Cervical collar use in spinal cord injury management
Abstract
Background
The use of cervical collars in the management of acute cervical spine injuries has been part of standard practice in the trauma setting for decades, aimed at preventing secondary injuries.
Objectives
To review the recent evidence challenging the routine use of cervical collars, addressing the limited scientific support, associated risks, and guidelines for their use.
Methods
A comprehensive literature review was conducted, analyzing recent studies and guidelines from authoritative bodies such as the American Association for Neurological Surgeons and the Congress of Neurological Surgeons. The review focused on the efficacy, risks, and recommendations regarding cervical collar use in acute cervical spine injuries.
Results
Recent evidence questions the routine use of cervical collars, highlighting limited scientific support and several associated risks, including pressure ulcers and decreased venous return. Cervical collars may also be contraindicated in individuals with abnormal spinal structures, such as those with Ankylosing Spondylitis. The efficacy of cervical collars is debated, particularly concerning undiagnosed spinal fractures, where delayed diagnosis can result in permanent injuries. Despite these risks, cervical collars may be beneficial in low-resource areas and when used effectively with early clearance post-injury. Current guidelines recommend immobilizing patients suspected of cervical spine injury but stress the importance of proper evaluation of the need for immobilization. Recent guidelines advocate for spinal motion restriction over traditional immobilization, emphasizing the need for better risk assessment and implementation strategies.
Conclusions/Clinical Importance
Re-evaluating the routine use of cervical collars is crucial due to potential risks and limited supporting evidence, with a focus on individualized assessment and adherence to updated guidelines favoring spinal motion restriction.
1 INTRODUCTION
Spinal cord injury (SCI) affects 250 000 to 500 000 new people every year around the world, with 17 000 new cases in the US every year.1 Motor vehicle accidents causing 38% and falls causing 30%, constitute the most likely cause of an SCI. Other causes are falls, violence such as gunshot wounds, and sports-related accidents.1 Risk is increased by underlying spinal diseases such as cervical spondylosis, ankylosing spondylitis, atlantoaxial instability, congenital conditions, osteoporosis, and spinal arthropathies.2, 3
During an event causing an acute SCI, there is pathologic stress on the spine such as extreme flexion, rotation, extension, or compression.2 Through this, SCIs also occur alongside other spinal injuries such as fractures, dislocations, tearing of ligaments, and/or disruption and/or herniation of intervertebral discs. This leaves the cervical spine unstable, leaving the patient vulnerable to further SCI.4 This initial damage occurs during the primary injury. Progressively, the effects of the secondary injury may continue to cause neurological damage. This mechanism is based on ischemia, hypoxia, inflammation, oedema, excitotoxicity, disturbance of ion homeostasis, and apoptosis.
Spinal stabilization is important in reducing the risk of new or worsening SCI while the cervical spine is unstable.5 Along with preventing pain from primary injury, cervical spinal stabilization can prevent quadriparesis or quadriplegia from cervical spinal injury (CSI). Besides stabilization of the spine, care may include mean arterial pressure augmentation with vasopressors, cerebrospinal fluid diversion using drains and intracranial pressure (ICP) monitors, and the use of methylprednisolone (MP) steroid use. Although, the use of MP has minimal scientific evidence supporting its use.5
Decreased movement of the spine is achieved as soon as possible after the injury right alongside the establishment of a free airway.6 Cervical collars have been used to prevent secondary injuries when the cervical spine is not stable.
2 OVERVIEW OF CERVICAL COLLARS
2.1 Cervical collar uses
Cervical collars are commonly used for spinal immobilization in patients with known or suspected SCI.5 The intended function of cervical collars in SCI is to prevent further injury by stabilizing the cervical spine while it is vulnerable and unstable. Cervical collar use has decreased in the past decade with increased research on poor outcomes with inappropriate use. Inappropriate use of cervical collars can lead to pressure ulcers and muscle atrophy in the neck leading to more instability and psychological dependence for the patient.7, 8 There is a remaining need for a standardized protocol to better identify and manage patients with a clear benefit from cervical collars.
