形状毛细血管的发生率较低(p=0.02)。伴有颈动脉狭窄>20%的患者中微动脉瘤的发生率较高(p=0.02)。
结论: 在2型糖尿病患者中观察到相关的甲襞微血管改变,其中大多数与血糖控制不佳、ED和颈动脉狭窄有关。需要进一步调查以认识到CNVC在预测慢性并发症的发生和进展以及监测抗高血糖药物治疗对微循环的有效性中所起的作用。
1 BACKGROUND
People living with type 2 diabetes (T2D) are at risk of developing microvascular and macrovascular complications,1 with atherosclerotic cardiovascular disease (CVD) as the most relevant cause of comorbidity and mortality.2 Microvascular complications, such as diabetic retinopathy (DR), micro- and macroalbuminuria, diabetic neuropathies, and erectile dysfunction, foster the risk of CVD,3, 4 also affecting the quality of life and general health status.5, 6
The computerized nailfold video-capillaroscopy (CNVC) is an imaging technique analyzing the microvasculature at the level of the toes and fingers in feet and hands. The method is used in numerous fields of medicine to assess microvascular injury in several conditions, including non-rheumatologic disorders such as hypertension,6 T2D,7 and endocrine diseases.8 The CNVC is not currently used in diabetology, even if a previous study found that nailfold examination can easily detect specific capillaroscopic changes in prediabetes and T2D compared to healthy controls and in T2D complicated by diabetic neuropathy.9
This study aimed to describe nailfold microvasculature characteristics in patients with T2D, analyzed by the CNVC at the level of nailfold of fingers. In addition, nailfold microvasculature changes were compared according to the level of glucose control and the presence of chronic diabetes-related complications at the time of the examination.
2 MATERIALS AND METHODS
The cross-sectional study was conducted on 102 consecutive and unselected T2D outpatients who attended the Endocrinology Center of the University of Bari from January to September 2018. Each patient was informed about the study's purposes and provided written informed consent to participate before undergoing the examination.
Inclusion criteria were as follows: established diagnosis of type 2 diabetes and age ≥18 years. Exclusion criteria were caffeine consumption and cigarette smoking within 2 hours before the CNVC examination and confirmed diagnosis of connective tissue disorders.
A single operator (G.L.) performed the CNVC examination. The examination was conducted after proper handwashing with water and soap and a complete ceramic oil immersion of fingers to obtain clear images. Fingers with recent signs of trauma were excluded to avoid false positive results. To prevent significant peripheral vasomotion, patients were examined at comfortable room temperatures between 23° and 25°C.
Nailfold microvasculature was described, and relevant morphological changes were classified according to quantitative and qualitative parameters. The former included capillary density, depth, and length. The latter were tortuosity (TOR), bizarre-shaped capillaries (BIZ), ectasias (ECT), avascular areas (AVA), microaneurysm (MIC), bleeding (BLE), and visible subpapillary venous plexus (PLE). The criteria used to describe quantitative and qualitative parameters are explained elsewhere.10
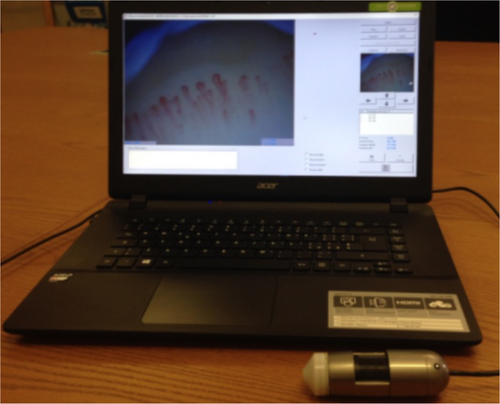
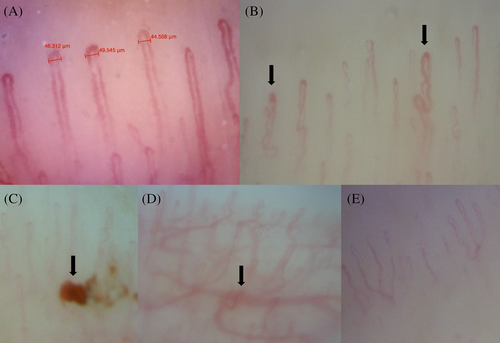
The CNVC examination was performed using the PicocapMicrolab Electronica® (Padua), as shown in Figure 1. Nailfold images were collected from the distal row of the fourth and fifth fingers of the nondominant hand. At least three shots were acquired and registered from the nailfold middle in examined fingers (Figure 2). Nailfold characteristics were described in each image, and all findings were shown as an average.
