Xanthogranulomatous hypophysitis: A rare presentation in a young female patient
Abstract
Hypophysitis is a rare inflammatory condition that may present both clinically and radiologically as a neoplastic lesion. Xanthogranulomas are rare intracranial lesions with controversial etiology. Here, we report a clinical case of histologically confirmed xanthogranulomatosis hypophysitis in a young female with type I diabetes mellitus and hypothyroidism.
1 INTRODUCTION
Hypophysitis is an uncommon inflammatory disease that may manifest both clinically and radiologically as a neoplastic lesion. Clinically, it is accompanied by headaches and visual disorder because of the local mass effect and compression of the optic chiasm. Pituitary dysfunction due to inflammatory infiltration is common.1
The clinical manifestation has a wide spectrum from asymptomatic to a fatal condition often as a result of electrolyte abnormalities because of glucocorticoid deficiency in the setting of adrenal crisis from central adrenal insufficiency. Milder forms of hypophysitis are treated with replacement of deficient hormones while more acute presentations with mass effects require glucocorticoid therapy, immunosuppressive therapy, or surgery. Timely diagnosis and interventions are keys to prevention of the lethal complications of this disease.2
Hypophysitis is histologically categorized into the following five distinct categories: lymphocytic, granulomatous, xanthomatous, necrotizing, and xanthogranulomatous hypophysitis (XGH), with the latter being a mixture of the xanthomatous and granulomatous subtypes. They are also classified as either adenohypophysitis or infundibuloneurohypophysitis based on their anatomical location and areas of infiltration.3 The pathogenesis of hypophysitis is unclear. Etiologically speaking, the primary hypophysitis is autoimmune in origin and can occur in isolation or as a part of systemic diseases such as Hashimoto's thyroiditis (HT), type 1 diabetes, polyglandular autoimmune syndromes, or IgG4 systemic disease.4, 5 Secondary hypophysitis is believed to occur as a consequence of local inflammation caused by lesions including craniopharyngioma/Rathke's cleft cyst or as a part of systemic diseases such as tuberculosis, sarcoidosis, Wegener's granulomatosis, or syphilis.6 Lymphocytic hypophysitis is the most common type, while XGH is rare.1, 7 XGH is characterized by cholesterol clefts, hemosiderin deposits, multinucleated giant cells, macrophage accumulation, and fibrous proliferation in pathology examinations.7 Here, we report a young girl with type I diabetes, presented with headache and occasional hypoglycemic episodes who was finally diagnosed with XGH after surgery.
1.1 Case presentation
An 18-year-old female presented with a longstanding headache and frequent episodes of hypoglycemic events to the clinical department. She had a history of type I diabetes since 2 years of age and was receiving insulin. Despite a constant dose of insulin, she had tight blood sugar control and hypoglycemic episodes, recently. Moreover, she had hypothyroidism (HT) since 3 years ago and was under treatment with levothyroxine (50 μg/day). She had experienced recurrent episodes of hypoglycemia with frontal and retro-orbital headaches and nausea and vomiting during the last year. She had experienced menstruation only once, which was a year ago. She had a short stature in physical examination. No history of other medication was stated. Neurologic and other examinations were normal. In laboratory outpatient investigation, basal cortisol, growth hormone, insulin-like growth factor-I, luteinizing hormone, Follicle-stimulating hormone, and estradiol levels were low (Table 1). ACTH test to assess the function of the hypothalamic–pituitary–adrenal axis showed no change in cortisol level. Also, stimulation test for growth hormone showed no increase. Prolactin base level was 35 ng/ml (Normal Level: up to 20). After 0.01% dilution, the serum prolactin level did not change significantly. Erythrocyte sedimentation rate (ESR) and C-reactive protein were normal. Chest X-ray was normal, and the uterus had normal size in ultrasonography with a normal echo of the myometrium with a 3 mm endometrial line. Some peripheral follicles were seen in the left ovary. According to the history of vomiting and occasional headaches, magnetic resonance imaging (MRI) was performed (Figure 1).