2.2 Types of collars
The two broad categories of cervical collars are rigid and soft cervical collars.9 Rigid cervical collars are used after surgery or serious injury and are made of hard plastic and foam, usually including a process for chin support. They are commonly used to keep the neck immobile while it heals. Soft cervical collars are used for pain management and are made of foam. Their purpose is to limit flexion and extension while supporting the neck.9
2.3 New improvements
New improvements in cervical collars have been focused on the integration of technology to make smart collars. Collars with motion sensors, Bluetooth, and WiFi capabilities provide opportunities for focused feedback and individualized patient care based on data collected from the collar itself. This data could also be streamed to apps for patients and providers to have the ability for continuous monitoring.10
The wide use of electronics and the shift in lifestyles during the COVID-19 pandemic sparked conversations about posture and its physiological effects becoming an area of concern, leading to the idea of dynamic braces. These braces would be capable of providing support as well as traction while also assessing stiffness in the head and neck. A preliminary prototype was studied in Egypt in 2022.11, 12
Future studies may focus on finding or engineering better materials to use in cervical collars to avoid humidity and temperature-related damage to the skin while also balancing the need for structural support and comfort to protect the stability of the spine while avoiding pressure ulcers.7
2.4 Current guidelines for cervical collar use in spinal cord injury
According to the life support guidelines provided by the American College of Surgeons (ACS) and the prehospital life support guidelines provided by the National Association of Emergency Medical Technicians (NAEMT), the use of collars has remained largely unchanged for more than 30 years.6 The standard use of collars remains regarded as crucial and is established as the fundamentals of major trauma and a first measure of action alongside guaranteeing a free airway.6 Initially introduced to prevent secondary SCIs, collars are now a common practice in modern prehospital care for trauma patients.6 Despite widespread use, the evidence supporting collar usage is limited, with a lack of randomized, controlled trials (RCTs) to establish its impact on mortality, neurological injury, and spinal stability, as noted in a Cochrane review from 2001.6
Additionally, there is a growing body of evidence and opinion against the routine use of collars.6 The American Association for Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS) Joint Guidelines Committee recently published a comprehensive update of the Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injury.6 In the prehospital setting, the AANS/CNS suggests immobilizing all trauma patients suspected of cervical spine injury (CSI) or SCI.6 However, it is recommended that experienced personnel evaluate the need for immobilization during transport.6 Patients who are fully alert, communicative, not intoxicated, devoid of neck pain or tenderness, neurologically intact, and without distracting injuries should forgo immobilization.6 The preferred approach involves using a rigid collar and supportive blocks on a spine board with straps.6 It is discouraged to rely solely on sandbags and tape, and spinal immobilization is not advised for patients with penetrating trauma.6
Currently, there is ongoing debate about the use of neck collars to immobilize trauma patients with potential spinal injuries due to lack of evidence. A population subset that has been studied are patients who have experienced undiagnosed spinal fractures. In one large multi-centre study, it was found that missed CSI resulting in neurological deficits was rare, occurring in less than 1 out of 500 spine injury cases and 1 out of 4000 trauma cases.13 The average delay in diagnosing these injuries was around 20 days.13 However, reports suggest that the delayed diagnoses of cervical fractures resulted in permanent and severe deficits. For instance, one study involving over 32 000 trauma patients with 740 cervical injuries noted 34 missed injuries, with 10 patients developing permanent deficits (29%).14 Another study with 367 cervical injuries reported 18 missed injuries, leading to 8 patients experiencing neurological symptoms and 2 developing permanent deficits (11%).15 One study noted how the neurological status of patients with SCI has been improving ever since the 1970s. Approximately, 55% of patients referred to SCI centres arrived with neurological lesions, whereas in the 1980s, the number increased to 39%.16 There is yet no specific evidence to support whether the decrease in SCI is from EMS protocol or if it is due to improvements in automobile safety and design.16
Recent traction has been shifting guidelines toward spinal motion restriction (SMR).16 The ACS Committee on Trauma, NAEMT, and ACEP, have released a unified statement endorsing SMR over traditional immobilization for trauma patients.16 The consensus among the groups is that the current methods used do not effectively prevent spinal movement, thus, SMR aims to better protect injured spines by minimizing unnecessary motion.16 Although the panel did not note any instances of neurological decline due to insufficient out-of-hospital immobilization, there have been cases reported of deterioration and mortality in ankylosing spondylitis (AS) patients wearing cervical collars.16 These individuals, who have bony vertebral bridging, have a heightened risk as collars can put further stress on unstable areas of the spine, warranting a contraindication of their use, thus, rigid collars pose multiple risks without any proven benefit.16 Overall, the benefits of the use of collars remain difficult to assess and there is a need for better assessment of their risks and benefits for proper implementation.