Medical history and physical examination, recent laboratory tests, and instrumental examinations were available for each patient. Information on chronic complications was obtained after a comprehensive appraisal of medical history, laboratory tests (e.g., serum creatinine and urinary albumin-to-creatinine ratio), electrocardiogram, carotid ultrasound, and fundoscopic examination. Lastly, the five-item International Index of Erectile Function (IIEF-5) questionnaire was administered to men for diagnosing and classifying erectile dysfunction (ED).11
The glucose control was defined based on the glycated hemoglobin (HbA1c) levels. More precisely, HbA1c <7% defined patients with optimal glucose control, whereas those having HbA1c ≥7% had worse glucose control.
3 STATISTICS
Descriptive data are shown as numbers, percentages, mean (or median), and SD (or quartile range). Comparisons between categorical variables were performed by the chi-square test. A two-tailed t test was performed to evaluate mean differences between the two groups in the case of continuous variables with a normal distribution (assessed by the Shapiro–Wilk test). A p value ≤.05 was considered statistically significant. Statistical analyses were carried out with R.
4 RESULTS
4.1 Baseline characteristics
The cross-sectional study included 102 outpatients (68 men and 34 women). Ten patients were excluded due to signs of trauma at the level of the fourth and fifth fingers of both hands (two), evidence of heavy manual works significantly affecting the nailfold microvasculature (two), having consumed caffeine or cigarette smoke before the examination (five), and suspicion of the Raynaud phenomenon (one).
Arterial hypertension (74%) and hypercholesterolemia (72%) were the main comorbidities in the study population. Around 80% of the entire cohort exhibited a weight excess. Thirty-seven patients (36.2%) were overweight (body mass index [BMI]: 25–29.9 kg/m2), and 45 (44.1%) were obese, defended as BMI ≥30 kg/m2. Sixteen individuals (15.6%) were current smokers (12 men; 4 women), and 31 (30.3%) smoked in the past (29 men; 2 women).
Mean age (men: 62.9 [10.8] years vs. women: 64.2 [12] years, p = .2), and the evolution of T2D (men 12.3 [9.2] years vs. women 11.8 [9] years, p = .5), arterial hypertension (men: 10.8 [7.9] years vs. women: 14 [8.7] years, p = .06), and hypercholesterolemia (men: 7.8 [7] years vs. women: 9.8 [9.6] years, p = .08) were not statistically different between the two genders.
4.2 Biochemical and anthropometric parameters
Table 1 shows the leading laboratory and anthropometric parameters of the study population. The mean value of HbA1c was 7.0%. Slightly more than half of patients (51.7%) achieved an adequate glucose control. Glucose control was similar between men and women. Low-density lipoprotein cholesterol levels were lower in men than women (men: 81.4 [31.4] mg/dL vs. women: 99.1 [41.7] mg/dL, p = .02). Non-high-density lipoprotein (HDL) cholesterol levels were lower in men than women (men: 106.5 [34.7] mg/dL vs. women: 124.7 [44.3] mg/dL, p = .03). Conversely, HDL cholesterol levels were higher in women than men (women: 54.3 [12.8] mg/dL vs. men: 46.3 [11.6] mg/dL, p = .002).
