Awareness of high and pathological myopia among myopic patients in China: A cross-sectional multicenter survey
Jing Zhao and Bingqing Sun contributed equally to this study.
Abstract
This study aimed to investigate the awareness of high and pathological myopia among patients with high myopia. A cross-sectional multicenter survey involving both physicians and patients was conducted between February and April 2021. The outpatient education status, doctors' expectations toward patient education, patients' awareness of high/pathological myopia, and their access to relevant knowledge were inquired, and the proportions of patients with myopia, including high and pathological myopia, were assessed. In total, the survey involved 6975 physicians and patients with myopia from 161 medical institutions in China. The prevalence of high myopia among patients was 11.3%, with 22.59% having pathological myopia. Among those with pathological myopia, 22.45% experienced high myopia complications. Approximately 48.7% of the physicians believed that patients had only a vague idea about high/pathological myopia, with certain misconceptions. Additionally, most outpatients (61.4%) had no access to specialized staff for patient education. Patients' preferences and requirements for online ophthalmology information varied based on family background, medical history, and cognition toward myopia. This study demonstrated that the awareness level among patients with myopia regarding high and pathological myopia is currently insufficient. Therefore, it is important to enhance education efforts to reduce the incidence of adverse outcomes.
1 INTRODUCTION
Myopia is the most common eye disorder worldwide, with a prevalence of 85%–90% among young people in Asian countries (such as Singapore) and 25%–50% among adults in the United States and Europe.1, 2 According to data from the National Institutes of Health in the United States, approximately 23.92% of the population suffered from myopia in 2010, and this number is expected to grow by one-third by 2050.3 The prevalence of myopia in East Asia is also proliferating, reaching 2.5 billion cases in 2020.4 Notably, in East Asia, myopia progresses at an alarming rate of nearly 1 D per year during childhood, and approximately 24% of patients may develop high myopia by adulthood.1 This condition has become a global public health concern because of its potential for serious eye complications, including retinal detachment, macular choroidal degeneration, immature cataracts, and glaucoma, all of which may eventually lead to blindness.5
High myopia is a significant risk factor for pathological myopia, typically characterized by a spherical refraction diopter < −6.00 D and axial length > 26 mm, along with pathological changes in the fundus.6 With the increased severity of myopia, varying degrees of damage to the fundus structure may occur, including axial lengthening and scleral dilation. Notably, among young individuals with high myopia, the prevalence of pathological myopia is approximately 8%, and the rates of their developing blindness and low vision are as high as 22.4% and 32.7%, respectively.7
A 19-year prospective cohort study in Singapore revealed that myopia progression mainly occurred during childhood and adolescence, and fundus damage (grade 1 myopia macular degeneration) in adolescents was highly associated with early-onset myopia, high spherical refraction, and long axial length.8 Additionally, a 12-year follow-up study in China found that the earlier onset of myopia during school age was associated with a higher risk of developing high myopia in adulthood.9 As such, greater attention toward high myopia and the risk of pathological myopia is required. However, research efforts in this area have been lacking, making it impossible to devise targeted treatment plans.
Accordingly, using data collected from 6975 doctors and patients at 161 medical institutions across China, this study primarily aimed to examine the prevalence and awareness of high and pathological myopia. Moreover, it also investigated the availability of medical information, current clinical diagnosis and treatment, and patient education among patients with myopia. The findings from this study will be instrumental in planning future medical care and patient education initiatives.
2 RESULTS
2.1 Questionnaire collection
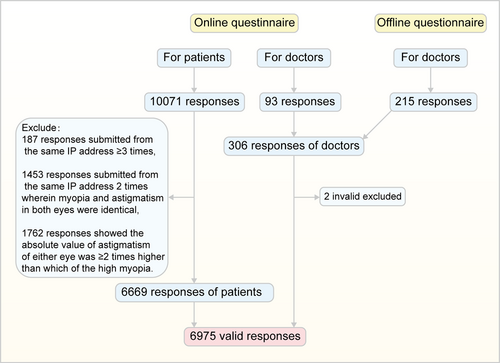
Physicians from 161 medical institutions, including primary, tertiary, specialized, and general hospitals, across 31 provinces in China participated in the survey. Patients from 31 provinces (including municipalities and autonomous regions) were also included, with 29 individuals from Hong Kong, China. The survey received a high-quality response from the majority of physicians, and only two invalid entries were excluded. In total, we collected 306 valid questionnaires from physicians, resulting in an impressive response rate of 100% and an effective rate of 99.3%. Furthermore, we collected 10,071 responses from patients, among which 6669 were valid, achieving response and effective rates of 100% and 66.2%, respectively. Combining both physician and patient responses, we gathered a total of 6975 valid responses (Figure 1).
