Intrusion of overerupted molars with temporary anchorage devices before prosthetic reconstruction: A case report
Abstract
Extraction of teeth without adequate prosthetic rehabilitation frequently can lead to overeruption of opposing teeth, which may cause occlusal disturbances and complicate dental restoration. Equilibration with consequent need of endodontic treatment, surgical intrusion or extraction are often indicated as a remedy in such cases. The article proposes a method of orthodontic intrusion with the use of temporary anchorage devices as a predictable and less invasive option. Important clinical aspects of molar intrusion with respect to surrounding anatomical structures are also discussed.
1 INTRODUCTION
Patients with missing posterior teeth are likely to present with consequent overeruption of unopposed dentition.1 In particular, severe overeruption poses a great challenge for the treating dentist because frequent occlusal disturbances and loss of interarch space hinder prosthetic reconstruction of the missing teeth.2 Functional and spatial concerns may be further complicated in adult patients with compromised dental and periodontal health.3 Several approaches are possible in such cases. Equilibration of overerupted teeth may be an option; however, there may be a need for a consequent endodontic treatment.4, 5 En bloc impaction using a segmental alveolar surgical approach has also been recommended.6 Orthodontic intrusion of overerupted teeth is a conservative option, which preserves tooth structure and avoids invasive surgical procedures.7, 8
However, orthodontic molar intrusion, let alone intrusion of entire posterior segments, is a difficult task due to large root surfaces and lack of posterior anchorage. Many methods of molar intrusion have been introduced in the past, especially in treating patients with an anterior open bite. These include magnets,9 transpalatal arches,10 prefabricated functional appliances,11 vacuum-formed retainers with elastics,12 high interim restorations on opposing teeth,13 and temporary anchorage devices.14, 15 Some of the above-mentioned techniques require the presence of opposing teeth or excellent compliance, and are not always able to predictably achieve sufficient amount of tooth movement. The use of skeletal anchorage devices has many advantages and seems to provide predictable results.16, 17 The main advantages are the ability to achieve true intrusion without any unwanted tooth movement of the surrounding teeth, precise and consistent dosing of the intrusive force and the possibility of local, problem-focused treatment.7, 18-21
The aim of this article was to demonstrate a simple method used on two severe cases of overeruption of maxillary and mandibular posterior segments. Important clinical aspects of molar intrusion with respect to the surrounding anatomical structures are also discussed.
2 CLINICAL REPORT
2.1 Case 1
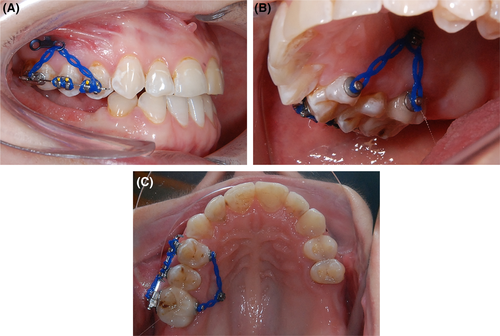
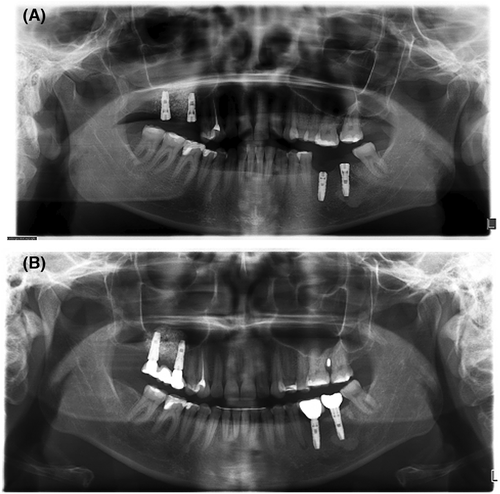
A 31-year-old woman presented to the Department of Orthodontics with a referral from the treating implantologist. The chief complaint was the overeruption of the upper right posterior segment, including the first upper molar and both premolars. The concerning teeth contacted the opposing alveolar crest tissues, preventing prosthetic reconstruction in the edentulous area (Figure 1).