| Variable | Mean (SD) | UM | p value |
|---|---|---|---|
| FPG | 126.2 (32.9) | mg/dL |
.08 |
| Women | 117.7 (32.6) | ||
| Men | 129.9 (32.7) | ||
| HbA1c | 7.0 (1) | % |
.06 |
| Women | 6.7 (1.1) | ||
| Men | 7.2 (0.9) | ||
| Non-HDL cholesterol | 109.5 (41.9) | mg/dL |
.03* |
| Women | 124.7 (44.3) | ||
| Men | 106.5 (34.7) | ||
| HDL cholesterol | 49.6 (13.2) | mg/dL |
.002* |
| Women | 54.3 (12.8) | ||
| Men | 46.3 (11.6) | ||
| LDL cholesterol | 87.1 (35.7) | mg/dL |
.02* |
| Women | 99.1 (41.7) | ||
| Men | 81.4 (31.4) | ||
| Triglycerides | 132.2 (85.2) | mg/dL |
.8 |
| Women | 133.7 (95.9) | ||
| Men | 130.1 (80.4) | ||
| eGFR | 84.1 (19.5) | mL/min/1.73 m2 |
.4 |
| Women | 86.4 (17.6) | ||
| Men | 83 (20.4) | ||
| ACR | 56.9 (150) | mg/g |
.97 |
| Women | 56 (175.5) | ||
| Men | 57.3 (139.3) | ||
| BMI | 31.4 (2.4) | kg/m2 |
.4 |
| Women | 31.7 (2.7) | ||
| Men | 29.8 (2.2) | ||
| WC | 123.2 (12.3) | cm |
.6 |
| Women | 121.9 (14.5) | ||
| Men | 124.5 (11.1) |
- Abbreviations: ACR, albumin to creatinine ratio; BMI, body mass index; eGFR, estimated filtration rate; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; HDL, high density lipoproteins; LDL, low density lipoproteins; UM, unit of measurement; WC, waist circumference.
- * Statistically significant (p value <.05).
The BMI and waist circumference were not significantly different between the two genders.
4.3 Diabetes-related complications
Patients with renal impairment were defined as those having a stable estimated glomerular filtration rate <60 mL/min/1.73 m2 or urine albumin to creatinine ratio >30 mg/g. They represented 32% of the study population (33 individuals).
DR has been diagnosed in 31 patients (30.5%), and 24 (23.5%) had established CVD (composite of acute coronary syndromes, coronary or carotid artery revascularization, stroke, and peripheral artery occlusion or revascularization).
Carotid intima-media thickness ranged from 0.6 to 1.4 mm (mean 0.91 [0.18] mm). An atherosclerotic stenosis in the carotid artery (CAS) was seen in 60 patients (58%), 45 men (59.4%), and 15 women (47%).
Clinically relevant erectile dysfunction (IIEF-5 < 17 points) was diagnosed in 20 men (19.6%).
4.4 CNVC findings
Capillary findings were defined as summarized in Table 2. They were split into two main categories, quantitative and qualitative parameters, according to Tavakol et al.12 The capillary density was 7.7 (1.6) per mm2 with no difference in men compared with women. Capillary depths and lengths were 42.2 (9.9) μm and 193.5 (91.3) μm, respectively. Although nailfold capillaries were longer and deeper in men than women, this difference was not statistically significant.
| Nailfold capillaroscopic parameters | |
|---|---|
| Quantitative | Qualitative |
| Capillary density: number of capillary loops observed in the nailfold distal row per mm2. | Tortuosity (TOR): capillary with waved, cross-linked, sinuous or twisted shape in at least 50% of the nailfold distal row per mm2. |
| Capillary diameters (depth and length): number of capillary loops observed per mm2 of the visual field (nailfold distal row). | Ectasias (ECT): capillary with apex diameter >50 μm and/or with one or both loop branches thickness >20 μm. |
| Capillaries with bizarre shape (BIZ): capillary with highly ramified shape, or shape resembling part of a tree or an animal. | |
| Avascular areas (AVA): capillary density <7 capillaries/mm2 or the absence of two or more consecutive distal row capillaries or capillary loss within a space >500 μm. | |
| Microaneurysm (MIC): dilatation of the capillary wall at the level of the capillary loop apex and/or one or both loop branches. | |
| Bleeding (BLE): hemosiderin deposits. | |
| Visible subpapillary venous plexus (PLE). | |
- Abbreviation: CNVC, computerized nailfold video-capillaroscopy.
