Splenogonadal fusion: A case series of two challenging diagnoses
Abstract
Splenogonadal fusion is an abnormal connection between the spleen and gonads. This rare entity can be easily confused with testicular tumors. It usually accompanies congenital malformations, such as cryptorchidism, making diagnosis more difficult. Surgeons must be aware of this entity to avoid unnecessary orchiectomy. In some cases, biopsy may help with diagnosis.
1 BACKGROUND
Splenogonadal fusion (SGF) is a rare congenital abnormal connection between the spleen and gonadal derivatives, first described by Bostroem in 1883.1 Since the first case published by Sneath in 1913, up to 220 cases have been published in the literature.2, 3 This entity is classified into two groups: continuous and discontinuous SGF.4 Congenital malformations occur more frequently in the continuous form, where cryptorchidism and inguinal hernias are the most frequently associated malformations.5 Typically, they are incidentally discovered during the surgical exploration of undescended testis or hernia.6 Pathological examination is sometimes necessary for two reasons: to eliminate differential diagnoses such as tumors and to avoid an orchiectomy. This was the case for our two patients with two different types of SGF, which were discovered during laparoscopic orchiopexy for bilateral cryptorchidism.
2 CASES PRESENTATION
2.1 Case 1
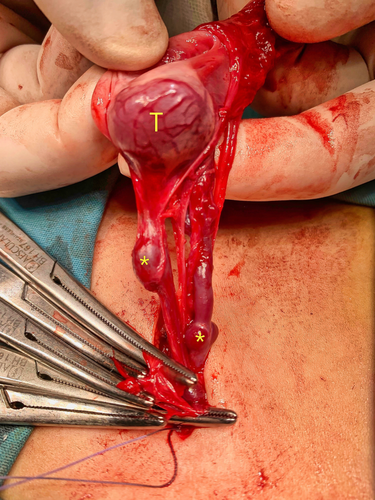
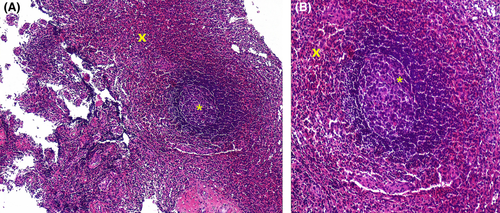
A male patient, 5 years old, presented with bilateral testicular cryptorchidism. The patient's medical and family history revealed nothing unusual, and there were no incidents at birth. Physical examination showed that the patient was in good general health except for the right testis, which was not palpable, and the left testis, which was in the inguinal canal. Ultrasound demonstrated that both testes were in the inguinal canal, having a normal echostructure without an individualizable mass or nodule. The patient underwent an initial treatment for the right cryptorchidism. After 5 months, the patient was readmitted for the treatment of the left side, which was associated with a left inguinal hernia. During the intraoperative examination, we discovered an intra hernia globular testis with two ovoid redness formations of 4 mm (Figure 1). There was no connection between the testis and the lower edge of the spleen. One of the nodules and the testis were biopsied (Figure 2), showing a normal splenic parenchyma during histological examination. Both the intraoperative findings and the pathology report confirmed the diagnosis of discontinuous SGF.
2.2 Case 2
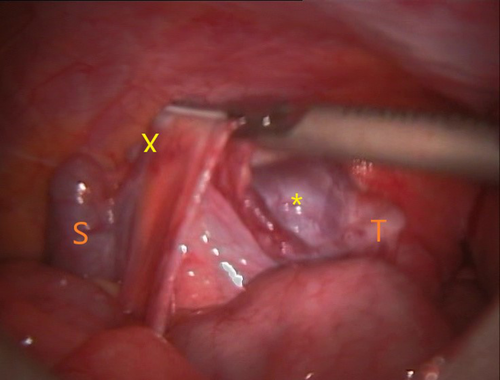
An infant was followed up in our pediatric surgery department for disorder of sex differentiation since the age of 26 days, stage III of Prader with a 46, XY genotype. Magnetic resonance and ultrasound imaging failed to detect any gonads. At the age of 9 months, the patient had a diagnostic coelioscopy (Figure 3), as part of the exploration of his disease, that demonstrated bilateral intraabdominal testes. There was a left testicular nodule connected to the lower edge of the spleen with a cord-like structure. One month later, an orchiopexy for the right testis and a biopsy of the left testis were performed. The histological examination showed a normal splenic parenchyma; thus, the diagnosis was continuous SGF. At the age of 1 year and 3 months, a Fowler–Stephen orchiopexy for the left testis was performed, respecting the testicular nodule.
