Efficacy and safety of arbidol (umifenovir) in patients with COVID-19: A systematic review and meta-analysis
Abstract
Objective
To provide the latest evidence for the efficacy and safety of arbidol (umifenovir) in COVID-19 treatment.
Methods
A literature systematic search was carried out in PubMed, Cochrane Library, Embase, and medRxiv up to May 2021. The Cochrane risk of bias tool and Newcastle–Ottawa scale were used to assess the quality of included studies. Meta-analysis was performed using RevMan 5.3.
Results
Sixteen studies were met the inclusion criteria. No significant difference was observed between arbidol and non-antiviral treatment groups neither for primary outcomes, including the negative rate of PCR (NR-PCR) on Day 7 (risk ratio [RR]: 0.94; 95% confidence interval (CI): 0.78–1.14) and Day 14 (RR: 1.10; 95% CI: 0.96–1.25), and PCR negative conversion time (PCR-NCT; mean difference [MD]: 0.74; 95% CI: −0.87 to 2.34), nor secondary outcomes (p > .05). However, arbidol was associated with higher adverse events (RR: 2.24; 95% CI: 1.06–4.73). Compared with lopinavir/ritonavir, arbidol showed better efficacy for primary outcomes (p < .05). Adding arbidol to lopinavir/ritonavir also led to better efficacy in terms of NR-PCR on Day 7 and PCR-NCT (p < .05). There was no significant difference between arbidol and chloroquine in primary outcomes (p > .05). No remarkable therapeutic effect was observed between arbidol and other agents (p > .05).
Conclusion
The present meta-analysis showed no significant benefit of using arbidol compared with non-antiviral treatment or other therapeutic agents against COVID-19 disease. High-quality studies are needed to establish the efficacy and safety of arbidol for COVID-19.
1 INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), has rapidly spread throughout the world leading to a pandemic.1-3 Up until now, some antiviral drugs have been proposed as promising therapeutic agents against SARS-CoV-2 infection including interferon,4 lopinavir/ritonavir,5 chloroquine,6 remdesivir,7 and arbidol.8
Arbidol (umifenovir) is an oral antiviral drug9 that was approved for prophylaxis in Russia and China several decades ago and used in the treatment of influenza A and B as well as other respiratory viral infections.10 In addition to Arbidol's antiviral and anti-inflammatory activities against various types of influenza viruses,11, 12 especially H1N1,13 its broad-spectrum antiviral activities against other viruses, such as Zika,14 Ebola,15 hepatitis B and C,16, 17 rhinovirus,18 respiratory syncytial virus,18, 19 coxsackie,18, 20 chikungunya,21 and adenovirus18 are shown in vitro and in vivo.
Regarding the SARS-CoV-2 infection, the antivirus effect of arbidol against SARS-CoV-2 has yet been controversial. On the one hand, the efficacy of arbidol was shown in vitro22, 23 which seems to have inhibited the infection more efficiently among other WHO-approved anti-influenza drugs including baloxavir, laninamivir, oseltamivir, peramivir, zanamivir23 by blocking the trimerization of the spike glycoprotein.22 Also, some studies suggested its beneficial effects either in monotherapy or combination therapy with other agents against COVID-19.5, 24-26 On the other hand, there exist other studies which have found no benefit of using arbidol in COVID-19 patients 27, 28 suggesting an urgent need to reach a conclusive decision on this matter. The present systematic review and meta-analysis aim to provide the latest evidence on arbidol's efficacy and safety compared with other therapeutic agents in COVID-19 treatment.