2.2 Basic physician information
Basic physician information was collected through a doctor questionnaire. Among the 306 interviewed physicians, 78.1%, 6.5%, 12.7%, and 2.6% practiced in ophthalmology, optometry, fundus, and optician service, respectively. Most of these physicians were women (63.1%) (Supporting Information: Table S1), and the surveyed physicians represented various backgrounds in the field of ophthalmology.
2.3 Improvements needed in outpatient settings and patient education based on the doctor questionnaire
Outpatient settings, patient awareness levels, and patient education staffing were surveyed in the doctor questionnaire to provide the current state of patient education. Based on the doctor questionnaire, only 29.7% of the 161 medical institutions surveyed had specialized clinics for high myopia. Among the patients, as reported by physicians, 11.3% had high myopia, with 22.59% of them experiencing pathological myopia; in this subgroup, 22.45% had developed complications requiring medical intervention or surgery (Supporting Information: Figure S1). Regarding patient knowledge, 48.7% of patients had elementary knowledge (along with certain misconceptions) about high or pathological myopia, while approximately 30% had limited awareness of high or pathological myopia. Additionally, 61.4% of the ophthalmology, optometry, fundus, and optician service departments lacked full-time medical staff for patient education, whereas approximately 10% had specialized personnel for patient education and related video courses. Nonetheless, almost all physicians (98.4%) recognized the importance of improving patient education in the diagnosis and treatment process. Furthermore, 65.4% of physicians agreed that patient education before the onset of pathological myopia would lead to long-term benefits. However, 22.5% of them expressed concerns about the current lack of full-time educational personnel and related materials (Figure 2). These findings suggest that patient education and awareness initiatives are not well-established despite the high prevalence of high myopia/pathological myopia in outpatient settings.
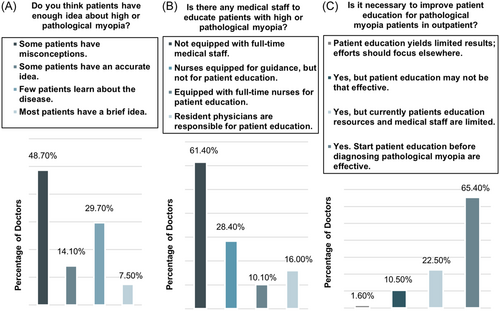
Mainly, physicians considered the following patient education topics essential: regular diagnosis, treatment, and follow-up; complications and harmfulness of pathological myopia; prevention and eye hygiene; and disease etiology and other basic knowledge. Regarding the patient education pattern, 85.3% of physicians suggested providing information manuals before and after hospital visits, 76.5% deemed self-education through authoritative online platforms appropriate, and 69.9% recommended participating in learning courses organized by medical staff. For outpatient education content, most doctors (65.7%) recommended discussing disease etiology and other basic knowledge, the harmfulness of complications, eye hygiene and disease prevention, and the importance of regular treatment and follow-up. Additionally, 12.0% of doctors suggested covering three of these items (Supporting Infromation: Figures S2 and S3). In conclusion, doctors recommended diversifying the content and format of patient education.