The main qualitative findings observed in the study population were as follow: TOR (65.7%), AVA and BIZ (62.7%), MIC (53.9%), ECT (49%), PLE (20.6%), and BLE (8.8%). The frequency of these qualitative parameters was similar in men and women (Table 3).
| Variables | Mean (SD) | p value |
|---|---|---|
| TOR | 67/102 (65.7) | .38 |
| Women | 20/34 (58.8) | |
| Men | 47/68 (69.1) | |
| AVA | 64/102 (62.7) | .052 |
| Women | 26/34 (70.6) | |
| Men | 38/68 (55.9) | |
| BIZ | 64/102 (62.7) | .52 |
| Women | 23/34 (67.6) | |
| Men | 41/68 (60.3) | |
| MIC | 55/102 (53.9) | .29 |
| Women | 21/34 (61.7) | |
| Men | 34/68 (50) | |
| ECT | 50/102 (49) | .53 |
| Women | 15/34 (44.1) | |
| Men | 35/68 (51.6) | |
| PLE | 21/102 (20.6) | 1 |
| Women | 7/34 (20.6) | |
| Men | 14/68 (20.6) | |
| BLE | 84.1 (8.8) | 1 |
| Women | 3/34 (8.8) | |
| Men | 6/68 (8.8) |
- Abbreviations: AVA, avascular zones; BIZ, bizarre-shaped capillaries; BLE, bleeding; CNVC, computerized nailfold video-capillaroscopy; ECT, ectasias; MIC, microaneurysm; PLE, subpapillary venous plexus; TOR, tortuosity.
4.5 CNVC findings and the level of glucose control
Patients with worse glucose control (HbA1c ≥7.0%) showed thicker nailfold capillaries (42.8 [9.8] vs. 38.2 [9.4] μm; p = .019) compared to those who had achieved better glucose control (HbA1c <7.0%). Shorter nailfold capillaries (174.8 [73.4] vs. 216.4 [103.8] μm, p = .021) were observed in patients with better glucose control than those with worse glucose control.
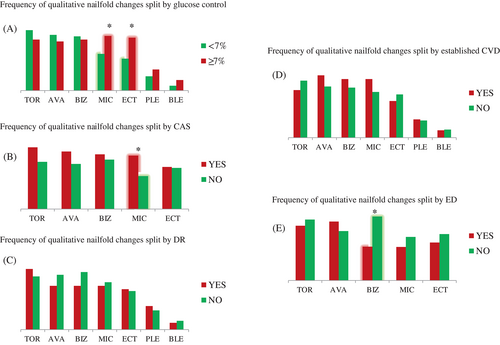
A statistically significant higher frequency of ECT (62.5% vs. 37.7%, p = .017) and MIC (64.6% vs. 43.4%, p = .045) was found in patients with worse glucose control than those with HbA1c <7.0%.
The remaining qualitative CNVC parameters were similar between the two groups.
4.6 CNVC findings and chronic diabetic complications
Patients with chronic renal impairment displayed slightly longer capillaries than those without renal impairment (219.6 [91.4] vs. 184.7 [89.9] μm), but the difference was not statistically significant (p = .07). Moreover, a lower frequency of BIZ was found in patients with ED (IIEF-5 < 17 points) compared to those without (35% vs. 68.9%, p = .02).
Patients with CAS >20% compared to those without CAS had a higher frequency of MIC (63.3% vs. 39%, p = .02). No difference in the frequency of qualitative parameters was found in patients with DR than those without DR and in patients with established CVD than those without CVD (Figure 3).
