Unusual case of broad ligament leiomyoma: A diagnostic and surgical challenge
Abstract
Extra-uterine leiomyoma (EUL) is extremely rare and due to its unusual location, results into diagnostic dilemma and due to its unusual location may lead to surgical complication as in this case. We present a case of large broad ligament leiomyoma in a 40-year-old premenauposal that was excised with challenges.
1 INTRODUCTION
Leiomyomas (fibroids) are common smooth muscle benign tumors that arise from the uterus. They are usually firm, well circumscribed, and localized to the pelvic cavity.1 Extrauterine leiomyomas (EULs) are rare, and their etiology is unclear.2 They usually affect premenopausal women and are described as three types; intraveinous leiomyomatosis, benign metastatisizing leiomyoma, and leiomyomatosis peritonealis disseminate.3 Other reported sites of EULs include the vulva, rectovaginal, gastrointestinal tract, and genitourinary tract.1 We describe an unusual case of broad ligament leiomyoma extending to the pouch of Douglas that was surgically removed successfully.
2 CASE PRESENTATION
2.1 Patient information
A 40-year-old female (P1L1) patient presented to our center with a gradual long-standing history of progressive abdominal distension more marked for 8 months accompanied with lower abdominal pain that was dull in nature radiating to her back and the thighs bilaterally. She also reported to experience heavy menses, feeling of heaviness in her vagina, and inter-menstrual bleeding through the course of illness. This has been associated with long standing history of inability to conceive in the last 2 years. She is a married lady with her second partner as she could not conceive with her first and does not smoke or consume alcohol. There is no family history of malignancies and she denied usage of contraception. She denied drug or food allergies. Prior to this, she is reported to have normal menses and menarchy was at 14 years of age.
She was diagnosed with polycystic kidneys 1 year ago and has been attending urology clinics regularly where her last serum creatinine and urea were within normal range with eGFR of 121 ml/min. Her past surgical history includes a caesarean section due to cord prolapsed and laparotomy was done in our center due to uterine myoma where only biopsy could be taken of the mass and confirmed uterine fibroid by histology. The surgeons could not excise the mass without performing a hysterectomy which was not consented for then and the patient opted to conceive. The ultrasound prior had concluded uterine fibroid.
2.2 Clinical findings
Upon admission, she was well nourished, alert, not pale, not jaundiced, and with no lower limb edema. Her vitals were within normal range and was saturating at 98% on room air. Her abdomen was distended but moving with respiration and not tender. She has a mass palpable in the suprapubic region extending above her umbilicus (equal to 28 weeks gestation), the mass was hard but mobile. On bimaual pelvic palpitation, the uterus was central, bulky, measuring almost 28 weeks, firm and fixed with mild tenderness on manipulation but the adnexa were free. Other systems were essentially normal. We had a provisional working diagnosis of uterine fibroid and polycystic kidneys.
2.3 Diagnostic evaluation
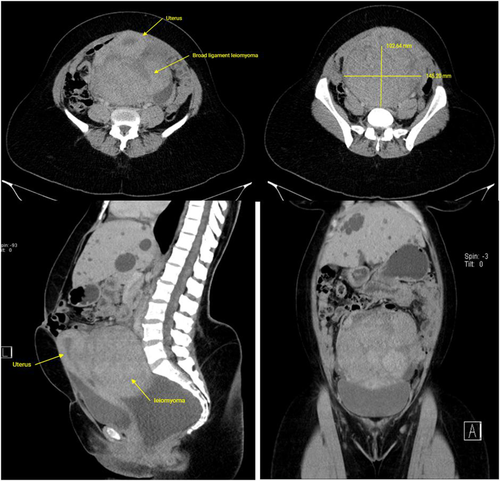
Her abdominal-pelvic ultrasound revealed bilateral hydronephrosis, multiple liver cysts, and uterine myoma measuring 13 × 9 cm from the posterior wall of the uterus. Then, an abdominal-pelvic CT-scan was done and showed polycystic kidney disease, broad ligament leiomyoma (measuring 14 × 10 cm), and mild ascites in the pelvis (Figure 1). Her complete blood count revealed leucocyte count of 3.95 × 109/L, hemoglobin of 14.1 g/dl, and platelet of 215 × 109/L. Her serum urea was 4.22 mmol/L, creatinine 59 μmol/L, ALT of 23 mmol/L, AST of 32 mmol/L, and was tested negative for Hepatitis B and C. The urology team was consulted for her polycystic kidney disease, and watchful waiting was opted as her renal functions were normal throughout.