| Parameter | ESR, mm/h | CRP, mg/l | TSH, miU/l | Free T4, ng/dl | PRL, ng/ml | Morning cortisol, μ/dl | ACTH, Pg/ml | GH, ng/ml | IGF-1, ng/ml | FSH, mIU/ml | LH, mIU/ml | E2, pg/ml |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Result | 7 | 2 | 0.2 | 1 | 35 | 4.2 | 7.8 | 1.65 | 70 | 1.1 | 1.4 | 20 |
| Normal value | Up to15 | 1–3 | 0.5–4.5 | 0.7–2.1 | 0–20 | 5–22 | 6–50 | 0–5 | 115–345 | 1.8–11.2 | 2–9 | 27–161 |
- Abbreviations: ACTH, adrenocorticotropic hormone; crp, C-reactive protein; E2, estradiol; Esr, erythrocyte sedimentation rate; FSH, follicle-stimulating hormone; GH, growth hormone; IGF-1, insulin-like growth factor-1; LH, luteinizing hormone; PRL, prolactin; T4, thyronine; TSH, thyroid-stimulating hormone.
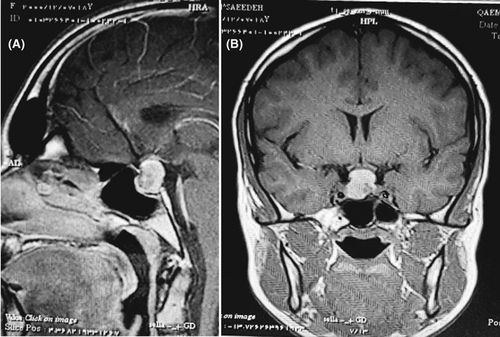
Hyperintense sellar and suprasellar mass with small non-enhancing foci in left side in T1 post-contrast image can be seen in Figure 1. Suprasellar extension of mass has pushed the optic chiasma upward. Cystic changes are seen.
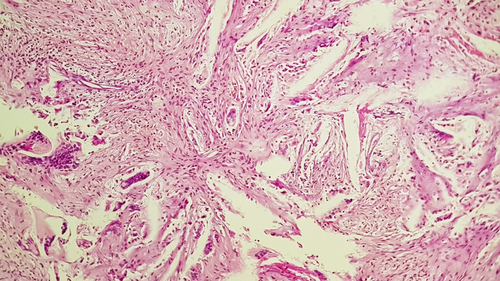
Due to mass effect of presumed macroadenoma and hypopituitarism, the patient underwent endoscopic trans-nasal trans-sphenoidal surgery, and avascular caseous-like white/yellow tissue was removed. Histopathologic examination and hematoxylin–eosin staining showed numerous cholesterol clefts surrounded by multinucleated giant cells, mononuclear inflammation, and fibrosis suggests the diagnosis of XGH (Figure 2). No evidence of vasculitis or well-formed granuloma formation was seen. Polymerase chain reaction for mycobacterium tuberculosis was negative.
The patient was treated with corticosteroids postoperatively. Also, desmopressin spray was started due to polyuria from diabetes insipidus (DI). Levothyroxine dosage did not change due to the normal free thyroid hormone after surgery. Six months later, no significant residual lesions were seen in MRI. Patient's blood sugar was acceptably in control. Menstruation occurred with estrogen and progesterone replacement therapy.
2 DISCUSSION
Combination of autoimmunity, hypopituitarism, and a sellar mass may represent autoimmune hypophysitis, which can mimic a pituitary adenoma. Our case was a type I diabetes mellitus patient presented with headache and recurrent hypoglycemia. Laboratory tests showed a central hypogonadism and hypocortisolism, a mild hyperprolactinemia, and a normal ESR and CRP. A sellar mass with cystic changes that pushed the optic chiasma upward was seen in MRI. Postoperative histopathology confirmed XGH. Corticosteroid therapy and pituitary hormone replacement resulted in patient recovery.
Hypophysitis is an uncommon etiology of pituitary mass lesions.1 The clinical presentation of hypophysitis is variable and is mainly due to inflammatory irritation of sellar and parasellar structures.8 The clinical manifestation can be seen in four categories of symptoms including sellar compression, hypopituitarism, DI, and hyperprolactinemia.