2 METHODS
We have registered the protocol of this systematic review and meta-analysis with the registry number CRD42020207821 and used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.29
2.1 Literature search strategy
We conducted a systematic search in the leading bibliographic databases, including PubMed, the Cochrane Library, and Embase for the relevant records up to May 2021. We also searched in medRxiv, Google Scholar, and clinical registry databases, including ClinicalTrials.gov, the European Union Clinical Trials Register, and the Chinese Clinical Trial Registry for additional relevant documents. Finally, the reference lists of the included studies and review articles were screened and the search was limited to the articles the abstract or full text of which were in English. Search terms included 2019-nCoV, SARS-CoV-2, COVID-19, arbidol, and umifenovir. The following terms were used to explore PubMed: ((((((((Coronavirus[Title/Abstract]) OR (Coronavirus[MeSH Terms])) OR (COVID-19[Title/Abstract])) OR (SARS-CoV-2[Title/Abstract])) OR (COVID-19[MeSH Terms])) OR (SARS-CoV-2[MeSH Terms])) OR (2019 novel coronavirus infection[Title/Abstract])) OR (2019-nCoV infection[Title/Abstract])) AND ((Umifenovir[Title/Abstract]) OR (Arbidol[Title/Abstract])).
2.2 Study selection
Two authors (Behnam Amani and Mahsa Zareei) independently screened the identified records based on inclusion and exclusion criteria. Disagreements between the authors were resolved by discussion among authors. The studies were included based on the following criteria: (1) patients with laboratory-confirmed positive COVID-19 test; (2) arbidol as monotherapy or in combination with other therapeutic agents; (3) any therapeutic intervention as a comparison (4); efficacy and safety outcomes of interest. The primary efficacy outcomes were the negative rate of PCR (polymerase chain reaction) and PCR negative conversion time and the secondary efficacy outcomes included the rate of improvement on chest CT, rate of cough alleviation, length of hospital stay, and disease progression. The safety outcome was the incidence of adverse events reported in patients; and (5) clinical trials or observational studies. The exclusion criteria were the studies conducted on animal models, case reports, case series, letters to editors, and editorials.
2.3 Data extraction and quality assessment
We used the Cochrane collaboration tool to assess the risk of bias of randomized clinical trials.30 Quality assessment of observational studies was conducted using the Newcastle–Ottawa scale (NOS).31 We extracted data using the same data extraction form. The extracted data included (1) study characteristics (author, year, setting, and design); (2) patient's characteristics (sample size, sex, and age); (3) intervention and comparison (sample size); and (4) efficacy and safety outcomes. All steps were performed independently by two authors (Behnam Amani and Mahsa Zareei).
2.4 Evidence synthesis
We performed a meta-analysis using RevMan software, version 5.3. The mean difference (MD) with a 95% confidence interval (CI) was used for continuous variables and a risk ratio (RR) with 95% CI for dichotomous variables. The statistical heterogeneity was evaluated using the I2 and Chi2 tests. The random-effects model was used for studies with I2 > 50% or p < .1. Otherwise, we used the fixed-effect model.
3 RESULTS
3.1 The characteristics of studies
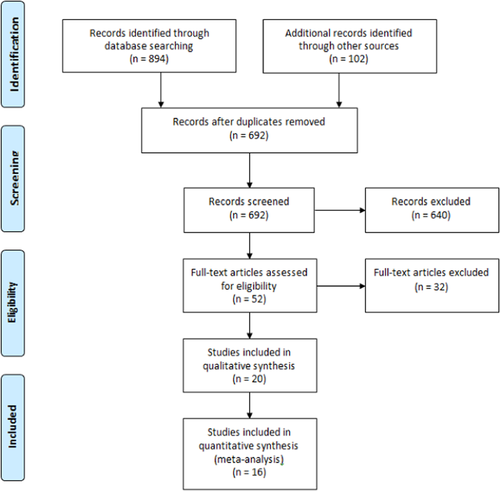
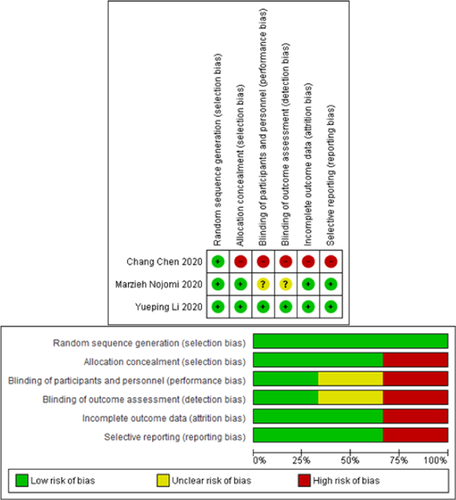
Figure 1 shows the literature search flow, removal of duplicates, and the screening based on title, abstract, and full text. As a result, 52 full-text articles were reviewed and sixteen studies24, 32-46 entered the final analysis. The characteristics of the studies included in the systematic review are presented in Table 1. Assessment of the risk of bias using the Cochrane collaboration tool is presented in Figure 2.