2.4 Therapeutic intervention
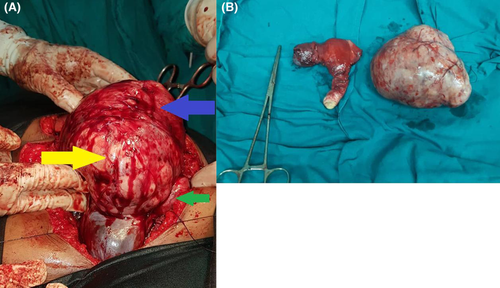
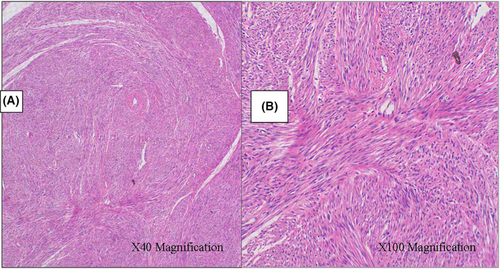
She was scheduled for an elective laparotomy after obtaining full consent (including for hysterectomy if need be) whereby intraoperatively a normal sized uterus with an huge mass of approximately 16 × 15 cm attached to its posterior wall, arising from the right broad ligament and pushing the uterus upwards and adhering to its posterior wall (Figure 2). The mass was well vascularized and the fallopian tubes, small bowel loops, and the sigmoid colon were adhered to it. The liver and kidneys were noted to be cystic. The small bowel loops were separated from the mass, however, while separating the sigmoid there was iatrogenic sigmoid injury during adhesionlysis, hence, double-barrel sigmoid colostomy was raised. Also, total hysterectomy and right salpingo-oopherectomy was done to gain access in the pouch of Douglas (in order to excise the whole of the mass) and the mass was completely excised, and histology analysis confirmed uterine fibroid (Figure 3). The abdomen was then cleaned with normal saline, hemostasis was achieved and closed. She was transfused with 2 units of whole blood intraoperatively and one unit on day-one post operatively.
2.5 Follow-up and results
She was nursed in the gynecological ward for 11 days, faired well whereby her wound healed and control hemoglobin was 10.8 g/dl, serum sodium of 134.8 mmol/L, and potassium of 4.86 mmol/L hence was discharged with oral hematenics and paracetamol and was counseled on colostomy care.
Two months later, she was reviewed at the surgical outpatient unit whereby she was clinically stable with no abdominal symptoms or signs. Her colostomy was functioning. She was scheduled for colostomy closure of which the procedure was uneventful, and she recovered well post operatively. She was reviewed 2 months later with normal renal function tests, liver enzymes within normal range, and hemoglobin of 13.7 g/dl. Urine for culture was negative and abdominal-pelvis ultrasound only showed polycystic kidney and liver.
3 DISCUSSION
Leiomyomas are histologically smooth muscle tumors and are almost always benign. They are common occurring in about 65% of women and incidentally found in 80% of all uterine specimens at hysterectomy.4 They are related to anovulation and high levels of estrogen.5 Their clinical features vary depending on their size and locations.4 Fibroids rarely occur and grow in unusual locations outside the uterus, and if so, they present with clinical and diagnostic challenges due to their nonspecific presentations hence compromise the accuracy of preoperative diagnosis.4, 6 Little is known about these extrauterine growths and often diagnosis of a leiomyoma is made after histology analysis of a resected specimen, as this was the case in the index case during her first laparotomy.
