Optical coherence tomography angiography features of retinal artery occlusion before and after intra-arterial thrombolysis
Qiaowei Wu and Yongyi Niu contributed equally to this work.
Abstract
Background
To evaluate the ability of optical coherence tomography angiography (OCTA) to quantitatively assess the effectiveness of intra-arterial thrombolysis (IAT) surgery for the treatment of retinal artery occlusion (RAO).
Methods
This was a prospective observational study. Patients diagnosed with RAO who received IAT were enrolled. All participants underwent comprehensive ophthalmologic examinations and OCTA scans. The best-corrected visual acuity (BCVA), vascular densities (VDs) of the superficial capillary plexus (SCP), deep capillary plexus (DCP), radial peripapillary capillaries, and central retinal thickness (CRT) were recorded. The above parameters were compared between RAO eyes and the fellow healthy eyes before and after IAT. Correlations between the BCVA and OCTA parameters in RAO eyes were calculated.
Results
Thirty-four eyes from 34 consecutive RAO patients with a mean age of 51.0 ± 12.9 years were enrolled. There was a considerable decrease of VDs in the SCP, DCP, and radial peripapillary capillaries in all RAO eyes (all p < 0.001). Compared with contralateral normal eyes, CRT was significantly increased in RAO eyes (p < 0.001). The SCP and DCP VDs were significantly improved after IAT surgery (p = 0.010 and 0.014, respectively). BCVA in logMAR unit was negatively correlated with the DCP VD (r = −0.664, p = 0.010) and positively correlated with CRT (r = 0.597, p = 0.024) after surgery, but not significantly correlated with VDs or CRT before surgery.
Conclusion
Macular and peripapillary VDs of the retina detected by OCTA were greatly decreased in RAO eyes and improved after IAT treatment. OCTA is capable of quantifying VDs in separate retinal layers non-invasively, conveniently, efficiently, and precisely.
Abbreviations
-
- BCVA
-
- best-corrected visual acuity
-
- CRT
-
- central retinal thickness
-
- DCP
-
- deep capillary plexus
-
- IAT
-
- intra-arterial thrombolysis
-
- IPL
-
- internal plexiform layer
-
- LogMAR
-
- logarithm of minimal angle of resolution
-
- NLM
-
- non-local means
-
- OCTA
-
- optical coherence tomography angiography
-
- RAO
-
- retinal artery occlusion
-
- RPC
-
- radial peripapillary capillaries
-
- SCP
-
- superficial capillary plexus
-
- VD
-
- vascular density
1 INTRODUCTION
Retinal artery occlusion (RAO) is considered to be a stroke equivalent within the spectrum of central nervous system ischemia. It is one of the most urgent and devastating ophthalmologic emergencies with extremely poor visual prognosis [1-4]. More than 90% of central RAO patients were left with a final vision of counting finger or less [5]. Without proper intervention, <20% of RAO patients have significant vision restoration with a majority displaying a visual acuity of 20/400 or worse [6]. While the diagnosis of RAO can be made simply according to pathognomonic clinical symptoms and typical fundus manifestations, the evaluation of the retinal blood flow depends solely on fundus fluorescein angiography, which is invasive, inconvenient, and time-consuming. Because of the demands on emergent managements, there has always been a lack of time for a thorough evaluation of the retinal microvasculature and perfusion before treatments. However, retinal vascular densities (VDs) reflect the extent of perfusion defects and might indicate visual prognosis; thus, it is important to visualize and quantify the retinal microcirculation to further confirm the diagnosis and to evaluate the severity of arterial occlusion to guide our treatments.