2.5 FDA oversight on cervical collars
The FDA classifies cervical collars as class 1 medical devices. Cervical collars fall under the Physical Medicine review panel of the FDA as cervical orthosis devices and are defined as “to be intended for medical purposes to support or to immobilize fractures, strains, or sprains of the neck or trunk of the body.17” Class 1 medical devices pose the lowest risk to patients and are under the least amount of regulatory controls by the FDA.18 Class 1 devices must still be manufactured in accordance with established quality standards to ensure their safety and effectiveness for their intended use.18 Cervical collars are also exempt from the 510 (k) notification as well as good manufacturing practices requirements which would be required of devices of higher risk classes.18 Overall, cervical collars as orthodontic devices are considered low-risk; however, manufacturers still fall under the general controls of the Food, Drug, and Cosmetic Act which requires manufacturers to register their products and allows the FDA to enforce regulations on products and requires recalls if the products do not meet their intended use through post-market surveillance.19
3 METHODS
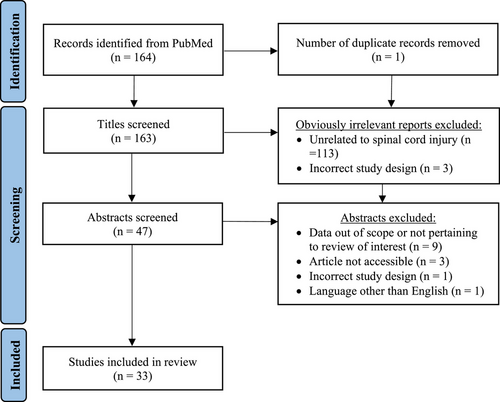
A systematic literature search was performed in March 2024 using PubMed and following the guidelines of PRISMA. Customized queries included the following keywords with AND/OR operators entered into the search engine: cervical collar, spinal immobilization, spinal cord injury, and spinal neurosurgery. The search was limited to full-text original retrospective or prospective studies, case reports, practice guidelines, meta-analyses, and systematic reviews published in English after the year 2014 and before the year 2024 to provide up-to-date information from the past 10 years. Article screening and inclusion eligibility were conducted independently by two different reviewers (SK and RM). Studies that evaluated the safety and efficacy of cervical collars used for SCI or spinal neurosurgery were included. A total of 168 articles were initially identified following this search strategy. After removing irrelevant articles based on title, a total of 85 abstracts that fit the inclusion criteria were retrieved. Abstracts were then screened, leaving 33 total articles published between 2014 and 2024 to be included in the review. The article selection process is outlined in Figure 1.