3 DISCUSSION
Splenogonadal fusion is a very rare, benign congenital abnormality, occurring most frequently in male patients.1, 3, 5 To date, one case has occurred in a newborn with a 46, XY genotype who is phenotypically female.7 Our second case report is also another condition of SGF associated with a disorder of sex differentiation. The age of diagnosis ranged from stillborn to 81 years,8 but it is common in people under the age of 20.1, 3
Most cases are diagnosed accidentally during surgery,5 and nearly 17% of the reported cases are diagnosed during an autopsy.9 Some patients develop asymptomatic testicular mass; however, patients may rarely develop symptoms linked to splenic involvement (leukemia, mononucleosis, malaria, and salmonellosis) or to intestinal obstruction caused by the intraperitoneal cord, or further symptoms related to a traumatic rupture of the ectopic spleen.3, 5, 10 Our two cases were incidentally discovered during the exploration of or the treatment for other congenital malformations.
The exact pathogenesis of SGF is not yet clear. However, most studies mention that the close proximity between the left dorsal mesogastrium and the left urogenital fold that contains the gonadal mesoderm during the 5th and 6th weeks of gestation is responsible for abnormal fusion.11 This theory may explain why most SGFs are left-sided.1, 3, 5 Some authors support the theory of the migration of splenic cells.11 In fact, the migration of splenic cells to left diaphragmatic ligament disturbs its normal degeneration, causing cryptorchidism,11 and the right-sided SGF reported in the literature is also explained by this theory.11
Putschar and Manion described two types of SGF dependent on the presence or absence of a connection between the main spleen and the testis.4 These two types occur approximately with the same frequency1, 3, 5 and with a little predominance of continuous forms.5 Congenital malformations occur most frequently in the continuous form.1, 3-5, 11 Cryptorchidism and inguinal hernias are the most frequently associated malformations.1, 3, 5, 11
Continuous type of SGF associated with sexual ambiguities is much rarer. In his review of 40 SGF cases, Chen et al. reported one patient presenting phenotypical sex reversal.3 Our second case report is a continuous form of SGF associated with bilateral testicular cryptorchidism with intraabdominal testes and with malformations related to disorder of sex differentiation.
The discontinuous form is rarely associated with congenital malformations.1, 3-5, 12 However, our case of discontinuous SGF was associated with bilateral testicular cryptorchidism associated with left inguinal hernia, which is uncommon.
Preoperative discovery of this lesion by ultrasound, computed tomography, or magnetic resonance imaging is very uncommon,1, 5, 12 and was the scenario for our two cases.
Our two SGFs were biopsied and demonstrated normal splenic parenchyma. Microscopically, the splenic tissue may also show increasing lobulation or regressive changes such as fibrosis, thrombosis, calcification, fat degeneration, or hemosiderin deposits.1, 12 One case with intermingling of splenic and gonadal tissue histologically has been reported.12
In Carragher's review, published in 1990, up to 37% of SGF patients underwent unnecessary orchidectomy,1 while Malik et al. reported orchidectomy in 24% of cases.12 Finally, in the review by Chen et al., 14 of the 40 cases underwent an orchidectomy, which was potentially unnecessary in nine cases.3 Surgical treatment of SGF is very controversial, but orchidectomy is not generally indicated in cases without associated testicular neoplasm.5 For some authors, abstention can be discussed if the anomaly is recognized perioperatively and if it does not manifest clinically.5 If surgery is needed, we can choose to respect the splenic tissue of the testicle1, 5 and orchidectomy must be reserved for difficult dissections or suspected cases.5, 12
In conclusion, SGF is a rare, benign congenital abnormality that can be easily confused with testicular neoplasm. Surgeons must be averted toward this misleading entity. Pathologists can help with the diagnosis to reduce unnecessary orchidectomy in young patients.
AUTHOR CONTRIBUTIONS
Dr khouloud Ben Lazreg, Dr Imen Helal, Dr Fatma Khanchel, and Dr Sirine El Fekih conceptualized and designed the study, and acquired, analyzed, and interpreted the data. Dr Aida Daieb and Dr Sameh Tlili conceptualized and designed the study, drafted the manuscript, and critically revised the manuscript for important intellectual content. Dr Ehsen Ben Brahim and Dr Raja jouini critically revised the paper for important intellectual content. Dr Youssef Helal and Dr Achref Chadli-Debbiche approved the final version of the manuscript to be published.
ACKNOWLEDGMENT
None.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
ETHICAL APPROVAL
No study on humans or animals was conducted. Informed consent for publication was received from the patients.
CONSENT
Written informed consent was obtained from the patients' parents to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this work are available from the corresponding author upon reasonable request.