Optical coherence tomography angiography (OCTA) has been extensively used in the assessment of various ocular disorders, particularly retinal vascular diseases, because it is able to non-invasively and efficiently provide reliable and high-resolution images of the retinal vasculature. In addition, OCTA has the great capacity to quantitatively evaluate the VDs in separate retinal layers accurately and conveniently [7, 8]. However, there are few published studies on the OCTA characteristics of RAO, most of which were cross-sectional and with small sample sizes [9, 10]. In our current study, VDs in different retinal layers and around the optic disc were quantified by OCTA in eyes with RAO and were compared with fellow healthy eyes. These parameters were also compared before and after intra-arterial thrombolysis (IAT) treatment, aiming to evaluate the ability of OCTA to quantitatively assess the effectiveness of thrombolysis, and its value in monitoring RAO patients.
2 METHODS
2.1 Study design and subject
This was a prospective observational study approved by the ethics committee of Guangdong Provincial People's Hospital (No. KY2023-089-01) and conformed to the tenets of the Declaration of Helsinki. Signed informed consent was obtained from all participants. Patients diagnosed with central RAO or branch RAO who received IAT treatment in Guangdong Provincial People's Hospital from July 2021 to October 2022 were enrolled prospectively. Exclusion criteria included any previous or comorbid ocular diseases that would substantially affect the image quality of OCTA, the visual acuity or the retinal and choroidal vasculature, such as diabetic retinopathy and age-related macular degeneration, among others. The diagnosis of RAO was made according to the symptoms of sudden painless loss of vision or visual field for one eye and amaurosis fugax before the onset of vision loss, as well as signs of a pale and edematous retina, cherry-red spot at the macula, visualization of embolus in the vessels, discontinuation of retinal arteries, and papillary edema or paleness. All participants underwent comprehensive ophthalmologic examinations, including best-corrected visual acuity (BCVA), red/green color discrimination, intraocular pressure measurement, pupillary light reaction, relative afferent pupillary defect determination, slit-lamp biomicroscopy, ophthalmoscopy, fundus photography, and OCTA.
2.2 OCTA examination, measurements, and image processing
OCTA scanning was performed with the RTVue-XR Avanti (Optovue Inc.) before and in the early stage after IAT surgery. Scanning modes of Macula 6 × 6 mm and Disc 4.5 × 4.5 mm were used to evaluate the VDs of the macula and the optic disc, respectively. The retina was automatically segmented into four layers by the built-in software (Optovue Inc., AngioVue Analytics, RTVue-XR version 2018.0.0.14), and any erroneous segmentation was corrected by manual modification via the built-in “Segmentation editing and automatic propagation” function of the device. The VD in the superficial capillary plexus (SCP), designated as SCP VD, was defined as from the internal limiting membrane to 10 μm above the internal plexiform layer (IPL) according to the manufacturer's instructions. The VD in the deep capillary plexus (DCP), designated as DCP VD, was defined as from 10 μm above the IPL to 10 μm below the outer plexiform layer. The VD of the radial peripapillary capillaries (RPC) was designated as the RPC VD. Central retinal thickness (CRT) was measured from the internal limiting membrane to the retinal pigment epithelium. For images with dramatic background noises that influenced the quantification of VDs, a non-local means (NLM) noise reduction algorithm was used to decrease the noises and improve the image quality. ImageJ software (version 1.5.2a) was adopted to quantify the retinal VDs.
2.3 Statistical analysis
BCVA with a decimal chart was converted to the logarithm of the minimal angle of resolution (logMAR) for statistical analyses. All values are presented as mean ± standard deviation. We used the SPSS 20.0 (SPSS. Inc.) to perform all statistical analyses. Differences in VDs and CRT between eyes with RAO and fellow eyes were tested by Wilcoxon signed-rank test after confirming the data normality. Paired t test was applied to compare the baseline and post-treatment changes of VDs and CRT in the eyes with RAO after confirming the data normality. The correlations between BCVA and VDs and CRT in the eyes with RAO before and after IAT treatment were analyzed using Spearman correlation test. For all the tests, a p <0.05 was considered to be statistically significant.