| Study, year | Country | Design | Age (mean) | N (M/F) | Intervention (n) | Comparison (n) | NOS |
|---|---|---|---|---|---|---|---|
| Chang Chen 2020,47 | China | RCT | NA | 236 (110/126) | Arbidol (120) | Favipiravir (116) | RoB 2 |
| Huang 2020,24 | China | R | NA | 27 (12/15) | Arbidol (11) | LPV/r (6), CQ (10) | 7 |
| Lisi Deng 2020,33 | China | R | 44.5 | 33 (17/16) | Arbidol + LPV/r (16) | LPV/r (17) | 8 |
| Ping Xu 2020,42 | China | R | 51.9 | 141 (74/67) | Arbidol + IFN (71) | IFN (70) | 6 |
| Qibin Liu 2020,25 | China | R | 59.5 | 504 (259/245) | Arbidol (257) | Os (66), LPV/r (259) | 6 |
| Qiong Zhou 2020,44 | China | R | NA | 77 (31/46) | Arbidol (24) | Arbidol + IFN (46), IFN (7) | 7 |
| Wenyu Chen 2020,48 | China | RCT | NA | 62 (34/28) | Arbidol + control (42) | Control (20) | RoB 2 |
| Kaijin Xu 2020,26 | China | R | NA | 111 (47/64) | Arbidol + ER (49) | ER (62) | 7 |
| Xiu Lan 2020,35 | China | R | 55.8 | 73 (37/36) | Arbidol + LPV/r (39) | LPV/r (34) | 7 |
| Jun Chen 2020,34 | China | R | 48 | 134 (69/65) | Arbidol (34) | LPV/r (52), non-antiviral (48) | 5 |
| Xudan Chen 2020,32 | China | R | 48 | 284 (131/153) | Arbidol (37) | Control (121), LPV/r (60), arbidol + LPV/r (16), CQ (17), Os (13), Other (16) | 9 |
| Yaya Zhou 2020,45 | China | R | 55.5 | 238 (102/136) | Arbidol (82) | Arbidol + IFN (139) | 7 |
| Yueping Li 2020,37 | China | RCT | 49.4 | 86 (40/46) | Arbidol (35) | LPV/r (34), control (17) | RoB 2 |
| Zhu 2020,46 | China | R | 39.8 | 50 (26/24) | Arbidol (16) | LPV/r (34) | 7 |
| Wen 2020,41 | China | R | 49.9 | 178 (81/97) | Arbidol (36) | LPV/r (59), control (58), arbidol + LPV/r (25) | 7 |
| Ming Li 2021,36 | China | R | NA | 62 (24/38) | Arbidol (42) | CQ (20) | 7 |
| Jie 2021,49 | China | R | 65 | 252 (106/146) | Arbidol (228) | No arbidol (24) | 8 |
| Ruan 2021,50 | China | R | 64 | 331 (160/171) | Arbidol (273) | Non-antiviral (58) | 8 |
| Ghaderkhani 2021,51 | Iran | RCT | NA | 53 (32/21) | HCQ + arbidol (28) | HCQ (25) | RoB 2 |
| Nojomi 2020,40 | Iran | RCT | 56.4 | 100 (60/40) | Arbidol (50) | LPV/r (50) | RoB 2 |
| Lian 2020,38 | China | R | 60 | 81 (45/36) | Arbidol (45) | Control (36) | 8 |
| Liu 2021,39 | China | R | 54.8 | 108 (47/61) | Arbidol (40) | Arbidol + LHQW (68) | 8 |
| Jing Chen 2020,52 | China | R | NA | 200 (130/70) | Arbidol + SFJDC (100) | Arbidol (100) | 8 |
| Fang 2020,53 | China | R | 61.5 | 162 (87/75) | Arbidol + LHQW (113) | LHQW (49) | 8 |
| Ping 2020,43 | China | R | NA | 295 (171/124) | Arbidol (148) | LHQW + arbidol (147) | 8 |
| Xiang-Kun 2020,54 | China | R | NA | 70 (41/29) | Arbidol (30) | SFJD + arbidol (40) | 9 |
- Abbreviations: CQ, chloroquine; ER, empirical regimens; F, female; HCQ, hydroxychloroquine; IFN, Interferon; LPV/r, lopinavir/ritonavir; LHQW: Lianhuaqingwen; M, male; N, number; NA, not acquired; Os, oseltamivir; R, retrospective; RCT, randomized clinical trial; RoB, risk of bias; SFJD, Shufeng Jiedu.