Sellar compression results in headache, nausea, vomiting, and visual field loss. Endocrine dysfunction is also common due to partial or complete deficit of the anterior pituitary hormones, mainly adrenocorticotropic hormone followed by TSH, gonadotropins, and prolactin. One-third of patients can have DI due to deficiency of the posterior pituitary hormones.1
Xanthomatous hypophysitis (XH) is a rare subtype. XH was first reported in 1998. In literature, very few number of XH cases have been reported so far. XH has been shown to have a predilection for young women.1, 9
Xanthoma cells (lipid-containing cells) are uncommonly seen in hypophyseal lesions. It can be seen in both primary and secondary hypophysitis. In primary conditions, XH, XGH, and xanthogranuloma of the sellar region all represent a continuous spectrum of the same disease process.9 The histological features of XH consist of foamy histiocytic infiltration of the adenohypophysis, small lymphocytes, and cyst-like areas of liquefaction. However, there should not be true cyst formation, granulomas, or adenoma. Fibrosis and hemosiderin pigments were later added as additional features of XH.9 The foamy cells are histiocytes and are positive for CD68 and negative for CD1a and S100. In our case, histopathology revealed foamy histiocytes in sheets, numerous multinucleated giant cells around cholesterol clefts, fibrosis, and lymphoplasmacytic infiltrate.
Xanthogranulomatous inflammation (also known as cholesterol granuloma) is commonly known in extra-pituitary sites like the middle ear, mastoid, paranasal sinuses, and choroid plexus. They have also been reported in association with adamantinomatous craniopharyngioma, and they represent tissue reaction to hemorrhage and degeneration.9 Lymphocytic adenohypophysitis is commonly seen in females in their third and fourth decade of life often in late pregnancy or postpartum period. In contrast to lymphocytic hypophysitis, XH in association with other autoimmune diseases is rarely reported in the literature. Only two cases are documented. One was associated with ulcerative colitis and the other with HT10 which was in line with our case (history of diabetes mellitus type I and HT). The presence of lymphoplasmacytic infiltrate in the histopathology and response to steroid therapy can support the autoimmune nature of XH.
Histology is the only way to diagnose XGH; hence, the first intervention in almost all cases will be surgical biopsy or resection. In case of surgical resection, no other treatment will probably be needed, while, other modalities such as steroids, methotrexate, azathioprine, and radiotherapy can be considered if there is residual or recurrent hypophysitis. Moreover, there is the risk of iatrogenic damage and resultant deterioration in pituitary function, necessitating hormonal replacement therapy, and adequate control of new-onset DI.11, 12 Postsurgically, our case was treated only with physiologic dose of hydrocortisone. It is recommended in previous studies to observe with a close follow-up schedule in patients with newly diagnosed primary hypophysitis without severe symptoms due to a space-occupying lesion. Surgery is indicated for clarifying the differential diagnosis and for acute relief of local symptoms. However, it remains controversial whether surgery is able to halt the natural progression of primary hypophysitis.13
Xanthomatous hypophysitis has got overall good prognosis if treated promptly through transsphenoidal resection of the mass. However, due to limited data, the real prognosis of this rare disease is still unclear.12 The resumption of the normal endocrine function however may be delayed or permanently lost in some cases.
3 CONCLUSION
In conclusion, XGH may clinically and radiologically mimic a pituitary adenoma. Accurate diagnosis by being aware of this entity and postsurgical steroid therapy may assist in preserving pituitary function in some cases.
AUTHOR CONTRIBUTIONS
Dr. Mohammad Ali Yaghoubi and Samira Zabihyan managed patients and wrote the first draft of the manuscript and Dr. Amin Saeidinia, Dr. Masoumeh Gharib, and Dr. Ramin Ghiyasi Moghaddam collected patients' data and wrote the final version. All authors read and approved final version.
ACKNOWLEDGMENT
Nothing.
CONFLICT OF INTEREST
The authors declare no conflict of interest regarding this manuscript.
CONSENT
The authors have confirmed that patients' consent has been signed and collected in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