3 RESULTS
3.1 Baseline characteristics of study participants
Thirty-four eyes from 34 consecutive RAO patients who received IAT surgery (mean age: 51.0 ± 12.9 years; females:males = 18:16) were enrolled. Demographic data and baseline information of the participants were summarized in Table 1.
| Items | Participants (n = 34) |
|---|---|
| Mean age (SD), years | 51.0 (12.9) |
| Sex | |
| Male, n (%) | 18 (52.9) |
| Female, n (%) | 16 (47.1) |
| Laterality | |
| OD, n (%) | 22 (64.7) |
| OS, n (%) | 12 (35.3) |
| Type of retinal artery occlusion | |
| Central retinal artery occlusion, n (%) | 30 (88.2) |
| Branch retinal artery occlusion, n (%) | 4 (11.8) |
| History of hypertension, n (%) | 16 (47.1) |
| History of hyperlipidemia, n (%) | 6 (17.6) |
| History of coronary heart disease, n (%) | 2 (5.9) |
| Iatrogenic causes, n (%) | 6 (17.6) |
| History of cardiac valve replacement, n (%) | 1 (2.9) |
| History of intravascular stent, n (%) | 2 (5.9) |
3.2 OCTA characteristics of RAO patients
A total of 222 OCTA images were obtained from both eyes per patients before and after surgery. Details of the OCTA images were summarized in Table 2. OCTA images were successfully obtained from 27/34 RAO eyes before and after IAT and contralateral normal eyes, whereas no valid or clear images were captured from the remaining eyes because of dramatic motion artefacts caused by loss of fixation. The most significant manifestation of OCTA images was retinal edema and scarcity of retinal vasculature. Retinal edema mainly presented as intracellular edema (diffuse intraretinal edema, 25 eyes) or mixed type (both intracellular and extracellular edema, 6 eyes), and 2 eyes displayed atrophy of retinal tissue in the acute stage. Typical OCTA images of the eye with RAO before and after IAT surgery and the contralateral normal eye of a 36-year-old woman were shown in Figure 1.
| Number of eyes | Number of scans | |
|---|---|---|
| Contralateral normal eye | 29 | 53 |
| Eye with retinal artery occlusion before IAT | 28 | 28 |
| Eye with retinal artery occlusion after IAT | 29 | 121 |
| Total | − | 222 |
- Abbreviation: IAT, intra-arterial thrombolysis.
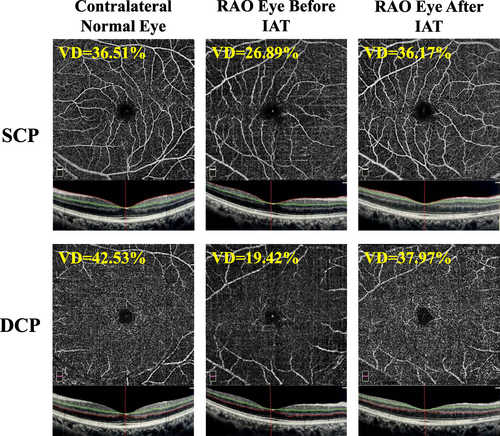
OCTA images of the eye with RAO and the contralateral normal eye of a 36-year-old woman. The OCTA images of contralateral normal eye showed normal SCP (Top left) and DCP (Bottom left) morphology. The VD in SCP and DCP was 36.51% and 42.53%, respectively. The OCTA images of RAO eyes before IAT treatment showed decreased SCP (Top middle) and DCP (Bottom middle) perfusion. The VD in SCP and DCP was 26.89% and 19.42%, respectively. The BCVA converted to the logMAR was 2.7 before IAT treatment. Two days after IAT treatment, the OCTA images of RAO eyes showed an improvement in SCP (Top right) and DCP (Bottom right) perfusion. The VD in SCP and DCP was 36.17% and 37.97%, respectively. The logMAR BCVA was 0.1 at 2 days after IAT treatment. BCVA, best-corrected visual acuity; DCP, deep capillary plexus; IAT, intra-arterial thrombolysis; logMAR, logarithm of minimal angle of resolution; OCTA, optical coherence tomography angiography; RAO, retinal artery occlusion; SCP, superficial capillary plexus; VD, vascular density.