4 RESULTS
4.1 Effectiveness of current clinical guidelines
Despite guidelines for liberal cervical collar use in patients with traumatic SCI,20 the use of cervical collars in CSI management has continued to be debated due to varied patient outcomes. In cases of cervical SCI, full mobilization is recommended to sufficiently immobilize the cervical spine instead of a cervical collar alone.20 Among patients with traumatic SCI who were treated at a level I trauma centre, cervical collars were often used in patients with cervical SCI, suggesting inappropriate use of cervical collars.20 Potential reasons for failure to use full spinal immobilization may include it being a more time-consuming option, especially if the patient is in an unstable condition; however, this was not found to be the case in all 12 patients who failed to receive full spinal immobilization.20 Thus, in cases of cervical SCI, cervical collar use must be closely monitored and reduced in order to reduce the risk of further injury from improper immobilization of the cervical spine.
In patients with blunt trauma, cervical spinal motion restriction was found to have high sensitivity (90.9%) and low specificity (17.4%) in the identification of CSI.21 Patients who did not receive spinal immobilization but who did have CSI had no neurologic compromise when managed without intervention.21 In general, conservative treatment using cervical collars or halo vests is still the preferred option in stable and/or minimally displaced CSI.22
Penetrating CSI often involves major vascular and airway injury and requires advanced airway protection.16 Cervical collar use in penetrating traumatic SCI has been implicated in serious neurological complications,16, 23 increased morbidity,16, 23 and higher mortality.16, 23-25 One proposed reason is that cervical spinal immobilization masks important clinical signs in penetrating trauma like tracheal deviation or absent carotid pulse and interferes with successful endotracheal intubation.16 As a result of these findings, several national emergency medicine and trauma surgery groups, including the Prehospital Trauma Life Support Executive Committee, ACS-CT, ACEP, NAEMSP, and Eastern Association for the Surgery or Trauma currently recommend against routine use of spinal immobilization for penetrating traumas in adult patients.16 A qualitative study with pre-hospital care providers revealed that existing spinal immobilization practices are being questioned, and many providers currently tailor guidelines to meet specific patient needs.26 Many discrepancies exist with the way guidelines are executed, with one study attributing 93% of clinical negligence cases of patient neurological deterioration to a failure to perform spinal immobilization or inappropriate removal of spinal immobilization.27 With limited evidence to support current cervical collar use practices and recent findings of harm from overuse, providers supported a pragmatic and individualized approach for high-quality, patient-centred care.26 Overall, unnecessary cervical collar use in traumatic SCI has decreased,28, 29 but collars continue to be inappropriately used in patients who do not need them and underused in those who would benefit from them.29
4.2 Potential benefits as a cost-effective alternative
In a study done in a low-resource hospital in Nigeria, patients with underlying degenerative disease with traumatic cervical SCI without evidence of spinal instability or neurological deterioration showed improved neurological outcomes with the use of hard cervical collar immobilization.30 Frankel grades were used to measure spinal stability status, finding that over 85% of patients with both grade B and grade C Frankel grades had an improved grade upon discharge.30 Furthermore, all patients demonstrated satisfactory spinal stability after conservative treatment with the hard cervical collar.30 Given the improvements shown in patients with underlying degenerative disease with traumatic cervical SCI, nonoperative management should be considered as a viable option. Cervical collars have the potential to provide adequate care in resource-limited settings, especially given their relative cost-effectiveness and accessibility.30
4.3 Impact on restricting movement