Extra-uterine leiomyoma usually present with pain and secondary complications from their compression effects as a result of their location, as this was evident in our case due to the location being in the pouch of Douglas.4 Uterine leiyomayomas depending on their size and site can cause menstrual disturbances, pressure symptoms such as bladder or bowel dysfunction, infertility, or even recurrent pregnancy loss. The most common extra uterine site is broad ligament with an incidence of <1% and other rare locations are round ligament, ovarian ligament, and ovaries.7 There are two types of broad ligament fibroids; false broad ligament fibroid that grow into the broad ligament from the uterus, and true broad ligament fibroid that arise from sub-peritoneal connective tissue of the ligament.5 In our case, this was a true broad ligament leiomyoma.
Extra-uterine leiomyoma can be among the differential diagnosis of uterine leiomyoma along with other being broad ligament fibroid, solid ovarian mass, pedanculated subserosal fibroid or lymphadenopathy. Clinicians should have a high suspicion of index of EUL as some diagnostic modalities can miss this.8 In a case report by Dulewad et al, the authors presented a case of EUL mistaken as pregnancy. Jha et al also state in their report that it can be difficult to make diagnosis using ultrasonography especially when the fibroid is big and displaces adjacent structures away.9, 10 Diagnostic options include imaging modalities such as ultrasonography, computed tomography (CT), or magnetic resonance imaging (MRI), whereby MRI has the highest sensitivity and can describe secondary changes like degenerations, calcifications, or necrosis. This can also assist in planning out the surgery. However, the final diagnosis is made by histology.5 As learnt from this case, higher modality of radiologic investigations is needed to make a preliminary diagnosis and can assist surgeons to plan out the surgery therefore appropriate consent can be sought from the patient highlighting the possible complications before the procedure. A multidisciplinary approach is also vital in planning for the management of such challenging cases.
Surgery is the mainstay for the management of symptomatic leiomyomas. Due to the size and location, sometimes surgery is challenging due to the proximity of nearby pelvic and abdominal structures as reported in the index case whereby hysterectomy had to be done in order to remove the whole fibroid and the sigmoid was injured in doing so. This is also reported by El-Agwany et al in their report that surrounding organs may be at risk especially the ureters.11, 12 Laparoscopic surgery can be an option, but surgeons should note that the fibroid can be much larger than the initial appearance because the pelvis and retroperitoneal space can accommodate as a reservoir and needs careful hemostasis during dissection as can be very vascularized and in close relations to nearby vital structures (ureters, internal iliacs, and nerves).6
Uterine artery embolization may have little or no effect because the mass may not rely on the uterus for its blood supply which is why it is located outside the uterus. If the setting allows and surgeon's experience, robot-assisted laparoscopic myomectomy (RALM) can be an option where advantage includes less fatigue for the operating surgeon.6
4 CONCLUSION
Broad ligament fibroids are unusual pelvic tumors that can cause difficulties in diagnosis as they mimic malignant tumors and surgical management due to their locations and sizes. Clinicians should think of extra-uterine leiomyomas as a differential diagnosis of adnexial masses. Management can be by surgery but can pose complications; hence, surgery expertise is required for successful outcome.
AUTHOR CONTRIBUTIONS
JL, RG, and EM conceptualized and drafted the manuscript. JT reviewed the medical records. JT, RG, and EM performed the surgery. AS reviewed and reported the radiology films and PA prepared and reported the histology slides. All authors have read and approved the final script.
ACKNOWLEDGMENTS
The authors would like to thank the patient for permission to share her medical history for educational purposes and publication.
FUNDING INFORMATION
There was no funding towards this research.
CONFLICT OF INTEREST
The authors declare they have no competing interests.
ETHICAL APPROVAL
Ethics approval was obtained from the Department of Obstetrics and gynecology, Kilimanjaro Christian Medical Centre.
CONSENT
Written informed consent was obtained from the patient for publication for this case report; additionally, accompanying images have been censored to ensure that the patient cannot be identified. A copy of the consent is available on record.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study