2.4 Myopia degree, onset time, and individual characteristics of patients
Myopia status, other eye conditions, and demographic information of patients were collected as the baseline patient information. According to patients' responses, the average equivalent sphere refractions were −7.04 D (average myopia and astigmatism were −5.82 ± 2.05 D and −2.43 ± 2.03 D, respectively) in the right eye and −7.06 D (average myopia and astigmatism were −5.76 ± 2.05 D and −2.47 ± 1.93 D, respectively) in the left eye. High myopia was diagnosed in 51.54% of patients during adolescence (between 11 and 20 years of age), 37.4% of adults aged 21–40 years, and 7.54% of children. Additionally, 46.7% of patients with high myopia had a family history through one parent, while 19.6% had a family history through both parents. Most patients (97.4%) engaged in work that demanded intensive and long-term eye use, among whom 71.9% had graduated from a college or university (Table 1). These findings suggest that both genetic and environmental factors influence myopia development and that it progresses rapidly during adolescence.
| Question | Frequency (n = 6669) | Percentage (%) |
|---|---|---|
| Location in China (subject to IP address) | ||
| East | 2241 | 33.61 |
| North | 1147 | 17.20 |
| Northeast | 707 | 10.60 |
| Central and south district | 2007 | 30.10 |
| Southwest | 380 | 5.70 |
| Northwest | 187 | 2.80 |
| Onset of myopia | ||
| ≤10 years old | 503 | 7.54 |
| 11–20 years old | 3437 | 51.54 |
| 21–40 years old | 2494 | 37.40 |
| 41–50 years old | 207 | 3.10 |
| >50 years old | 28 | 0.42 |
| Family history of myopia | ||
| No | 1206 | 18.10 |
| History through one parent | 3113 | 46.70 |
| History through both parents | 1310 | 19.60 |
| History through immediate family members except parents | 1040 | 15.60 |
| Education background | ||
| Elementary school and below | 255 | 3.80 |
| Junior/senior high school | 1622 | 24.30 |
| College or undergraduate | 4325 | 64.90 |
| Graduate and above | 467 | 7.00 |
| Work demanding intensive and long-term eye use | ||
| Yes | 6498 | 97.40 |
| No | 171 | 2.60 |
| Categories of other eye diseases diagnosed | ||
| Cataracts | ||
| Yes | 1480 | 22.20 |
| No | 5189 | 77.80 |
| Diabetic Retinopathy | ||
| Yes | 2321 | 34.80 |
| No | 4348 | 65.20 |
| Glaucoma | ||
| Yes | 2017 | 30.20 |
| No | 4652 | 69.80 |
| Age-related macular degeneration | ||
| Yes | 2348 | 35.20 |
| No | 4321 | 64.80 |
| Other | ||
| Yes | 148 | 2.20 |
| No | 6521 | 97.80 |
- Note: East China comprises six provinces and one city, that is, Shanghai, Zhejiang, Jiangsu, Anhui, Shandong, Fujian, and Jiangxi. North China is composed of two provinces, two cities, and one district, that is, Hebei, Shanxi, Beijing, Tianjin, and Inner Mongolia. Northeast China has three provinces, that is, Heilongjiang, Liaoning, and Jilin. Central South District consists of five provinces and one district, including Hubei, Hunan, Guangdong, Guangxi, Hainan, and Henan. Southwest China includes four provinces, one district, and one city, that is, Sichuan, Chongqing, Yunnan, Guizhou, Qinghai, and Tibet. Northwest China has two provinces and two districts, that is, Ningxia, Gansu, Xinjiang, and Shaanxi.
2.5 Patient diagnosis, treatment status, and relatively vague awareness of high/pathological myopia
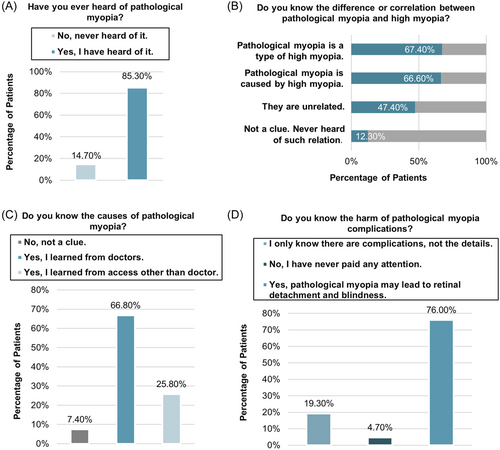
Data on diagnosis rate, patient understanding of pathological myopia, and healthcare-seeking behaviors were collected to evaluate patient awareness regarding high/pathological myopia. Among the 6669 patients who participated in the survey, 65.3% claimed to have been diagnosed with pathological myopia, and 65.9% had developed complications. Additionally, 70% of the patients received treatment for high myopia, and 40.3% received treatment for other eye diseases (Table 2). Regarding patient education, 85.3% of patients had heard of pathological myopia, 66.8% had learned about the etiology of pathological myopia from a doctor during their diagnosis and treatment, and approximately 76% understood the hazards arising from complications of pathological myopia, such as retinal detachment and blindness. In terms of awareness of myopia, 47.4% of patients thought that pathological myopia and high myopia were unrelated, 66.6% believed that pathological myopia was caused by high myopia, and 67.4% considered pathological myopia a type of high myopia (Figure 3). These findings suggest that patient awareness of pathological myopia requires further enhancement.
