Coincidence or association: Adult-onset Still's disease following HPV vaccine
Key Clinical Message
This case details adult-onset Still's disease (AOSD) onset post-human papillomavirus (HPV) vaccination and acute gastroenteritis. The timing of HPV vaccine and vaccine-autoimmune disease literature may potentially confound the well-established link between infections and AOSD onset.
1 INTRODUCTION
Adult-onset Still's disease (AOSD) is a systemic autoinflammatory disease that classically presents with daily fevers, salmon-pink maculopapular rash typically found on the trunk or upper extremities, and migrating polyarthritis.1 Pertinent laboratory values that are commonly elevated in AOSD patients include ferritin, erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), and white blood cell (WBC) count; however, being a diagnosis of exclusion, negative rheumatoid factor (RF), antinuclear antibodies (ANA), and anti-citrullinated protein antibody (ACPA) may also help in diagnosing this disease. The etiology remains unclear, but it has been suggested that both genetic predispositions and infectious triggers may be contributing factors. Current literature indicates a connection between various infectious agents and the onset of AOSD including rubella, Epstein–Barr virus (EBV), cytomegalovirus, and human papillomavirus (HPV).2-4 Although a rare phenomenon, there are multiple case reports in the literature of AOSD developing after various vaccinations including the influenza and COVID-19 vaccines.5-9 Furthermore, there are reports of the onset of various autoimmune diseases after the administration of the HPV vaccine.10, 11 However, there are no current reports in the literature demonstrating the onset of AOSD after the HPV vaccine specifically. Here, we present the case of a 20-year-old male who presented with malaise, fevers, headache, and joint pain after receiving the third dose of the HPV vaccine and was diagnosed with AOSD after an extensive workup.
2 CASE HISTORY
A 20-year-old male with no significant medical history presented to the emergency department for 2 days of fever, malaise, headaches, dark-colored urine, and vomiting. Of note, the patient received his third dose of the HPV vaccine the day prior to the onset of symptoms and had an episode of self-limiting diarrhea approximately 2 weeks prior. Initial labs were significant for WBC 22.7 K/μL, AST 107 IU/L, ALT 145 IU/L, Alk Phos 193 IU/L, total bilirubin 7.9 mg/dL, CRP 17 mg/dL, ESR 106 mm/h, haptoglobin 341.9 mg/dL, ferritin 885 ng/mL, and aldolase 18.7 U/L. His urinalysis also demonstrated significant proteinuria and large amounts of bilirubin, which in combination with dehydration, explained the dark-colored urine. Initial imaging via abdominal ultrasound was significant for splenomegaly but otherwise unremarkable. Ancillary testing including HIV, EBV, CMV, Lyme, hepatitis serology, parvovirus, syphilis, and toxoplasmosis was negative. While in the hospital, the patient was treated with 1 day of ceftriaxone, then transitioned to empiric doxycycline. He was discharged after 2 days in the hospital with a 7-day course of doxycycline with a diagnosis of fever of unknown origin (Figure 1), likely secondary to infectious cause.
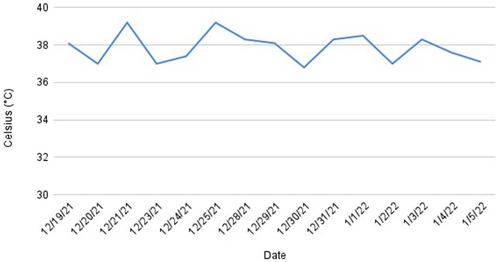
He then returned to the hospital 2 days later due to worsening liver function tests (LFTs) at his outpatient follow-up appointment and worsening of his symptoms, including recurrent fevers (Figure 1), abdominal pain, and migrating polyarthritis. The gastroenterology, infectious disease, endocrinology, and hematology teams were consulted. The patient's workup at this time was largely unremarkable including a negative infectious workup including blood cultures, COVID, EBV PCR, influenza, hepatitis, syphilis, treponema, leptospira and ehrlichia, and a negative autoimmune panel including ANA, thyroid antibodies and autoimmune hepatitis. A CT scan of the abdomen and pelvis was also performed to rule out any hepatobiliary process and was negative. An abdominal ultrasound was repeated and showed prominence of the gallbladder wall with trace pericholecystic fluid noted. Sludge was also noted in the gallbladder with the findings being equivocal for low-grade acalculous cholecystitis. Throughout the course of his stay, the patient continued to have intermittent, recurrent fevers and he developed a sore throat and salmon-pink colored rash on his chest and upper extremities. He was started on ibuprofen 800 mg. On the second day the patient's condition began to improve and his LFTs also showed mild improvement. The patient was discharged with a 5-day course of amoxicillin.