3.2 Comparisons
3.2.1 Arbidol versus non-antiviral treatment
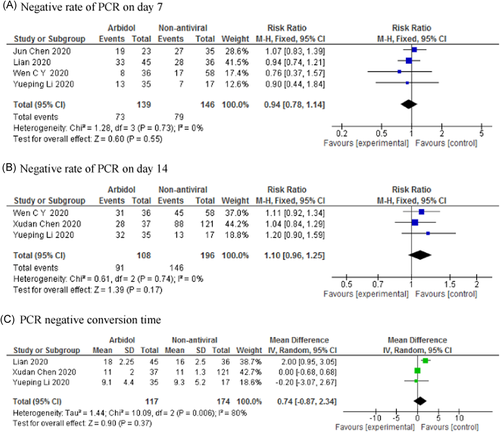
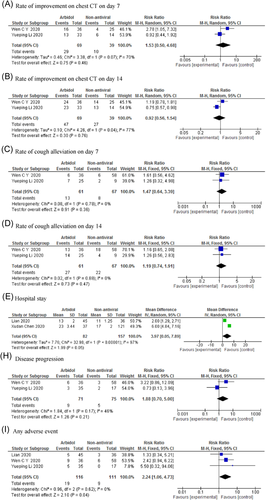
The result of meta-analysis showed that there was no significant difference between arbidol and non-antiviral groups in terms of negative rate of PCR on Day 7 (RR: 0.94; 95% CI: 0.78–1.14; p = .55) and Day 14 (RR: 1.10; 95% CI: 0.96–1.25; p = .17), PCR negative conversion time (MD: 0.74; 95% CI: −0.87 to 2.34; p = .37) (Figure 3), rate of improvement on chest CT on Day 7 (RR: 1.53; 95% CI: 0.50–4.68; p = .46) and Day 14 (RR: 0.92; 95% CI: 0.56–1.54; p = .76), rate of cough alleviation on Day 7 (RR: 1.47; 95% CI: 0.64–3.39; p = .36) and Day 14 (RR: 1.19; 95% CI: 0.74–1.91; p = .47), hospital stay (MD: 3.97; 95% CI: 0.05–7.89; p = .05), and disease progression (RR: 1.88; 95% CI: 0.70–5.00; p = .21; Figure 4). Arbidol was associated with higher adverse events (RR: 2.24; 95% CI: 1.06–4.73; p = .04; Figure 4).
3.2.2 Arbidol versus favipiravir
Only one study47 compared arbidol with favipiravir. The result showed no significant difference between arbidol and favipiravir groups in the clinical recovery rate. However, favipiravir was associated with better efficacy in relieving pyrexia and cough. The frequencies of drug-related adverse events for arbidol and favipiravir were 23.33% and 31.9%, respectively.