3.3 Comparison of OCTA quantitative parameters between eyes with RAO and contralateral normal eyes
Twenty-seven patients had successful OCTA scans of both eyes before IAT treatment. The comparison of OCTA quantitative parameters between eyes with RAO and contralateral eyes is shown in Table 3. There was a considerable decrease in the SCP VD, DCP VD and RPC VD in all RAO eyes (all p < 0.0001). Compared with contralateral normal eyes, CRT was significantly increased in RAO eyes (p < 0.0001).
| Contralateral normal eye | RAO eyes before IAT | RAO eyes after IAT | p valuea | p valueb | |
|---|---|---|---|---|---|
| Mean BCVA (SD), logMAR | − | 2.52 (0.61) | 2.18 (0.85) | − | <0.001 |
| Mean RPC-VD (SD), % | 45.1 (3.0) | 32.1 (4.4) | 36.6 (7.4) | <0.001 | 0.159 |
| Mean SCP-VD (SD), % | 35.4 (5.3) | 23.1 (8.1) | 28.1 (7.4) | <0.001 | 0.010 |
| Mean DCP-VD (SD), % | 42.5 (10.2) | 27.1 (6.0) | 29.9 (3.6) | <0.001 | 0.014 |
| Mean CRT (SD), μm | 255.1 (26.7) | 354.3 (148.0) | 331.0 (123.0) | <0.001 | 0.150 |
- Note: Statistically analysis: Wilcoxon signed-rank test.
- Abbreviations: BCVA, best-corrected visual acuity; CRT, central retinal thickness; DCP, deep capillary plexus; IAT, intra-arterial thrombolysis; RAO, retinal artery occlusion; RPC, peripapillary capillaries; SCP, superficial capillary plexus; VD, vascular density.
- a Comparisons of RAO eyes versus fellow eyes.
- b Comparison of parameters in RAO eyes before versus after IAT treatment.
3.4 Comparison of OCTA quantitative parameters in RAO eyes before and after IAT treatment
Twenty-seven patients had successful OCTA scans both before and after IAT treatment. The comparison of OCTA quantitative parameters before and after IAT treatment is shown in Table 3. Generally, there was a great improvement of the SCP VD and DCP VD after IAT treatment (p = 0.014 and 0.01, respectively). The RPC VD was increased and CRT was decreased after IAT treatment, but there was no statistical significance (p = 0.086 and 0.15, respectively).
3.5 Correlation between BCVA and OCTA parameters in RAO eyes
There was a significant improvement in BCVA after IAT treatment in 22/32 eyes (the data of visual acuity of 2 eyes were missing) with an improvement rate of 68.75%. Overall, the logMAR BCVA decreased by 0.33 ± 0.54 after surgery (p = 0.002). The correlations between BCVA and OCTA parameters were shown in Table 4. LogMAR BCVA was negatively correlated with the DCP VD (r = −0.664, p = 0.010) and positively correlated with CRT (r = 0.597, p = 0.024) after surgery, but not significantly correlated with VDs or CRT before surgery.
| OCTA parameters | RPC-VD | SCP-VD | DCP-VD | Central retinal thickness |
|---|---|---|---|---|
| Before IAT | ||||
| r | 0.155 | 0.466 | 0.200 | 0.306 |
| p | 0.690 | 0.093 | 0.493 | 0.287 |
| After IAT | ||||
| r | −0.071 | −0.144 | −0.664 | 0.597 |
| p | 0.810 | 0.624 | 0.010 | 0.024 |
- Note: Statistically analysis: Spearman correlation test.
- Abbreviations: BCVA, best-corrected visual acuity; DCP, deep capillary plexus; IAT, intra-arterial thrombolysis; logMAR, logarithm of minimal angle of resolution; OCTA, optical coherence tomography angiography; RPC, peripapillary capillaries; SCP, superficial capillary plexus; VD, vascular density.