| Question | Frequency (n = 6669) | Percentage (%) |
|---|---|---|
| Are you diagnosed with pathological myopia? | ||
| Yes | 4353 | 65.30 |
| No | 981 | 14.70 |
| Don't know | 1335 | 20 |
| Are there any pathological complications of myopia? | ||
| Yes | 4394 | 65.90 |
| No | 1134 | 17.00 |
| Don't know | 1141 | 17.10 |
| Have you received treatments for myopia or pathological myopia? | ||
| Yes | 4666 | 70.00 |
| No | 862 | 12.90 |
| Don't know | 1141 | 17.10 |
| Have you received treatments for other eye diseases? | ||
| Yes | 2685 | 40.30 |
| No | 1649 | 24.70 |
| No other eye diseases | 2335 | 35.00 |
| Do you have regular vision checks? | ||
| Yes | 4510 | 67.60 |
| No | 1018 | 15.30 |
| Not answered | 1141 | 17.10 |
| How often do you check your vision? | ||
| Once every half a year | 1649 | 24.70 |
| Once a year | 2238 | 33.60 |
| Once every 2–5 years | 580 | 8.70 |
| Once every 5 years | 43 | 0.60 |
| Not answered | 2159 | 32.40 |
2.6 Diverse patient preferences for accessing ophthalmological information
Most patients (69.45%) obtained relevant information from the internet (including search engines and question-and-answer platforms), 57.93% from online medical platforms and official accounts of ophthalmology specialists, 52.18% from platforms of large or ophthalmology specialist hospitals, and 45.36% from private ophthalmology clinics or hospitals. Regarding eye diseases of concern, approximately half of the patients had a vague idea about glaucoma, cataracts, and vitreous degeneration; 60%–70% had limited knowledge about macular degeneration, retinopathy, and dry eye; and approximately 90% knew nothing about diabetic and other eye diseases. Most patients prioritized timely treatment, interaction with doctors, and access to authoritative sources on ophthalmology (Figure 4).
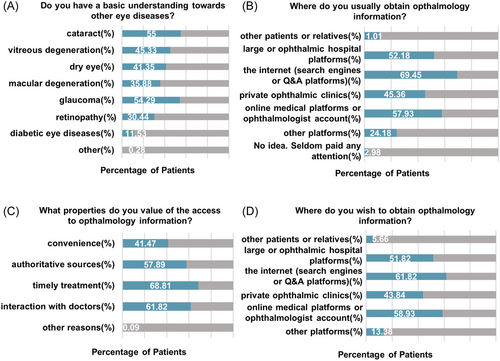
Further, the logistic regression tables regarding the patients' selection and requirements for ophthalmology information channels and their requirements for channel characteristics are presented in Supporting Information: Tables S2 and S3. Patients with both parents having myopia were less likely to choose general online information (odds ratio [OR] = 0.656, p = 0.003) or information from large hospitals or specialized ophthalmic hospital platforms (OR = 0.673, p = 0.005), and they were less concerned about the authority of the information source (OR = 0.445, p < 0.001) compared to those without myopic immediate family members. Similarly, patients with pre-existing eye diseases were less likely to choose information from large hospitals or ophthalmology specialty hospital platforms (OR = 0.767, p = 0.017), and they were less concerned about the authority (OR = 0.757, p = 0.02) and convenience (OR = 0.674, p < 0.001) of the information channels. Patients who required long-term eye use placed more emphasis on the timeliness of information updates from information channels (OR = 2.14, p = 0.003). Individuals with certain knowledge about the etiology of pathological myopia were less likely to seek information from large hospitals or ophthalmology specialty hospital platforms (OR = 0.627, p = 0.036) and were less concerned about the authority (OR = 0.333, p < 0.001) and convenience (OR = 0.582, p = 0.005) of information channels. Contrarily, patients who lacked awareness of the complications and risks associated with pathological myopia were less likely to choose general online information (OR = 0.471, p = 0.025) but were more likely to opt for information from large hospitals or ophthalmology specialty hospital platforms (OR = 2.023, p = 0.025). Patients who paid attention to ophthalmic information before and after the onset of myopia were more likely to prefer general online information (OR = 5.847, p < 0.001; OR = 2.082, p = 0.031), while those who started focusing on ophthalmic information after the onset of myopia or pathological myopia were more likely to prefer online information and official ophthalmology accounts. However, regardless of when they started paying attention to ophthalmic information, they were less likely to prefer channels from fellow patients or relatives compared to those who never paid attention. In conclusion, patients exhibited varying preferences and requirements for online ophthalmology information channels, influenced by factors such as family background, medical history, and knowledge about myopia.
