Skin autofluorescence, a non-invasive biomarker for advanced glycation end products, is not related to the number of pregnancies
皮肤自发荧光强度是一种非侵入性的晚期糖基化终末产物的生物标志物, 与妊娠次数无关
Abstract
Highlights
- Skin autofluorescence (SAF) assesses subcutaneous accumulation of advanced glycation end products and has been shown to predict future cardiovascular disease and diabetes.
- A higher number of pregnancies was significantly associated with higher SAF, even after correction for relevant confounders like waist circumference, creatinine clearance, and diabetes status, but not after correction for age.
- Women with the highest SAF Z-score had a more unfavorable risk factor profile, with higher body mass index and waist circumference, higher blood pressure, lower high-density lipoprotein cholesterol, and higher triglyceride levels.
To the Editor
The role of advanced glycation end products (AGEs) in the pathophysiology of diabetes-related complications and aging has been studied extensively. The AGEs represent chronic exposure to hyperglycemia and oxidative stress. Tissue AGE accumulation can be assessed non-invasively by measuring skin autofluorescence (SAF) with a so-called AGE reader. Markers of oxidative stress are elevated during pregnancy, which can, in turn, increase the formation of AGEs.1 One study reported that SAF levels were higher in pregnant women with pre-existing diabetes than in women with gestational diabetes and women without diabetes.2
Preliminary data from our group suggested that SAF increases during pregnancy and does not return to prepregnancy levels (B. Groen et al., unpublished data, 2014). This phenomenon may be caused by increased oxidative and glycemic stress during pregnancy. Therefore, the aim of the present study was to assess the relationship between SAF and the number of pregnancies.
Methods
Subjects included in the study were participants from the Lifelines Cohort Study, a large population-based cohort study in the northern region of the Netherlands (www.lifelines.net, accessed 24 December 2017). The Lifelines study was approved by the Medical Ethics Committee of the University Medical Center Groningen. Written informed consent was obtained from all participants. The present study included women of Western European descent aged between 18 and 80 years for whom an SAF measurement was available. Subjects with type 1 and type 2 diabetes were excluded, as were as those with missing data for diabetes, leaving 47 834 individuals for analysis. Subjects completed a questionnaire on medical history, past and current diseases, use of medication, and health behavior. The questionnaire also included information on previous pregnancies and childbirth. Women were asked how many times they had been pregnant and how many children were born. In the present study, SAF was calculated as the mean of three consecutive measurements using an AGE Reader (DiagnOptics Technologies, Groningen, Netherlands).3 Age-adjusted SAF (Z-scores) was calculated because SAF is strongly affected by aging.3
Data are given as the mean ±SD or as the median with interquartile range (IQR) in the case of non-normally distributed data. Linear regression analysis was performed to examine the association between the number of pregnancies and SAF. In the multivariate models, we adjusted for relevant factors, such as waist circumference, body mass index (BMI), renal function, and smoking. Two-tailed P < 0.001 was considered significant.
Results
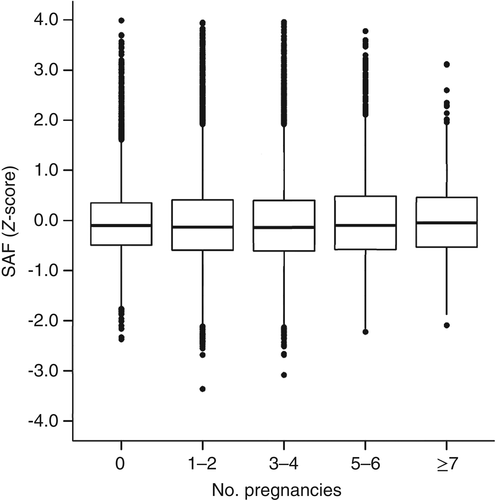
The clinical characteristics of the study population are given in Table S1, available as Supplementary Material to this paper. Mean subject age was 44 ±12 years, mean waist circumference was 87 ±12 cm, and mean BMI was 25.8 ±4.6 kg/m2. The median number of pregnancies was 2.0 (IQR 1.0–3.0). In total, 20.5% of women had not been pregnant, 42% reported one to two pregnancies, 30% reported three to four pregnancies, and 7.5% reported five or more pregnancies. A higher number of pregnancies was associated with higher SAF, which persisted after correction for waist circumference and renal function (P < 0.0001). However, after further correction for age, SAF was no longer associated with the number of pregnancies (P = 0.713; Table 1). Fig. 1 shows that SAF Z-scores are comparable in the various groups of women divided according to the number of pregnancies. Women in the highest quartile of the SAF Z-score had a higher prevalence of metabolic syndrome, as well as higher BMI, waist circumference, glucose, HbA1c, and lipids (all P < 0.01) than women in the other three quartiles, and a similar number of pregnancies compared with those in the lowest quartile (Table S2).