In healthy volunteers using cervical collars during vehicle and subsequent self-extrication, collar use resulted in decreased maximal movement, a valuable surrogate measure for the risk of secondary SCI.31 Maximal movements were found to be significantly decreased when a collar was used, while smaller movements still occurred resulting in comparable cumulative movement.31 Although rescue services and medical providers operate with the rationale that smaller movements pose less risk for secondary spinal injury than larger movements, the effect of cumulative movement on SCI risk remains unknown. Another study found that there was a significantly increased average movement of the cervical spine with cervical collar use during self-extrication than without.32 Cadaver studies also demonstrated significantly increased three-dimensional movement after the application of a cervical collar.33 This can lead to dural sac compression and SCI in cases of unstable craniocervical junction.33 Mixed evidence regarding cervical spine movement and subsequent risk for SCI demonstrates that it may be safer for hemodynamically stable patients to perform controlled self-extrication without a cervical collar or other traditional prehospital rescue equipment.32
4.4 Injury prevention in patients with existing spinal instability
Cervical collars have been widely used to prevent further injury, especially in patients with conditions predisposing them to SCI. For example, AS patients have an eleven-fold greater risk of SCI, and spinal injury often contributes to increased mortality due to exacerbated neurological deficits.34 One patient with AS experienced paraplegia attributed to the use of a rigid backboard for spinal immobilization.34 This rigid backboard increases the risk of unstable fracture and neurological dysfunction by forcing an already kyphotic spine into an unnatural alignment.34 Hard cervical collars have been implicated in causing life-threatening SCI, such as posttraumatic C5 palsy experienced by one AS patient after hard collar application.35 Instead, a vacuum splint device with a cervical collar was found to be a more effective and safe alternative than a rigid background with or without a cervical collar for spinal immobilization in AS patients.34 Cervical collars that support the original spinal curvature of AS patients show promise in providing cervical spinal stability without creating further injury.34, 35 Furthermore, given significant spinal movements shown in studies with cadavers being transferred to and from backboards, AS and other patients who are ambulatory should self-transport themselves with a cervical collar if this can be done without pain.34
4.5 Post-surgical recovery and injury prevention
Cervical collars are often used after surgery to prevent injury and aid in recovery; yet, the effectiveness of this remains controversial. Cervical collars are a popular option post-laminoplasty, to protect hinge-opening and reduce the risk of hinge fractures and spring-back phenomena.36 However, Philadelphia collar use for 2 weeks after cervical laminoplasty was not found to change cervical pain up to 1 year after surgery, cervical range of motion, lordotic angle, or complications.37 Another study similarly found that although rigid cervical collar use after single-door laminoplasty reduced axial neck pain in the first two weeks after surgery, it did not have a significant impact on range of motion, quality of life, or complications upon subsequent follow-up.36
Axial symptom is a specific complication after laminoplasty that causes pain and/or stiffness in the posterior neck, along with a poorer quality of life.38 Postoperative axial symptoms were associated with postoperative results of spinal surgery.38 Cervical collar use after laminoplasty was implicated in 34.9% prevalence of axial symptoms.38 Risk factors for higher incidence of axial symptoms with cervical collar use after laminoplasty included longer collar wear time and larger preoperative and postoperative C2 sagittal vertical axis.38
In a qualitative study with adult blunt trauma victims who had cervical collar placement for potential SCI, 38% of patients reported discomfort from immobilization, mainly from point pressure at the posterior head and hip.39 24% of the patients experienced pain related to immobilization.39 Given these patient perspectives and clinical data regarding cervical collar complications, collar wear time should be appropriately assessed to maximize recovery and minimize discomfort and pain during post-surgery recovery in SCI patients. Early collar clearance after criteria validation is recommended, as it helps reduce costs and limit immobilization-related morbidities.5, 40, 41 Overall collar use should be evaluated for necessity relative to individual patient risk factors and removed appropriately if complications arise.