3 DISCUSSION
Our survey provided comprehensive information on patients with myopia, encompassing their diagnosis and treatment, outpatient education, and awareness of high and pathological myopia in China.
Several surveys showed that the prevalence rate of pathological myopia among the young Chinese population with high myopia was approximately 8% and that up to 22.4% of these individuals would go blind.10 Our survey conducted in the hospital outpatient setting showed that 11.3% of patients had high myopia, among whom 22.59% had pathological myopia, with 22.45% of this subgroup experiencing complications that required medicinal or surgical intervention. Moreover, our study found that 51.51% of cases of high myopia occurred during adolescence. Consistently, Tricard et al. reported that the risk of high myopia can rise to 58% within 5.5 years after the initial myopia diagnosis, and children under 12 years old are at a higher risk of developing high myopia.11 Hence, effectively controlling the development of high myopia in adolescents is essential to curtail any subsequent development of pathological myopia.11
Myopia is a complex interplay between genetic and environmental factors.12 A study conducted in China found that children with a mean age of 11.45 years, who had one or both parents with myopia, had two–three times higher prevalence of myopia than did those who had no family history.13 In our study, 46.7% and 19.6% of patients with high myopia had family history through one and both parents, respectively. Li et al. reported a significant difference in myopia prevalence between children with and without parents with myopia (96.2% vs. 57.7%); the environmental and genetic indices were 0.385, indicating the importance of environmental exposure to myopia development in children. These findings highlight the significance of myopia education within families.14
Pathological myopia is characterized by progressive atrophy of the fundus, including retinal and choroidal atrophy, such as diffuse, patchy, or other patterns, which is considered the core of visual impairment.15, 16 Our survey found that the incidences of pathological myopia combined with age-related macular degeneration or diabetic retinopathy were 35.2% or 34.8%, respectively. This finding suggests that clinicians have been paying greater attention to fundus changes when assessing patients with pathological myopia. Additionally, in line with the correlation of glaucoma and cataract with myopia demonstrated previously,5 our study revealed that the incidences of glaucoma and cataract in patients with myopia were 30.2% and 22.2%, respectively. These findings highlight the importance of multidisciplinary cooperation during diagnosis and treatment.
Our survey found that 97.4% of patients with high myopia experienced long-term eye use, and 71.9% had a college education or above, indicating a strong association between work or study-associated eye use and pathological myopia. Long-time exposure to digital devices and prolonged reading have been reported to be associated with myopia due to macular choroidal thinning.17, 18 A study on myopia among students in East China revealed a nonlinear increase in the prevalence of myopia with increasing grade levels, and academic pressure was identified as an independent risk factor for myopia among young children.17 Therefore, preventive measures should be taken to limit extensive eye use, particularly among adolescents.