Intraoral examination together with assessment of the panoramic radiograph revealed missing upper left maxillary and lower left mandibular molars, a missing upper right second molar and impacted upper and lower right third molars. The lower right first premolar presented with a large periapical radiolucency requiring endodontic treatment. The patient underwent orthodontic treatment in her childhood. One lower incisor had been extracted, with a consequent midline shift and an asymmetric treatment result (Class II on the right and Class I on the left side). To make sure that the patient was periodontally stable before any planned treatment, she underwent regular hygiene visits with detailed cleaning by an experienced hygienist.
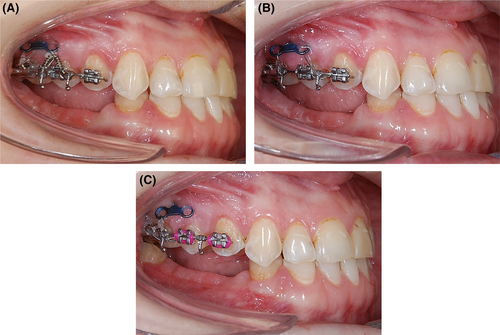
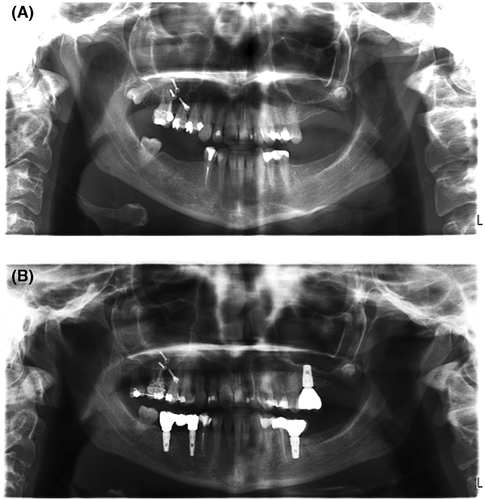
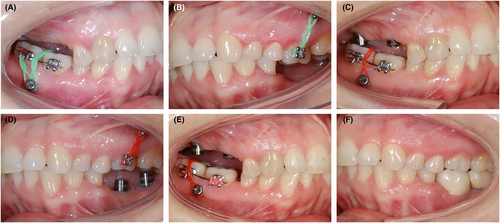
After discussing possible treatments options with the patient and her implantologist, an agreement was made for problem-focused treatment in the maxillary right posterior segment. The treatment plan included the intrusion of the overerupted teeth by 3 mm to level the occlusal plane, creating space for future implant supported prosthetic reconstruction in the opposing arch. For this purpose, a palatally placed miniscrew inserted between the second premolar and first molar (length 10 mm, 2.0 mm diameter, Type JD, Jeil Medical Corporation), and a T-shaped miniplate placed on the zygomatic crest fixed with two fixating screws (CMF System, Helmut Zepf Medizintechnik Gmbh, Seitingen-Oberflacht) were chosen as skeletal anchorage devices. The patient was instructed on how to maintain proper hygiene around the anchorage devices using a solo tooth brush and a mouth rinse (Curasept). To provide attachments on both buccal and palatal surfaces of the overerupted teeth, a segmental fixed appliance (Victory Brackets, Buccal Tubes, Roth prescription, 0.022-inch slot, 3 M, Unitek, Sherman Oaks, and .018×.025-inch stainless steel passive segmental arch wire) and orthodontic round button attachments (Rocky Mountain Orthodontics) were used. Symmetrically dosed force was applied using an elastic chain (Rocky Mountains Orthodontics, Denver) (Figure 2). After 2 weeks of initial healing and removal of the sutures, a force of 150 g was used on both sides and gradually reactivated in monthly intervals. The amount of force was measured using the force gauge (Correx, Haag-Streit). As the intrusion continued, a need occurred to enlarge the effective activation distance between the miniplate and the fixed appliance. Therefore, two crimpable hooks (Rocky Mountains Orthodontics) bent occlusally were applied to the segmental arch wire. The elastic chain was replaced with a nitinol coil spring through one of the eye-lets (150 g, 3 M Unitek). The treatment progress is shown in Figure 3. The planned intrusion was achieved after 12 months and the result was maintained until the end of prosthodontic therapy by stainless steel ligature anchors placed between the miniscrew and miniplate and orthodontic attachments. As a result of the intrusion in the upper arch, spontaneous eruption of the impacted lower right third molar with finished root development occurred. Surgical uncovering was then performed to enhance the eruption of both the upper and lower