The patient presented to the ED again 3 days later with persistent fevers (Figure 1), jaundice, and severe left hip pain causing an inability to ambulate. On arrival, the patient was found to have a small joint effusion of the left hip through point of care ultrasound. Despite intermittent fevers, the patient's infectious disease workup was negative and antibiotics were discontinued based on recommendations from the infectious disease team. During this visit, the hepatology and rheumatology teams were further consulted. The patient had a magnetic resonance cholangiopancreatography done which showed hepatosplenomegaly, but no significant liver parenchymal abnormalities. However, there was some small-volume ascites and diffuse mesenteric edema. The patient also had a liver biopsy done which revealed moderate inflammation of the portal tracts and moderate centrilobular cholestasis. Other than an IL-6 of 293.3 pg/mL, serological work-up (i.e; ANA, RF, ACPA, extractable nuclear antigens, complements, antineutrophil cytoplasmic antibodies, creatine phosphokinase, autoimmune hepatitis panel, and urine protein and creatinine) was negative. The patient was diagnosed with AOSD based on the Yamaguchi Criteria: he fulfilled all four major criteria consisting of having a fever, arthralgias, typical rash, and leukocytosis along with four of the five minor criteria with a sore throat, hepatosplenomegaly, liver dysfunction, and absence of ANA and RF.12 The patient was started on Prednisone 40 mg and his symptoms improved significantly in a matter of days including resolution of his rash, decreased joint pains, and resolution of his sore throat within 1 day. He was discharged on day 3 of starting steroids (day 9 of his hospital stay) with recommendations for outpatient follow-up with a rheumatologist in 2 weeks.
At his first outpatient follow-up, the rheumatologist decreased the prednisone dosage to 30 mg and recommended a gradual reduction of 10 mg every 3 weeks. The patient maintained regular follow-ups with the rheumatologist, initially on a monthly basis, and then at intervals of 3–4 months, showing remarkable improvement in response to the steroid treatment. Notably, his LFTs also showed excellent response, with AST and ALT levels returning to normal by June. Although there was consideration of starting the patient on anakinra, it was decided to avoid its use unless another episode of AOSD flare occurs.
3 METHODS AND RESULTS
To the best of our knowledge, this is the first case reporting the development of AOSD in a patient immediately after receiving the HPV vaccine. It is suspected that infectious agents can trigger AOSD, with one case study reporting the onset of AOSD in a patient with recurrent genital HPV infection.2 Vaccines have been correlated with the onset of autoimmune disease in rare cases, but the role that vaccines play in the development of autoimmune diseases has not been established.2, 10, 13 Previous research demonstrates individuals reporting the onset of autoimmune conditions following COVID-19 vaccination,5 including idiopathic thrombocytopenic purpura,14 transverse myelitis,15 Guillain–Barre syndrome,16 and anti-neutrophil cytoplasmic antibody-associated vasculitis.17 Another case reported macrophage activation syndrome in a patient with AOSD after receiving the COVID-19 vaccine.18 Additionally, there are confirmed associations between the flu vaccine and Guillain–Barré syndrome and between the measles–mumps–rubella vaccine and thrombocytopenia.19-21 Previous studies have also shown an association between the HPV vaccine and lupus.11, 22 Most notably, there have been reports of the onset of AOSD after vaccinations.5-9 Taking these cases into consideration, it is prudent to consider if vaccinations follow the same pathway as infectious agents in triggering the onset of AOSD and other autoimmune conditions.
4 DISCUSSION
The current case is unique but relevant as it illustrates a potential relationship between vaccination and the onset of AOSD and builds on previous research examining this very association. Although the relationship between this patient's AOSD and HPV vaccine is unknown, there are some possibilities we hypothesize could explain this relationship. One likely possibility is that this overlap in timing was purely coincidental and the patient's onset of AOSD was unrelated to the vaccine he received, but rather related to the episode of gastroenteritis he had 2 weeks prior. A second less likely possibility relates to the association of AOSD with high ferritin levels.23 Elevated ferritin levels can result from viral infections, or in this case, possibly the HPV vaccine. Since AOSD is hypothesized to have a potential infectious trigger and prior studies show an association between vaccinations and autoimmune disease, perhaps the HPV vaccine could have played a role in triggering the onset of AOSD in this particular case. Although the etiology of this patient's AOSD seems to be most likely caused by an infectious agent based on his episode of viral gastroenteritis 2 weeks prior, due to the fact that the patient received a vaccine a day before the onset of symptoms, we cannot rule out an association between the vaccination and the onset of AOSD. The purpose of this case report was not to associate vaccines with AOSD but to expand our understanding of its etiology. There is no enough evidence to suggest whether the vaccine caused the reaction or triggered an underlying process, or if the timing was coincidental. However, the patient's symptoms all started after receiving the vaccine, which leads us to question whether it had any relation to his presentation.5 Previous literature suggests a correlation between infectious agents and AOSD and if a similar relationship is seen between vaccines and AOSD, it may further our understanding of underlying mechanisms. Furthermore, clinicians must be aware of these cases and take them into consideration as early diagnosis and treatment can make the difference between making a full recovery and facing long-term complications.13
AUTHOR CONTRIBUTIONS
Muhammad Ahmed: Conceptualization; data curation; formal analysis; investigation; methodology; writing – original draft; writing – review and editing. Kaab Husain: Conceptualization; investigation; writing – original draft; writing – review and editing. Arqam Husain: Conceptualization; investigation; writing – original draft; writing – review and editing. Sameer Syed: Methodology; writing – original draft; writing – review and editing. Mahfujul Z. Haque: Supervision; validation; writing – review and editing. Alireza Meysami: Supervision; writing – review and editing.
FUNDING INFORMATION
The authors did not recieve funding for this study.
CONFLICT OF INTEREST
All listed authors were enabled access to relevant data and had a role in writing the manuscript. This project received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