4.6 Pain with collar use
Despite their demonstrated benefits in SCI management, cervical collars commonly increase pain and discomfort through the development of pressure ulcers.42, 43 Hospital-acquired pressure ulcers are often not reimbursed by health insurance and impose an estimated annual cost of $4 million in the United States.44 They can require extensive reconstruction if severe and can cause tissue ischemia and death via constant pressure, especially in the occipital area.44 In adult trauma patients with an extrication collar, over 75% of patients developed a category 1 pressure ulcer.42 Although category 1 pressure ulcers are reversible, it is a marker of increased risk for severe pressure ulcer development with continued use of the collar.42 Moreover, approximately 65% of the patients developed indentation marks, with 28% having severe indentation marks.42 Over 60% of patients experienced pain, and 38.5% experienced severe pain.42 Female patients were found to experience significantly more pain than their male counterparts.42 The high rates of pressure ulcers and indentation marks indicate a significantly higher risk of developing pressure ulcers and pain with prolonged use of cervical collars in trauma patients.42 In addition to prolonged collar use, predictive factors for cervical collar-related pressure injuries include intensive care unit hospitalization, low level of consciousness, longer hospital stay, older age, underlying cardiovascular or respiratory disease, and need for mechanical ventilation.43 These markers should be closely studied when managing traumatic SCI to avoid inappropriate cervical collar use that may exacerbate pain. In another study evaluating the Philadelphia and Stifneck cervical collars in healthy adults, a high occurrence of indentation marks and a significant increase in skin temperature was observed.45 These two markers have been implicated in the development of collar-related pressure ulcers,45 illustrating the need for improvements in collar design and comfort for trauma patients. The occiput was mainly implicated in pressure ulcer formation due to a significantly higher device-skin interface pressure, especially for the Stifneck extrication collar.7 The Stifneck collar was implicated in higher movement restriction overall.7 The Stifneck and Philadelphia collars both had significantly higher humidity at the device-skin interface, which corresponded to the closed-cell foam padding of these designs.7 Both occipital pressure7, 44 and skin humidity7 were associated with higher collar discomfort and risk of pressure ulcer formation, especially for Stifneck® extrication collars.7 Lined open-cell foams may provide a potential for reducing this risk7 in SCI patients using cervical collars.
In addition to pressure ulcers, hard cervical collars may increase the risk of head injury through elevated ICP from impaired venous return.5 Cervical collar use in the elderly has been associated with an increased risk of dysphagia, dyspnea, delirium, mobility, compliance issues, and function outcomes.46 When comparing soft and rigid collars, rigid collars provided significantly higher stability in flexion, extension, and rotation movements; however, there were no significant differences in secondary SCIs between soft and rigid collars.47 Given the increased risk of complications with hard cervical collars, soft foam collars may mitigate these issues while providing adequate injury protection. In a study with trauma patients with potential CSI, the use of soft foam cervical collars did not increase the risk for secondary SCI when compared with rigid collars.48 Further investigation into potential alternatives like soft collars is needed to reduce pressure ulcers and related complications from cervical collar use.
Pediatric patients with SCI are currently underserved in their access to cervical collars.49 In a national study of pediatric trauma encounters in the United States, 83% of pediatric patients with cervical spine fractures did not have a prehospital cervical collar placed.49 Lack of pediatric-sized equipment plays a role in the underuse of cervical collars in pediatric patients with potential SCI,49 necessitating the development of a clinical decision tool to guide cervical collar placement in pediatric patients with SCI or at risk of developing SCI.
5 CONCLUSIONS AND FUTURE RESEARCH
The controversy surrounding the effectiveness of cervical collars for spinal cord injury prevention and management highlights the need for further research in the area. As seen in the literature, spinal immobilization has high sensitivity and low specificity in detecting SCI.21 There is documented evidence of additional harms caused by cervical collar use in certain patient cases, such as penetrating SCI6, 23-25 and AS.34, 35 Proactive identification of risk factors before cervical collar use can reduce additional injuries and the risk of further spinal injury. Ultimately, with the absence of clear guidelines and lack of robust evidence, healthcare professionals are faced with making highly personal decisions that are not rooted in fact, yielding significant variability and impacting the quality of care. Thus, additional studies are imperative in examining the efficacy and safety of cervical collars for spinal cord injury management.
AUTHOR CONTRIBUTIONS
Conceptualization: Shruti Kolli, Robert Medina, Chloe DeYoung, and Brandon Lucke-Wold; writing–original draft: Shruti Kolli, Robert Medina, Chloe DeYoung, and Brandon Lucke-Wold; writing–review & editing: Shruti Kolli, Robert Medina, Chloe DeYoung, and Brandon Lucke-Wold. All authors have read and agreed to the published version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICAL APPROVAL
Not applicable.