Mitral valve plasty in a patient with multiple cerebral cavernous malformations: A case report
Abstract
Cerebral cavernous malformations (CCMs) are blood vessel malformations, often untreated if asymptomatic. However, upon cardiac surgery with cardiopulmonary bypass, cerebral edema/hemorrhage may occur. We successful performed mitral valve plasty for a case of severe mitral regurgitation with multiple CCMs. Preoperative head magnetic resonance imaging and strict perioperative management are important.
1 INTRODUCTION
Few reports have described cardiac surgery using cardiopulmonary bypass (CPB) in patients with brain tumors. When CPB is performed in patients with brain tumors, there may be an increased risk of cerebral hemorrhage, infarction, and edema.1-8 In the present case report, we performed mitral valve plasty (MVP) in a patient with mitral regurgitation (MR) complicated by multiple cerebral cavernous malformations (CCMs). With strict perioperative management, the patient had good outcomes.
2 CASE REPORT
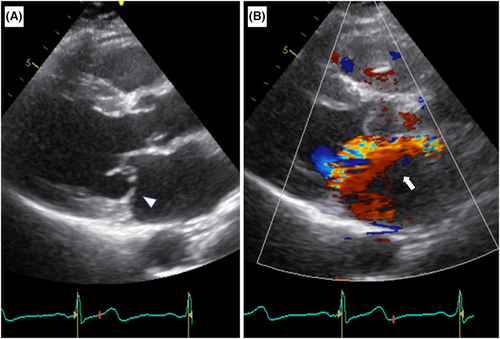
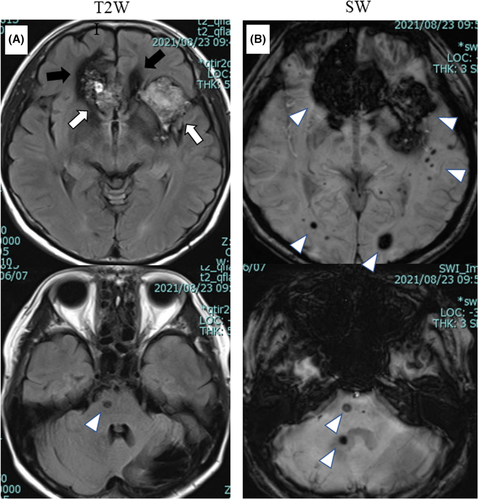
A 54-year-old woman presented to our hospital with shortness of breath upon exertion. Her New York Heart Association (NYHA) classification was class 3. She had a history of multiple CCMs and had undergone surgical resection of CCM on the left cerebellum at 16 years of age due to intratumoral hemorrhage. Physical examination at the time of her initial visit revealed no neurological abnormalities. Transthoracic echocardiography (TTE) revealed severe MR due to the posterior leaflet prolapse (Figure 1) (color Doppler area ratio, 0.41; vena contracta widths, 7.0 mm; regurgitant volume, 57.9 ml; regurgitant fraction, 0.63; and effective regurgitant orifice area of MR, 0.46). Left ventricular (LV) contractility was normal (LV diastolic diameter, 56 mm; LV systolic diameter, 33 mm; and LV ejection fraction, 0.71). Coronary angiography confirmed the absence of stenotic lesions in the coronary arteries. Intracardiac pressure measurements revealed a mean pulmonary artery pressure of 28 mmHg, pulmonary artery wedge pressure (PAWP) of 19 mmHg, v wave in PAWP of 31 mmHg, cardiac index of 2.28 L/min m2, and LV end-diastolic pressure of 25 mmHg. Magnetic resonance imaging (MRI) of the head revealed multiple CCMs and microbleeding lesions (Figure 2). Since our patient had symptomatic severe primary MR, the American College of Cardiology/American Heart Association (ACC/AHA) guideline recommended a class I indication for MVP.9
Because the patient had multiple CCMs, there was a risk of perioperative cranial neurological complications during cardiac surgery with CPB. In this regard, risk factors for hemorrhagic complications in CCM included a history of hemorrhage, presence of focal neuropathy, site of origin (infratentorial, brainstem), and female sex.10 Our patient had all of these factors, except for focal neuropathy, and was at a high risk for hemorrhagic complications. Therefore, percutaneous Mitraclip without the use of CPB represented a viable treatment option. After a thorough discussion at a multidisciplinary heart team conference, cardiac surgery was decided as appropriate, considering the patient's age and long-term outcome.
Surgery was performed under general anesthesia through a median sternal incision. Intraoperative CPB management has been performed according to the guidelines.11 In this case, in addition to the standard CPB management from the guidelines, strict management was required, particularly because of the risk of cerebral hemorrhage, cerebral infarction, and cerebral edema. The measures we strictly adhered to were as follows. To prevent plasma osmolality reduction due to excessive hemodilution at the start of CPB, CPB was primed with 280 ml of red blood cells, 240 ml of fresh frozen plasma, 268 ml of 20% mannitol, 40 ml of 8.4% sodium bicarbonate, 5 ml of heparin, and 500 mg of methylprednisolone sodium succinate. After systemic heparinization, dexamethasone (4 mg) was administered intravenously. CPB was established by ascending aortic cannulation and bicaval drainage, and the patient's deep body temperature was cooled to 30°C. The PaCO2 levels were strictly regulated to 30–40 mmHg by adjusting the ventilator and CPB. Activated coagulation time (ACT) was measured every 30 min to avoid excessive prolongation. The intrapoerative target range of ACT was 400–450 s. As a result, ACT was managed between 473 and 592 s during the use of CPB. The intraoperative mean blood pressure (mBP) was controlled at 60–80 mmHg. Since hyponatremia associated with the use of CPB decreases plasma osmolality and might cause cerebral edema,12 the target range of serum sodium concentration was 130–140 mmol/L, and the actual serum sodium levels were controlled within a range of 137–139 mmol/L. Observation of the mitral valve via a transseptal approach revealed that the posterior leaflet (P2) had prolapsed significantly because of tendon rupture. The prolapsed leaflet was resected and sutured in a triangular manner. The MVP was completed by suturing a semi-rigid full-ring to the mitral valve annulus. CPB weaning was uneventful, and dexamethasone (4 mg) was administered intravenously. Postoperatively, the patient was managed with an mBP of 60–80 mmHg by continuous infusion of nitroglycerin and carperitide, and from the second postoperative day with oral enalapril and carvedilol. Frequent blood examinations were performed and serum sodium levels were strictly controlled to achieve our target level. As a consequent, her postoperative serum sodium levels ranged from 132 to 142 mmol/L. Oral tolvaptan was administered for approximately 1 week postoperatively to prevent hyponatremia. Neurological complications were not observed. Postoperative TTE revealed no residual MR or abnormal LV contractility. The patient was discharged on the 14th day.
