Shared histological and immunohistological findings in two patients with generalized vitiligo associated with autoimmune atrophic gastritis
Abstract
The prevalence of autoimmune atrophic gastritis (AAG) in vitiligo patients was estimated at about 15%. In both conditions, a release of specific antibodies and an autoimmune destruction of target cells (melanocytes in vitiligo, parietal cells (PC) in AAG) mediated by CD8-T lymphocytes was demonstrated to perform a comparative histological study of vitiligo skin and AAG mucosa. In two patients with concomitant vitiligo and AAG, biopsies from the vitiligo lesions and gastric mucosa from corpus fundus were performed. Sections were immunostained with E-cadherin, Coll IV, CD8, CD20, CD4 antibodies. The skin sections also were stained with HES, HMB45, MITF. Common histological findings were found in both diseases. Adhesivity impairment with down expression of E-cadherin and Coll IV was objectivated. The protruding MITF+melanocytes and the detached PC were surrounded by an infiltrate including CD8 and CD4. CD8 was infiltrating the epidermis in close contact with the remaining melanocytes and the gastric glands around the remaining PC. In both diseases, the autoimmune process could be preceded by a detachment of either melanocytes in vitiligo or PC in AAG possibly in relation to an initial adhesivity impairment of these cells. Common autoimmune mechanisms could be suggested for both diseases.
1 INTRODUCTION
Vitiligo is an acquired depigmenting disorder due to melanocyte loss affecting skin and mucosal surfaces with a prevalence of about 1%. Different theories regarding its pathogenesis have been put forward, autoimmunity being the most popular one. The latter is based mainly on the association of vitiligo with known autoimmune diseases and the presence of organ-specific antibodies in affected patients.1 Clinically, autoimmune atrophic gastritis (AAG) is not associated with any specific gastrointestinal signs or symptoms. In a recent study, the most common initial findings were hematological disorders (pernicious anemia in 10% to 15% of patients), followed by a positive histology for gastritis.2 In less than 10% of the patients, a clinical suspicion of AAG was provided by the concomitant presence of other autoimmune diseases. The prevalence of AAG in vitiligo patients, certainly underdiagnosed, was estimated at about 15%.3
The purpose of our study was first to perform successive biopsies of both skin and gastric mucosa samples from two patients with associated vitiligo and AAG and second to compare step by step their histological and immunohistological characters.
2 CLINICAL CASE n° 1
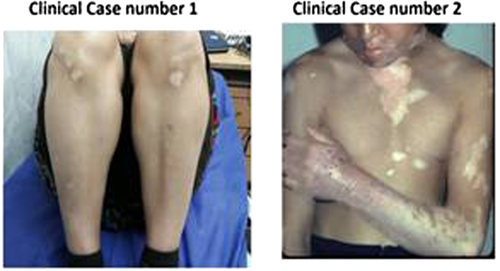
A 48-year-old woman, with AAG, was referred by gastroenterology service for the evaluation of depigmented patches on her abdomen and legs (Table 1; Figure 1). Lesions had appeared since 5 years ago.
| Vitiligo type | Autoimmune atrophic gastritis | Anti-parietal cells antibodies | Pernicious anemia detection | Hashimoto thyroiditis detection | Other diseases | |
|---|---|---|---|---|---|---|
|
Clinical case No. 1 |
NSV Abdomen lower limbs |
PC atrophy Oxyntic mucosa inflammation |
Positive | Positive | Thyroid insufficiency |
Type-1 Diabetes Breast Cancer |
|
Clinical case No. 2 |
N S V FACE, NECK, TRUNK, UPPER LIMBS |
Atrophic glandular alterations «pseudo-pyloric metaplasia» |
Positive | Positive | Positive | None |
- Abbreviations: NSV, Non-segmental vitiligo; PC, Parietal Cells.
In her past medical history, she had diabetes mellitus type I, hypothyroidism, pernicious anemia with a positive antiparietal cell antibody, and breast cancer. Mastectomy, chemotherapy, and radiotherapy had been done for her. Histological description of gastric mucosa revealed atrophy of parietal cells (PC) in fundus and inflammation restricted to the oxyntic mucosa. The disappearing glandular units were replaced by fibrotic expansion of the lamina propria with no changes in the glandular phenotype. We performed a skin biopsy from the border of the depigmented patch on her right leg.