third molars. Alignment of the upper right third molar was planned and carried out with the use of temporary anchorage devices to prevent any unwanted distal movement of the intruded posterior segment. A sectional arch wire and gold chain bonded to the occlusal surface was used for this purpose. A buccal tube was bonded when the tooth erupted sufficiently. The orthodontic treatment continued for another 12 months to mesialize and extrude the upper third molar. After completing orthodontic treatment, the implantologist placed dental implants in the edentulous areas. Four implants (26, 36, 45, 47) were placed under local anesthesia (Dentis Submerged, Dentis Co., Ltd.) with simultaneous augmentation of the deficient buccal cortical bone (36, 45, 47) by the guided bone regeneration technique (BioOss S and Hyprosorb membrane) and sinus lift (26). After 6 months of healing, implants were restored with screw-retained zirconia (ZrO) porcelain crowns with titanium base in 26 and 36, and an implant-borne screw-retained bridge in 45–47 (Figures 4 and 5). The only retention device provided to the patient was a short retainer bonded to the buccal surface of 16 and 18 (0.0215-inch, 5-stranded coaxial, Penta-One, Gold'n Braces, Gold Harbor), preventing relapse following mesialization of the third molar. All temporary anchorage devices were removed after the prosthetic reconstruction was finished.

2.2 Case 2
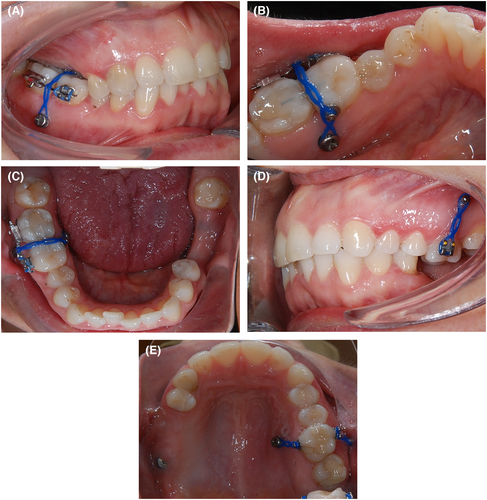
A 33-year-old woman was referred to our department from the treating implantologist. The chief complaint was that her lower right posterior teeth were touching the opposing gingiva, where two dental implants (Astra Tech, Densply Sirona) had already been placed in positions of 15 and 17 after previous bone augmentation procedures (Cerabone and autologous bone). In addition, after the loss of the lower left posterior teeth, her upper left first molar overerupted, hindering prosthetic rehabilitation of the previously placed implants in the lower left segment in positions 36 and 37 (Astra Tech, Densply Sirona). Intraoral dental examination and assessment of panoramic radiograph revealed acceptable Class I occlusion with normal overjet and overbite, mild crowding in the lower anterior segment and endodontically treated 13 (Figure 6). Hygiene was scheduled before starting the orthodontic treatment to make sure no periodontal inflammation was present.

The recommended plan included comprehensive treatment with fixed appliances in both arches; however, the patient declined, electing a problem-focused plan in the overerupted quadrants. After discussing the options, intrusion of the overerupted teeth with the help of temporary anchorage devices was planned on both sides. The lower right third molar was indicated for extraction. Two miniscrews placed in the interradicular space buccally and lingually were used to intrude the upper left first molar (palatal: 2.7/10 mm, DePuy Synthes, Johnson, and Johnson, and buccal: 1.8/10 mm, IMTEC Ortho, Ardmore). Similarly, both lower right molars were intruded by means of buccally and lingually placed miniscrews (2.7/10 mm, DePuy Synthes, Johnson and Johnson). Oral hygiene instructions were given to maintain healthy tissues around the anchorage devices using a solo tooth brush and a chlorhexidine rinse.