3.2.3 Arbidol versus chloroquine
There was no significant difference between arbidol and chloroquine in terms of negative rate of PCR on Day 14 (RR: 1.27; 95% CI: 0.64–2.51; p = .50) and PCR negative conversion time (MD: 0.69; 95% CI: −3.72 to 5.10; p = .76; Table 2). However, the length of hospital stay in patients taking chloroquine was significantly shorter than patients taking arbidol (MD: 4.59; 95% CI: 0.58–8.60; p = .02; Table 2).
| Analysis | No. of studies | Participants | Pooled estimate (95% CI) | p | Heterogeneity | ||
|---|---|---|---|---|---|---|---|
| Ch2 | p | I2 | |||||
| Sensitivity analysis | |||||||
| Arbidol versus non-antiviral | |||||||
| Negative rate of PCR | 4 | 405 | 1.21 (1.06–1.38) | .005 | 5.79 | .12 | 48% |
| Arbidol versus chloroquine | |||||||
| Negative rate of PCR on Day 14 | 3 | 137 | 1.27 (0.64–2.51) | .50 | 12.54 | .002 | 84% |
| PCR negative conversion time | 2 | 75 | 0.69 (−3.72 to 5.10) | .76 | 14.71 | .0001 | 93% |
| Hospital stay | 2 | 75 | 4.59 (0.58–8.60) | .02 | 8.44 | .004 | 88% |
| Arbidol versus LPV/r | |||||||
| Negative rate of PCR on Day 7 | 4 | 276 | 1.35 (1.03–1.76) | .03 | 4.18 | .24 | 28% |
| Negative rate of PCR on Day 14 | 5 | 328 | 1.47 (1.06–2.04) | .02 | 24.07 | <.0001 | 83% |
| PCR negative conversion time | 5 | 328 | −2.28 (−3.83 to −0.72) | .004 | 21.91 | .0002 | 82% |
| Hospital stay | 3 | 214 | −1.87 (−8.01 to 4.27) | .55 | 50.39 | <.00001 | 96% |
| Rate of improvement on chest CT on Day 7 | 2 | 156 | 1.14 (0.77–1.69) | .50 | 0.29 | 0.59 | 0% |
| Rate of improvement on chest CT on Day 14 | 2 | 156 | 0.99 (0.80–1.23) | .92 | 0.24 | 0.62 | 0% |
| Disease progress | 2 | 164 | 1.08 (0.13–9.29) | .94 | 5.64 | 0.02 | 82% |
| Rate of cough alleviation on Day 7 | 2 | 141 | 1.61 (0.21–12.22) | .64 | 5.48 | 0.02 | 82% |
| Rate of cough alleviation on Day 14 | 2 | 141 | 0.81 (0.58–1.15) | .24 | 0.32 | 0.57 | 0% |
| Adverse events | 5 | 367 | 0.44 (0.28–0.68) | .0002 | 2.70 | 0.61 | 0% |
| Arbidol + LPV/r versus LPV/r | |||||||
| Negative rate of PCR on Day 7 | 2 | 117 | 2.06 (1.13–3.76) | .02 | 0.01 | 0.91 | 0% |
| Negative rate of PCR on Day 14 | 3 | 193 | 0.99 (0.55–1.80) | .99 | 9.44 | 0.009 | 79% |
| PCR negative conversion time | 3 | 229 | 2.21 (−0.13 to 4.54) | .06 | 6.61 | 0.04 | 70% |
| Hospital stay | 2 | 145 | 1.51 (−3.94 to 6.97) | .59 | 6.46 | 0.01 | 85% |
| Rate of imrovement on chest CT on Day 7 | 2 | 117 | 1.05 (0.20–5.50) | .96 | 6.99 | 0.008 | 86% |
| Arbidol versus arbidol + IFN | |||||||
| PCR negative conversion time | 2 | 291 | −0.99 (−16.67 to 14.69) | .90 | 715.70 | <.00001 | 100% |
| Arbidol + IFN versus IFN | |||||||
| PCR negative conversion time | 2 | 194 | 2.31 (−7.78 to 12.40) | .65 | 28.11 | <.00001 | 96% |
| Arbidol + LHQW versus arbidol | |||||||
| Rate of improvement on chest CT | 2 | 403 | 1.27 (0.88–1.85) | .20 | 2.91 | 0.09 | 66% |
- Abbreviations: CI, confidence interval; IFN, interferon; LHQW, Lianhuqingwen; LPV/r, lopinavir/ritonavir; P, p-value; PCR, polymerase chain reaction.