3 CLINICAL CASE n° 2
A 35-year-old male with a generalized vitiligo involving the face, the upper limbs, associated with a thyroid insufficiency and a pernicious anemia was recruited. A gastroscopy was proposed to the patient following the recent discovery of his pernicious anemia and the positive detection of anti-PC antibodies. Helicobacter Pylori research was negative. A biopsy was performed from the edge of a vitiligo lesion including depigmented and normally pigmented areas. Skin and gastric samples were stained with HES and immunostained with anti-E-cadherin for assessment of an adhesivity defect, anti-Collagen IV for detecting an impairment of basement membrane, and CD8 antibodies for evaluating the inflammatory infiltrate. Histological description: infiltration of plasma cells and lymphocytes involving the full thickness of lamina propria with atrophic glandular alteration and in some places pseudopyloric metaplasia.5
4 COMMON HISTOLOGICAL AND IMMUNOHISTOCHEMICAL FINDINGS IN CASE 1 AND CASE 2
Several common histological findings were found both in vitiligo and in AAG (Figure 2). Melanocytes in the depigmented skin and autofluorescent PC in the gastric mucosa were partially or totally missing. At high magnification, we found MITF melanocytes protruding or falling down into the dermis, while several detached and damaged PC were staying within the lamina propria. In both conditions, an adhesivity impairment with a down expression of E-cadherin and of Coll IV was objectivated. MITF + melanocytes falling down into the dermis and the detached PC were surrounded by an infiltrate including CD8 and CD4-T lymphocytes. CD8 was infiltrating the epidermis in close contact with remaining melanocytes and around remaining P.C in gastric mucosa.

5 DISCUSSION
Melanocytes in the depigmented skin and autofluorescent PCs in the gastric mucosa were partially or totally missing. In normal conditions, melanocytes within epidermis, PC within gastric mucosa, and thyrocytes in thyroid gland are held in place through the intervention of adhesion molecules such as E-cadherin or integrins. In vitiligo, a defect of E-cadherin was reported to induce an impairment of cell adhesivity leading to a melanocyte detachment.4, 5 Therefore, in both diseases the autoimmune process could be preceded by a cell adhesivity impairment leading to a detachment of either melanocytes in vitiligo or PC in AAG. Generalized vitiligo involves genetic susceptibility loci shared with other auto-immune diseases. AAG may coexist with polyglandular autoimmune (PGA), in 10% to 15% syndrome type 1 (including hypo-parathyroidism, Addison's disease, diabetes mellitus, and mucocutaneous candidiasis) and in 15% of PGA type 3 patients (with diabetes mellitus and autoimmune thyroid diseases).6 AAG and vitiligo have been associated with thyroiditis since the early 1960. Thyrogastric autoimmune syndrome describes the presence of thyroid antibodies, autoimmune thyroid disease and autoimmune atrophic gastritis.7 In <10% of the vitiligo patients, a clinical suspicion of AAG was provided by the concomitant presence of other autoimmune diseases. The prevalence of AAG in vitiligo patients, certainly underdiagnosed, was estimated at about 15%.
6 CONCLUSION
A common autoimmune mechanism is suggested for pathogenesis of both diseases. A gastroscopy check-up should be performed in vitiligo patients with a positive detection of antiparietal cell antibodies or evocative symptoms.
AUTHOR CONTRIBUTIONS
Fariba Ghalamkarpour: Clinical study, histopathological study, writing and correction of the article. M Cario Andre: Histo- and immunopathological studies. Yvon Gauthier: Clinical study, histopathological study, writing the article.
ACKNOWLEDGMENT
None.
CONFLICT OF INTEREST
The authors have no conflict of interest to disclose. Contents of the manuscript have not been previously published and are not currently submitted elsewhere.
CONSENT
Written informed consent was obtained from the patients to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Our data are available.