5 DISCUSSION
The CNVC is a noninvasive and easy-to-use diagnostic tool that provides real-time information on the general microvascular architecture and specific details of small nailfold vessels. Accurate nailfold examination should include the capillary density, shape, and distribution. In healthy individuals, different capillaroscopic patterns were described so that a “physiologic” nailfold appearance is challenging to be well-defined. Three healthy capillaroscopic patterns have been identified,13 including the following: (a) the “normal pattern” made up of 2–5 “U-shaped” loops and ≤2 TOR per mm2; (b) the “perfect normal pattern” composed of more than five “U shaped” loops per mm2; and (c) the “unusual normal pattern,” which includes at least one “bushy” loop, one microhemorrhage, or more than four “crossed” loops per mm2. Nevertheless, several factors may affect the nailfold microvasculature appearance including age, gender, and lifestyle habits (eg, cigarette smoking, heavy physical exercise). Therefore, a high variability in healthy and pathological findings could be expected.14
However, the CVNC examination provides valuable information about the type and severity of microvascular involvement in chronic diseases and for evaluating the efficacy of treatments. The CNVC is used to assess scleroderma spectrum disorders. In patients with systemic sclerosis, capillary abnormalities appear and evolve in a clearly defined sequence called the “scleroderma pattern,” which strongly correlates with splanchnic involvement. The CNVC findings are currently listed as one of the leading criteria to stage the severity of systemic sclerosis, according to the European League Against Rheumatism.15
Morphological remodeling of the capillary wall occurs due to specific connective damage and may also result from hydrodynamic and metabolic disorders, including T2D. Microvascular dysfunction is strictly related to hyperglycemia, and a reciprocal relationship between the two phenomena is also known.16 Patients with arterial hypertension and diabetes17 exhibit a microvascular imbalance at the level of the precapillary sphincters, leading to raised hydrostatic pressure and consequent enlargement and twisting of the capillary axis. This pathophysiological phenomenon generates crossing capillaries, one of the first signs of capillary adaptation. Another study confirmed an elevated frequency of branched/ramified capillaries and TOR in T2D.18 As recently reviewed by Maldonado et al,19 unusual nailfold capillaroscopic patterns (such as TOR, ECT, AVA, and BIZ) can also be identified in individuals with diabetes mellitus. Loss of pericytes and capillary wall enlargement are two common findings in T2D, and they lead to ECT, MIC, and BLE due to pathological increase of vascular permeability. These alterations are similar to those described in diabetes-related retinal injury.20
Extensive chronic hypoxic injury conducts to either neoangiogenesis or capillary rarefaction. The presence of nailfold PLE and BIZ is frequently described in some disorders, including T2D. PLE and BIZ result from newborn vessels developing and chaotic neoangiogenesis.21 AVA results from a capillary desertification process due to severe and extensive tissue hypoperfusion/hypoxia and insufficient neoangiogenesis restoring stimuli.
This cross-sectional study analyzed nailfold microvascular architecture and capillary details in T2D patients. Over half of the participants achieved optimal glucose control (HbA1c <7%). CAS was the most relevant chronic complication diagnosed in the study population, especially men (60%). Data are consistent with results previously described in T2D.22 The frequencies of both chronic renal impairment and DR in this study were similar to those observed by other authors (35% and 30%, respectively).23 CVD and ED were diagnosed in fewer patients (around 20%).24
The CNVC assessment showed an elevated frequency of TOR (66%), AVA (63%), BIZ (63%), MIC (54%), and ECT (49%). These findings were comparable to those observed in an Ecuadorian–Hispanic population with parallel mean age (57 [8.9] years) and evolution of T2D (around 12 years). Nailfold microvascular abnormalities were observed in 83% of the population, and TOR (63%) represented the main capillary alteration.25 However, in our study, AVA and ECT were slightly more frequent than those found by Maldonado.