3 DISCUSSION
CCMs are vascular malformations, and common symptoms include convulsions and focal neurological symptoms due to compression of the mass with a low bleeding rate.13 Reports of cardiac surgery with CPB for patients with complicated brain tumors are limited to a small number of case series. Large studies were lacking, and data on appropriate intraoperative and perioperative management are also insufficient. There is no established information on risk stratification or prophylactic perioperative management for this patient population. Therefore, it is necessary to devise perioperative management while conducting preoperative risk assessment for each case. Accurate risk stratification through the accumulation of similar cases in the future will lead to improved outcomes. The present case showed no evidence of focal neurological deficits; however, there was a risk of cerebral edema or bleeding during and after CPB.10 Therefore, we followed the management recommended in previous reports1-8: (1) maintain a PaCO2 of <40 mmHg during surgery; (2) steroids (dexamethasone, 4 mg) should be administered before and after CPB; (3) maintain intraoperative and postoperative mBP at 60–80 mmHg; (4) maintain serum sodium concentrations at 130–140 mmol/L to stabillize serum osmolality; and (5) maintain a central venous pressure of <8–10 mmHg.
On the other hand, Aleksic et al.8 reported cardiac surgery in 16 patients with intracranial meningiomas and concluded that the presence of intracranial meningiomas was not a risk factor during cardiac surgery, as they found no cranial nerve complications related to meningiomas. The authors consulted a neurosurgeon preoperatively and used steroids if necessary. They also had a policy of maintaining moderate hypocapnia as anesthetic management, adding hypertonic saline or mannitol for cardiopulmonary priming, and maintaining sodium levels of 132–138 mmol/L. Ultimately, good outcomes were achieved posisbly because of such perioperative management. Further, it is unlikely that strict management is not necessary during cardiac surgery for patients with brain tumors.
In several case reports of cardiac surgery complicated by brain tumors, cranial nerve complications have occurred relatively late during the postoperative period. These observations indicated the importance of both intraoperative management and management during the first few days after surgery. Therefore, continuous control of blood pressure, blood sodium level, and anticoagulation therapy are necessary during hospitalization. In the present case, blood pressure was well controlled with nitroglycerin and carberytide continuous infusion while the patient was in the intensive care unit (ICU). Thereafter, enalapril and carvedilol were taken orally. Sodium levels in the blood were controlled by oral tolvaptan for several days with appropriate fluid replacement management. Kinugawa et al.14 reported that tolvaptan can be used safely in patients with normal sodium levels. In this case, the blood sodium level was well controlled at a dose of 7.5 mg/day, and no postoperative cranial nerve complications occurred.
Cerebral edema generally occurs with the use of CPB, even in the absence of brain tumors.15 This phenomenon may result from a decrease in plasma osmolality (hemodilution and increased anti-diuretic hormone levels due to CPB stress), increased permeability of the blood–brain barrier (BBB), and hemodynamic changes in the perioperative period. Capillaries in brain tumors do not have normal BBB function and are susceptible to edema around the tumor, increasing the risk of neurological complications.16
There are many cases of asymptomatic brain tumors, and it is difficult to detect the presence of brain tumors based on physical examination alone. Therefore, imaging examinations, such as head MRI, are necessary to detect brain tumors and are recommended routinely for patients scheduled for surgery using CPB. Head MRI is also effective in detecting asymptomatic cerebral infarctions or stenosis of cerebral arteries in addition to brain tumors and is considered cost-effective, because it can avoid major postoperative neurological complications.
In this case, because the presence of a brain tumor was known preoperatively, the aforementioned measures could be taken, and no major postoperative neurological complications occurred. Previous case studies have reported death or long-term rehabilitation due to neurological complications when brain tumors were not detected before surgery using CPB or when adequate measures were not taken perioperatively.1-5 In contrast, when tumors were detected preoperatively and adequate measures were taken, surgery was completed without complications.6-8 These findings suggested that intracranial evaluation before surgery using CPB and strict perioperative management are important for patients with brain tumors.
4 CONCLUSION
In this study, MVP was successfully performed in a patient with MR and multiple CCMs. Strict perioperative management is important to avoid perioperative cerebral complications.
AUTHOR CONTRIBUTIONS
Study conception: S Yamashita. Data collection: all authors. Analysis: all authors. Investigation: S Yamashita, SY, TD. Writing: S Yamashita. Critical review and revision: all authors. Final approval of the article: all authors. Accountability for all aspects of the work: all authors.
FUNDING INFORMATION
No funds, grants, or other support was received to assist with the preparation of this manuscript.
CONFLICT OF INTEREST
The authors have no conflict of interests to disclose with this study.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