4 DISCUSSION
To the best of our knowledge, this is the first published study using OCTA to quantitatively evaluate the retinal perfusion of RAO after IAT surgery. Accurate assessment and comparison of retinal VDs before and after treatment is the most straightforward approach to evaluate the efficacy of IAT surgery. The outstanding properties of OCTA in depicting vasculature details and quantification make it the most appropriate device for RAO assessment. Our current study not only provided a detailed description of quantitative characteristics of the vasculature in acute-onset RAO in comparison with the contralateral healthy eyes, but also applied OCTA to quantify the changes of VDs in different retinal layers before and after IAT surgery. This would illustrate the value of OCTA in the evaluation of retinal arterial occlusive diseases and the efficacy of treatment as well as monitoring disease progression.
According to our knowledge of the published studies, to date, there have been few focusing on the OCTA features of RAO and perfusion changes after treatment. Bonini Filho et al. described OCTA images of seven RAO patients, which showed decreased vascular perfusion in the SCP and DCP corresponding to delayed perfusion on fundus fluorescein angiography and inner retinal changes in the optical coherence tomography-B scan [10]. Another study by Yang et al. retrospectively compared the OCTA images of 19 acute RAO patients with those of fellow eyes and normal control eyes. They discovered that the SCP VD, DCP VD, and RPC VD were significantly reduced in RAO eyes, while there was no difference in the foveal avascular zone area [9]. Hautz et al. evaluated the role of OCTA in the diagnosis and monitoring of pediatric RAO and concluded that OCTA was able to clearly visualize progressive impairment of retinal perfusion. Typical ischemic changes and loss of capillary network in the SCP and DCP were shown, and follow-up OCTA revealed an increased ischemic area and persistent arterial stenosis [11]. A case report by Wang et al showed that OCTA revealed a significantly reduced VD of the RAO eye, which improved in all quadrants at the 9-month follow-up but was still lower than that of the fellow healthy eye [12]. Rommel et al. applied OCTA to investigate the impact of ocular massage on the hemodynamics of healthy eyes and demonstrated a significant increase of retinal perfusion (SCP, DCP, and choriocapillaris) after ocular massage [13]. All this indicated that OCTA is a useful tool to evaluate the efficacy of treatments on RAO in a quantitative manner.
Different from the above published studies, our study adopted an NLM noise reduction algorithm to diminish the background noises and used ImageJ software to mark the blood flow signals and quantify VDs, instead of using the built-in software of OCTA for VD quantification, which consequently was more accurate and reliable. Similarly, the results of our current study showed that before IAT treatment, the SCP VD, DCP VD, and RPC VD were all greatly reduced compared with the fellow eyes (all p < 0.0001), which confirmed severe impairment of retinal perfusion in all layers and explained the severe vision loss as being caused by cessation of the blood and thus the oxygen supply. The thickness of central fovea was greatly increased from 255.1 ± 26.7 to 354.3 ± 148.0 μm (p < 0.0001), mainly caused by retinal edema. The majority (80.65%) of the retinal edema was of the intracellular type, presented as diffuse thickening and opacification of the inner retinal layer in the optical coherence tomography-B scan. This was consistent with the histologic findings of transient ischemic attack rat models, where apoptosis of the ganglion cell layer and inner nuclear layer of the retina were revealed but were less in the outer nuclear layer and the photoreceptor layer [14, 15]. In the present study, following IAT surgery, the SCP VD, DCP VD, and RPC VD all increased dramatically and the visual acuity improved significantly, indicating the effectiveness of IAT treatment in the early stage. However, similar to previous studies, the VDs in all retinal layers were still lower than those of the fellow normal eyes, which meant that despite efficient management, the damage to retinal microcirculation in RAO was only partially reversible [12]. Edema of the retinal tissue was slightly relieved after IAT treatment, but the reduction of CRT was not statistically significant (p = 0.15). One of the explanations might be that the edema of ischemic retinal tissue had not yet attained a peak level, such that the retinal cells still necrosed and tissues continued to swell after surgery. It was also reported that after ischemia had occurred, the retinal thickness of pig eyes increased at a rate of 25.32 μm/h, and in human eyes, the rate of retinal edema progression was 10.02 μm/h [16]. Another more important reason might be ischemia-reperfusion injury to retinal tissues in the early post-thrombolysis stage, such as spongiform edema of the IPL and cytoplasmic edema of the inner nuclear layer [17]. The findings in the present study were compatible with those published previously. In addition, our study for the first time applied OCTA to quantitatively investigate VDs in separate retinal layers after IAT treatment.