Patients with worse glucose control during the examination displayed thicker and longer capillaries and a higher frequency of MIC and ECT compared to those with better control. These data support the hypothesis that glucose control could negatively affect microvasculature health at the level of the fingers.26
The so-called “diabetic nailfold capillaropathy”27 is the local expression of a systemic microvascular disorder that is characterized by pericyte damage, capillary wall enlargement and elongation, and variable structural changes, including TOR, ECT, AVA, and MIC.28 This phenomenon could be particularly more evident in patients with worse glucose control. Given the same pathogenetic hypothesis, a higher frequency of detrimental nailfold patterns should be expected in patients with chronic diabetes-related complications. Uyar et al29 found a high prevalence of TOR, ECT, and “bushy” capillaries in T2D patients with DR. The reduction of capillary length, irregular distribution, and abnormal capillaries morphology were more frequently observed in patients with prediabetes and T2D than in healthy controls, as well as in T2D patients with neuropathy compared to those without.9 Previous findings in type 1 and T2D30 also indicated a direct relationship between the severity of the retinal vascular injury and several nailfold microvasculature signs of adaptation such as ECT, MIC, and TOR. Lastly, the capillary rarefaction at rest and after brachial artery ischemia was directly associated with the level of urinary albumin excretion, resulting in an independent risk factor of the pathogenesis of microalbuminuria.31 Our data did not find a significantly higher number of capillaroscopic alterations in patients with DR and renal impairment. However, patients with ED had more AVA and fewer BIZ than those without. These findings could reflect the presence of a chronic hypoxic injury as a common pathophysiological mechanism explaining ED and finger nailfold microvascular deterioration.
Irrespective of T2D, some authors32 evaluated the relationship between nailfold microvasculature patterns (or digital flowmetry) and the severity of ED in patients with systemic sclerosis. Despite controversial results, AVA and ECT and a relevant reduction in the digital flowmetry were found in the nailfold and penile vessels of men with ED. Specific data on the relationship between nailfold microvascular patterns and penile microvascular damage in T2D are lacking, and further investigation is required to clarify this issue.
This study has some strengths and limitations. First, the cross-sectional design of this study provides only epidemiological information on a small sample of T2D individuals. Second, the CNVC examination in healthy and unhealthy subjects is affected by a relevant heterogenicity in terms of the morphological appearance of nailfold microvasculature. Moreover, the CNVC assessment significantly depends on the operator's expertise, and both may affect the accuracy when defining the architecture of nailfold microvasculature. In this study, a single-operator examination was carried out according to standardized methods before, during, and after the examination to improve the quality of nailfold images and interpretation of results (e.g., finger selection, room temperature, exposure to interfering substances such as caffeine and cigarette smoking, adequate magnification, number of captured images, selection of appropriate shots). Furthermore, the single-operator examination avoided an additional interoperator bias in describing nailfold appearance.
Automated and semiautomated systems are operated to reduce the intra- and interoperator variability of microvasculature analyses. Thanks to movement correction, selection of the frame range and positioning of the region of interest, automatic detection of capillaries, and manual correction of detected capillaries, automated algorithms,33 and machine learning significantly improve the accuracy, reproducibly, and standardization of CNVC results, also predicting diabetes-related outcomes.34
Although not yet standardized, the CVNC examination in patients with diabetes mellitus may provide further information on the microvascular injury in T2D. More research is needed to characterize better the diabetes-related nailfold microvasculature damage and its relationship with other chronic complications, such as CVD and high cardiovascular risk. For example, identifying morphological or functional capillaroscopic alterations potentially associated with silent coronary artery disease could implement current algorithms to identify patients at high risk of asymptomatic coronary artery disease. In addition, nailfold examination could be used to assess quickly and monitor the progression of complications over time and the response to antihyperglycemic treatments.
6 CONCLUSION
CNVC is an easy, inexpensive, and valuable tool to evaluate the microvasculature damage at the level of the fingers in T2D. Further studies are urgently needed to explore better the role of nailfold examination in improving the management of the disease over time. The current limitation is the interpretation of results, which could be easily overcome by using newer computerized systems to improve the automatic assessment and understanding of nailfold images.
AUTHOR CONTRIBUTIONS
Giuseppe Lisco conceived the study, collected and analyzed data, developed the database, provided statistical expertise, and drafted the manuscript. Vincenzo Triggiani read the text, provided feedback, and approved the final version.
ACKNOWLEDGEMENTS
We are grateful to Doctor Giuseppe Cicco, who provided his expertise in the field with passion and dedication.
FUNDING INFORMATION
None to declare.
CONFLICT OF INTEREST STATEMENT
There are neither competing conflicts of interest in connection with the submitted article nor industry relationship; thus, the authors deny any competing financial claim related to this study.