A French study found that most patients with myopia were initially unaware of the nature and risk of complications and wished to learn more before their conditions deteriorated.18 In our survey, physicians observed that 48.7% of patients had only a general idea about high or pathological myopia, but with certain misconceptions; 47.4% of the patients thought that high myopia was unrelated to pathological myopia, and 24% of patients did not understand the hazards of pathological myopia complications. These findings reveal the inadequacy of patient education, highlighting the urgent need to address limited patient education content, materials, and personnel.
Our data suggest that patient education should adopt a more comprehensive approach, utilizing a combination of booklets, authoritative online platforms, and lectures by medical staff. These educational means should be timely, convenient, interactive, and authoritative. Most doctors deemed online platforms useful for disseminating information on disease diagnosis and treatment, positioning them as the future hub of patient education. Additionally, financial status should be considered in making patient education accessible and relatively inexpensive. As such, online platforms have the advantage of improving the allocation of medical resources and aligning with the future of medical instruction.
Further regression analysis revealed that patients had varying preferences and requirements for online ophthalmology information channels, influenced by family background, lifestyle, and cognition toward myopia. Patients with parents who have myopia tend to avoid general online information and large hospitals or specialized ophthalmic platforms, instead focusing more on practical results and personal experience. Those who require long-term eye use value timely information updates to monitor the latest developments and treatment methods for better vision protection. Patients familiar with the causes of pathological myopia are less reliant on large hospitals or specialized platforms and pay less attention to the authority and convenience of information channels, possibly because of their existing ophthalmic knowledge. In contrast, patients who are unaware of the complications and dangers of pathological myopia prefer information from large hospitals or specialized platforms owing to their perceived authority and reliability.
Based on the current prevalence and education status of high myopia and pathological myopia in China, the following improvements should be made to the medical system. First, a systematic personal profile should be established for myopia patients, especially those with high myopia and pathological myopia among adolescents, to track the progression of their condition and provide timely interventions. Second, schools should take responsibility for educating students by implementing measures to prevent intensive eye use, encouraging good eye hygiene, and promoting outdoor exercise.19 Finally, a youth-friendly method of popularizing the science of myopia, including the use of social media, should be considered to achieve “point-to-point” communication between doctors and patients, thereby enhancing the authoritativeness, convenience, interactivity, and timeliness of patient education.
The current study had the following limitations. First, the lack of quantitative evaluation regarding the level of awareness in our study made it unable to evaluate the relationship between awareness and the progression of myopia. Second, the sample size of participating doctors was relatively small, which could be further expanded in future studies. Third, physicians were selected via simple random and cluster sampling methods; therefore, their data may not be as representative as those obtained directly from patients. Finally, the patient questionnaires were all administered online. While this approach offers convenience and the potential to collect a large sample, it can be susceptible to selection and response bias. Moreover, the credibility of the results obtained from patient questionnaires might be lower than that collected in person by physicians, as the prevalence of pathological myopia obtained from patient questionnaires was significantly higher than that reported in the literature or provided by medical staff.
4 CONCLUSION
The awareness level among patients with myopia regarding high and pathological myopia is currently insufficient. Therefore, it is important to enhance education efforts to reduce the incidence of adverse outcomes.
5 MATERIALS AND METHODS
5.1 Questionnaire
The preliminary survey was developed by two clinical physicians and subsequently modified and optimized by a third clinical physician. Next, a research team member distributed the survey questionnaires to 15 clinical doctors within our institution and 45 patients undergoing treatment at our optometry clinic. This step aimed to ensure that the phrasing of the questions did not present any comprehension difficulties; thereafter, the questionnaires were distributed. Upon receiving responses from the first 50 doctor questionnaires and 280 patient questionnaires, the internal consistency of the items was assessed, with a Cronbach's α criterion of 0.7 or higher as acceptable.
In this study, two professional questionnaires were designed, comprising single- and multiple-choice questions tailored for doctors and patients, respectively. The questionnaires were administered through the Sojump platform between February and April 2021.