3.2.4 Arbidol versus oseltamivir
Chen et al.27 found that the clearance rate of arbidol and oseltamivir during 14 days were 75.7% and 61.5%, respectively. The median length of hospital stay in both groups was similar. The result of another study25 showed that arbidol was more effective than oseltamivir in reducing mortality. Also, arbidol was more effective in the reduction of lesion size (46.43% vs. 41.18%).
3.2.5 Arbidol versus lopinavir/ritonavir
Arbidol showed better efficacy compared to lopinavir/ritonavir in terms of negative rate of PCR on Day 7 (RR: 1.35; 95% CI: 1.03–1.76; p = .03) and Day 14 (RR: 1.47; 95% CI: 1.06–2.04; p = .02), as well as PCR negative conversion time (MD: −2.28; 95% CI: −3.83 to − 0.72; p = .004; Table 2). However, there was no significant difference between two drugs in terms of rate of improvement on chest CT on Day 7 (RR: 1.14; 95% CI: 0.77–1.69; p = .50) and Day 14 (RR: 0.99; 95% CI: 0.80–1.23; p = .92), rate of cough alleviation on Day 7 (RR: 1.61; 95% CI: 0.21–12.22; p = .64) and Day 14 (RR: 0.81; 95% CI: 0.58–1.15; p = .24), hospital stay (MD: −1.87; 95% CI: −8.01 to 4.27; p = .55), and disease progression (RR: 1.08; 95% CI: 0.13–9.29; p = .94; Table 2). Compared with lopinavir/ritonavir, arbidol had fewer adverse events (RR: 0.44; 95% CI: 0.28–0.68; p = .0002; Table 2).
3.2.6 Arbidol plus lopinavir/ritonavir versus lopinavir/ritonavir
Arbidol combined with lopinavir/ritonavir versus exclusive administration of lopinavir/ritonavir was associated with higher negative rate of PCR on Day 7 (RR: 2.06; 95% CI: 1.13–3.76; p = .02; Table 2). However, no significant effect was observed between two administrations in terms of negative rate of PCR on Day 14 (RR: 0.99; 95% CI: 0.55–1.80; p = .99), PCR negative conversion time (MD: 2.21; 95% CI: −0.13 to 4.54; p = .06), rate of improvement on chest CT on Day 7 (RR: 1.05; 95% CI: 0.20–5.50; p = .96), and hospital stay (MD: 1.51; 95% CI: −3.94 to 6.97; p = .59; Table 2).
3.2.7 Arbidol and interferon
The meta-analysis result showed no significant difference between exclusive arbidol and interferon/arbidol combination regarding the PCR negative conversion time (MD: −0.99; 95% CI: −16.67 to 14.69; p = .90; Table 2). Also, interferon/arbidol combination showed no beneficial effect compared with interferon alone regarding PCR negative conversion time (MD: 2.31; 95% CI: −7.78 to 12.40; p = .65; Table 2).
3.2.8 Arbidol combined with traditional Chinese medicines
Several studies52-54 compared the efficacy of arbidol as a combination therapy with traditional Chinese medicines. The meta-analysis of improvement rate of chest CT found no greater benefit of arbidol combined with Lianhuaqingwen compared to arbidol alone in the treatment of COVID-19 patients (RR: 1.27; 95% CI: 0.88–1.85; p = .20; Table 2). Fang et al.53 found that the simultaneous treatment of arbidol and Lianhuaqingwen was associated with higher improvement in patients with moderate COVID-19 compared with Lianhuaqingwen alone. There are other studies52, 54 that reported the efficacy and safety of Shufeng Jiedu capsule combined with arbidol versus arbidol alone in patients with COVID-19.
3.2.9 Sensitivity analysis
We conducted a sensitivity analysis by including the case-series study55 (Table 2).
4 DISCUSSION
This study aimed to provide the latest available evidence on the efficacy and safety of arbidol in the treatment of COVID-19 disease. The meta-analysis results showed that arbidol had no clinical efficacy for all primary and secondary outcomes, including the negative rate of PCR, PCR negative conversion time, rate of improvement on chest CT, cough alleviation, hospital stay, and disease progression.