Our result showed that visual acuity (recorded as logMAR BCVA) was negatively correlated with DCP VD and positively correlated with CRT after IAT treatment, indicating that the more severe the retinal ischemia was, the more substantial the macular edema became, and the worse was the final visual acuity. Similar findings were also reported in other studies. Yang et al. found the logMAR BCVA to be positively correlated with central macular thickness but was not significantly correlated with VD in the SCP or DCP [9]. Their result was consistent with that of Ahn et al., where the baseline central macular thickness correlated significantly with the final BCVA [18].
However, according to previous published and the current studies, limitations of OCTA in the evaluation of RAO remain. The prime problem is the unavoidable motion artefacts in eyes with fixation loss during OCTA examination, which leads to poor image quality. Furthermore, the background noises would also interfere with the recognition of blood flow signals and the calculation of VD. To optimize the quality of images and improve the accuracy of VD, we adopted an NLM noise reduction algorithm to remove the signals generated by background noises and used imageJ software to quantify retinal VDs. The second difficulty lies in the inaccurate segmentation of the vascular layers caused by deterioration of the structure and optical reflectivity of the edematous retina [19]. Therefore, a shorter acquisition time, better penetration, and a more sensitive motion tracking system might be needed to improve the image quality and solve these technical problems.
5 CONCLUSIONS
Macular and peripapillary VDs of the retina detected by OCTA were greatly decreased in RAO eyes and improved significantly after IAT treatment. OCTA is capable of quantifying VDs in separate retinal layers non-invasively, conveniently, efficiently, and precisely. Therefore, OCTA has the potential to be the first-choice modality in the evaluation of retinal perfusion of RAO and efficacy of treatments.
AUTHOR CONTRIBUTIONS
Qiaowei Wu was responsible for the statistical analysis and writing of the manuscript. Yongyi Niu was responsible for clinical diagnosis and examination of the enrolled patients. Daiyu Chen was responsible for data collection and processing. Hongbin Lin and Mingkui Tan were responsible for OCTA image processing and quantification. Yijun Hu was responsible for language polishing and revision of the manuscript. Honghua Yu was responsible of clinical management of the enrolled patients and providing funding for the project. Anyi Liang was responsible for the construction, writing, and revision of the paper and data collection.
ACKNOWLEDGMENTS
We thank all the patients for their participation and cooperation. Special thanks to the intervention department of Guangdong Provincial People's Hospital for their excellent surgical management of the patients. This work was supported by National Natural Science Foundation of China (82171075), The Science and Technology Program of Guangzhou (20220610092 and 202103000045), The Outstanding Young Talent Trainee Program of Guangdong Provincial People's Hospital (KJ012019087), The GDPH Scientific Research Funds for Leading Medical Talents and Distinguished Young Scholars in Guangdong Province (KJ012019457), The Talent Introduction Fund of Guangdong Provincial People's Hospital (Y012018145), and The Launch Fund of Guangdong Provincial People's Hospital for NSFC (8217040546).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interests.
ETHICS STATEMENT
This was a prospective observational study approved by the ethics committee of Guangdong Provincial People's Hospital (No. S2023-087-01) and conformed to the tenets of the Declaration of Helsinki.
INFORMED CONSENT
Signed informed consent was obtained from all participants.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