The doctor's questionnaire was distributed both online and offline. The online questionnaire was obtained through random sampling of doctors' responses. In contrast, the offline questionnaire was distributed through convenience sampling. We collaborated with department heads in clinical facilities, including specialized eye hospitals, large hospitals with ophthalmology departments, and grassroots hospitals with ophthalmology services across China. Subsequently, we provided them with electronic questionnaire links to enable direct survey participation and data collection. The doctor questionnaire covered three aspects: baseline information such as their department and professional titles, details about outpatient facilities, and information on patient education status and expectations. On the other hand, the patient questionnaire was collected through random sampling and included four aspects: personal information, course of myopia, awareness of high and pathological myopia, and access to relevant knowledge. The complete questionnaires are shown in Supporting Information: Table S4.
Further, we recorded the time taken to complete the patient questionnaire and IP addresses to validate the questionnaires. The following exclusion criteria were applied to assure the quality of digital questionnaire submissions: (1) responses submitted from the same IP address ≥3 times, (2) entries submitted from the same IP address twice with identical myopia and astigmatism values in both eyes, or (3) cases where the absolute value of astigmatism in either eye was ≥2 times higher than that of high myopia.
5.2 Participants
The study participants comprised certified physicians specializing in ophthalmology and optometry and patients with myopia or those with a high risk of pathological myopia (e.g., those with high myopia and those whose degrees of spherical refraction were worse than −6 D for adults aged ≥18 years or −4 D for adolescents aged 9–17 years).
The doctors' questionnaire required the completing and authenticating of their professional qualifications to ensure professionality. The offline questionnaires targeted at doctors were distributed in ophthalmology specialist hospitals and ophthalmology departments of general or primary hospitals nationwide to ensure representativeness.
5.3 Statistical analysis
Statistical analyses were performed using SAS version 17.0 (SAS Institute). Descriptive statistics were employed to summarize all the collected responses. Data are presented as numbers (percentages) for categorical variables and means (quartiles) for continuous variables. The measurements for myopia and astigmatism are presented as means plus their corresponding standard deviation. Multinomial logistic regression models were used to explore the patients' choices and expectations regarding access to ophthalmology information.
AUTHOR CONTRIBUTIONS
Jing Zhao, Bingqing Sun, Xingtao Zhou, and Xiaoying Wang: Conception and design of the study. Zhe Zhang, Fang Liu, and Yang Shen: Statistical analysis and interpretation of data. Jing Zhao, Bingqing Sun, Zhi Chen, Yang Shen, and Peijun Yao: Illustrations. Fangwen Yang, Xiaomei Qu, and Zhiqiang Yu: Administrative, technical, or material support. Jing Zhao and Bingqing Sun: Drafting of the manuscript. Jing Zhao, Bingqing Sun, and Xingtao Zhou: Critical revision of the manuscript. Jing Zhao and Xingtao Zhou: Study supervision. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
The authors express their gratitude to all members of our lab. Additionally, we appreciate the generous support offered by the hospitals and patients who participated in our study. Moreover, we would also like to acknowledge the assistance of ChatGPT for assistance in translation services for the questionnaire and Editage (https://app.editage.cn/) for its linguistic assistance while preparing this manuscript. We created Supporting Information: Figure S1 and the graphical abstract using Adobe Illustrator 2021. Zhao received funding from the following sources: the National Natural Science Foundation of China (grant no. 82271119), the Shanghai Rising-Star Program (23QA1401000), the Healthy Young Talents Project of Shanghai Municipal Health Commission (2022YQ015), and the Project of Shanghai Science and Technology (grant no. 21Y11909800). On the other hand, Zhou was granted funding from the Project of Shanghai Science and Technology (grant no. 20410710100), the Clinical Research Plan of SHDC (SHDC2020CR1043B), and the Project of Shanghai Xuhui District Science and Technology (XHLHGG202104).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
This study was conducted from February 2021 to April 2021 and followed the principles of the Declaration of Helsinki. It was approved by the ethics committee of Eye and ENT Hospital of Fudan University, Shanghai, China, and all the participants signed an informed consent form in the questionnaire (approval number: 2020107-2).
Open Research
DATA AVAILABILITY STATEMENT
All data used in the study are already provided in the tables, figures, and online supporting information materials. The data sets used and/or analyzed during the current study are not publicly available due to the local government's policy on nondisclosure of patient information.