Similar to our finding, a meta-analysis by Huang et al.56 indicated that arbidol was not associated with significant improvement in terms of efficacy outcomes but for the negative rate of PCR on Day 14 compared to the control group. However, they performed a subgroup analysis only on primary outcomes based on without or with antiviral drugs.
In another similar meta-analysis done by Li et al.,27 arbidol was associated with a higher negative rate of PCR compared with control in patients with COVID-19. Nevertheless, this study found no efficacy for PCR negative conversion time and improvement rate on chest CT and progression disease. The finding of these meta-analyses for the negative rate of PCR contrast with our findings due to the differences in control groups. In fact, the present study boasts specified control subgroups in which each non-arabidol treatment was considered as a separate control group, but other studies take more general categories into accounts such as all non-arabidol treatments in Huang et al.'s study and all other antiviral/no antiviral drugs in the one done by Li et al. It should be noted that the inclusion of different interventions in a control group in the meta-analysis may cause problems including the risk of bias, heterogeneity, and imprecision, which finally affect the interpretation of findings.57
Although the present study found no significant treatment benefit for arbidol compared with non-antiviral interventions, recent findings from two studies5, 58 have suggested its efficacy and safety for prophylaxis in patients with COVID-19. The result of a clinical and laboratory data analysis also58 showed that arbidol improved SARS-CoV-2 infection though without any effect on the hospitalization rate. Zhang et al.5 found that arbidol was associated with the improvement in SARS-CoV-2 infection. It seems that more evidence is needed to approve the potential of arbidol for prophylaxis of COVID-19.
Based on the meta-analysis results, arabidol showed different efficacies in various outcomes in comparison to other treatments. Arbidol was not more effective than chloroquine in the negative rate of PCR and PCR negative conversion time. Also, chloroquine led to a shorter length of hospital stay than arabidol. However, arbidol showed better efficacy than oseltamivir in terms of the negative rate of PCR, the length of hospital stay, and the mortality rate. Compared with lopinavir/ritonavir, arbidol had better efficacy in the negative rate of PCR and PCR negative conversion time, and also was associated with fewer adverse events, with no significant difference between them for other efficacy outcomes.
Our meta-analysis showed that adding arbidol to lopinavir/ritonavir increased the negative rate of PCR on Day 7 and decreased PCR negative conversion time compared to lopinavir/ritonavir alone. Furthermore, simultaneous prescription of arbidol with interferon has no effect on the PCR negative conversion time in patients. Similar results were also found for interferon as a combination therapy with arbidol. The present meta-analysis found no benefit for arbidol in combination with traditional Chines medicine. However, more studies are needed to approve this therapeutic alternative. The meta-analysis of Huang et al.56 found no significant adverse events for arbidol. However, in our study arbidol was associated with higher adverse events in patients.
5 LIMITATIONS
Despite the efforts to minimize limitations, there were still several limitations to the current study. One of the challenging limitations of our study was the study design. Studies conducted were mostly retrospective and associated with a higher risk of bias. To reduce bias, we applied some strategies recommended by Almeida et al.59 Another important limitation was the location of the studies. The majority of studies were conducted in China, which makes our findings prone to a selection bias. Finally, we could not perform subgroup analyses on variables such as the severity of illness, dosage, sample size, and other variables due to an insufficient number of available studies.
6 CONCLUSION
The finding of this meta-analysis revealed that arbidol was not superior to non-antiviral treatment in patients with COVID-19. Compared with lopinavir/ritonavir, arbidol showed better efficacy for primary outcomes. No remarkable treatment effect was observed compared with other therapeutic agents. A well-designed randomized controlled trial with a large sample size is necessary to conclude the efficacy and safety of arbidol against COVID-19.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Ahmad Khanijahani for his contribution during the preparation of this study.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Study concept and design: Bahman Amani and Behnam Amani. Literature searching: Bahman Amani and Behnam Amani. Study selection and appraisal: Behnam Amani and Mahsa Zareei. Data extraction: Sara Zareei and Mahsa Zareei. Data analysis and interpretation: Bahman Amani and Behnam Amani. Critical revision of the manuscript: Sara Zareei. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Open Research
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are included within the Supporting Information file.