| Model | Parameters | β | P-value | R2 (%) |
|---|---|---|---|---|
| 1 | No. pregnancies | 0.061 | <0.0001 | 5.3 |
| 2 | No. pregnancies | 0.0003 | 0.800 | 30.7 |
| Age | 0.020 | <0.0001 | ||
| 3 | No. pregnancies | 0.0031 | <0.0001 | 19.7 |
| Waist | 0.013 | <0.0001 | ||
| GFR | −0.006 | <0.0001 | ||
| 4 | No. pregnancies | 0.030 | <0.0001 | 20.5 |
| Waist | 0.012 | <0.0001 | ||
| GFR | −0.006 | <0.0001 | ||
| Diabetes or glucose | 0.084 | <0.0001 | ||
| 5 | No. pregnancies | −0.0001 | 0.941 | 31.3 |
| Age | 0.17 | <0.0001 | ||
| Waist | 0.004 | <0.0001 | ||
| GFR | −0.001 | <0.0001 | ||
| Diabetes | 0.015 | <0.0001 |
- GFR, glomerular filtration rate.
Discussion
After correction for important confounders, SAF increased with the number of pregnancies in women from the general population. However, after correction for age, this association was no longer significant. The increased oxidative stress that occurs during pregnancy may significantly affect SAF measurements. Indeed, it has been reported that SAF is elevated in women with pre-eclampsia and associated with increased carotid artery intima–media thickness, a marker for atherosclerosis.4 Moreover, SAF was associated with higher blood pressure, triglycerides, and C-reactive protein levels, indicating the potential cardiovascular risk associated with these factors.5 Therefore, we postulate that the effect of pregnancy on SAF may only be restricted to pathological pregnancies, such as those complicated by pre-eclampsia.4, 5 Unfortunately, the Lifelines dataset did not record any complications of pregnancy.
Two important studies have reported on the association between reproductive history and cardiovascular health. One of these studies reported that a higher number of pregnancies was associated with lower cardiovascular mortality,6 whereas the other study showed that the number of pregnancies or live births was associated with higher left ventricular mass and end-systolic volume.7 A recent review suggested that pre-eclampsia is an under-recognized risk factor for ischemic heart disease, chronic hypertension, peripheral vascular disease, and stroke.8
In conclusion, in the present study SAF increased with a higher number of pregnancies, but not after correction for participants’ age. Those with the highest age-corrected SAF had a worse risk factor profile for future cardiovascular disease.
Acknowledgements
The authors acknowledge all the participants of the Lifelines Cohort Study and everybody involved in the set-up and implementation of the study. Lifelines has been funded by a number of public sources, notably the Dutch Government, The Netherlands Organization of Scientific Research NWO (Grant 175.010.2007.006), the Northern Netherlands Collaboration of Provinces (SNN), the European Fund for Regional Development, Dutch Ministry of Economic Affairs, Pieken in de Delta, Provinces of Groningen and Drenthe, the Target project, BBMRI-NL (Biobanking and BioMolecular resources Research Infrastructure The Netherlands), the University of Groningen, and the University Medical Center Groningen. This work was supported by the National Consortium for Healthy Ageing, and funds from the European Union's Seventh Framework Program (FP7/2007–2013) through the Biobank Standardisation and Harmonisation for Research Excellence in the European Union (BioSHaRE-EU) project (Grant agreement 261433). Lifelines (BRIF4568) is engaged in a Bioresource research impact factor (BRIF) policy pilot study, details of which can be found at: https://www.bioshare.eu/content/bioresource-impact-factor (accessed 24 December 2017).
Disclosure
None declared.