In the upper arch, simple round button attachments (Rocky Mountain Orthodontics) were used to attach elastic chain (Rocky Mountains Orthodontics) to the anchors. In the lower arch bonded brackets (Victory, 3 M Unitek) were placed buccally with a segmental .018×.025-inch stainless steel arch wire. A second wire was bonded on the occlusal surfaces with flowable composite (Transbond Supreme LV, 3 M Unitek), and bonded buttons were used as lingual attachments. The purpose of the occlusally bonded sectional arch wire and the buttons bonded on the lingual surface was to prevent any traumatic impingement on the gingiva and slipping of the elastic chain into the interdental space (Figure 7). The patient was seen monthly for re-activation of the intrusion force, which was set to 150 g per side and verified by the force gauge. After 6 months, the lower lingual miniscrew placed between the molars loosened and was replaced posteriorly into lingual retromolar area (1.8/10 mm, IMTEC Ortho). Initially, this appeared as a complication. However, the patient subsequently decided to undergo additional orthodontic treatment in the lower arch to resolve anterior crowding. The new position of the miniscrew enabled the addition of a distally directed force vector, enhancing distalization of the lower right segment in order to alleviate the anterior crowding (Figure 8). When sufficient space was created in the vertical and sagittal directions, a full fixed appliance (Victory Brackets, Roth prescription, 0.022-inch slot, 3 M Unitek) was bonded in the lower arch. Leveling and alignment occurred with standard straightwire technique and a progression of nitinol and stainless steel wires. Slight interproximal reduction was also used to gain space. After intrusion of the overerupted molars, which took 8 months in the upper jaw and 12 months in the lower jaw, all implants were restored with cemented porcelain fused to metal crowns (36, 37) and a screw-retained Cresco bridge (15–17), respectively (Figures 9 and 10).

3 DISCUSSION
Severely overerupted molars or entire posterior segments pose a great challenge to the treating dentist. Multidisciplinary treatment including a prosthodontist, an implantologist, and an orthodontist is often necessary. A variety of approaches are possible in such cases, including equilibration of the overerupted teeth, surgical impaction or extraction.4, 22 However, these methods involve either loss of hard tooth structures and subsequent need of root canal therapy, invasive surgical procedures, or loss of the tooth itself. Orthodontic intrusion of the overerupted teeth or segments offers a more conservative approach. The use of conventional orthodontic treatment is not possible in such cases due to great anchorage demands in the vertical dimension leading to unwanted extrusion of anchor teeth. Therefore, the use of temporary anchorage devices (miniscrews or miniplates) offers a more predictable solution with minimal side effects. Another advantage of this approach is it can be limited only to a problematic area. This is particularly beneficial because many adult patients are unwilling to undergo comprehensive orthodontic treatment. Single overerupted teeth have been successfully treated with the help of various temporary anchorage devices alone or with the help of partial fixed appliances.7, 18-20 In some instances, corticotomy might facilitate intrusion.21
3.1 Insertion sites of the miniscrews and biomechanical considerations
Precise treatment planning is crucial in such cases, especially regarding miniscrew size (diameter, length), type, and placement. To avoid any unwanted tipping of the intruded tooth in the mesio-distal and vestibulo-oral directions, two miniscrews have to be placed—one on the buccal and one on the palate or lingual side. Only this arrangement can enable sufficient control of the force system as the vector of intrusive force passes through the center of resistance of the intruded tooth or lateral segment.20
In the posterior maxilla, the miniscrew should be placed in the interradicular space at the mucogingival junction to provide enough effective activation distance, while avoiding mucosal overgrowth and providing enough distance of the roots from the screw itself. The recommended angle of insertion is between 30 and 45 degrees to the occlusal plane, which minimizes the risk of root damage.23 In cases of severe overeruption, as presented in our first case, placement at the mucogingival junction may not provide enough distance, which in turn leads to failure and loss of the miniscrew by bone remodeling in the vicinity of intruded tooth.24 A higher insertion of the miniscrew is necessary in such cases in order to gain more distance from the intruded roots. The angle of insertion should be more perpendicular to minimize the risk of perforation of the maxillary sinus.23 Sinus perforations smaller than 2 mm have been reported to heal without complications and do not seem to compromise the miniscrew stability.25 However, an overgrowth of the soft tissue with consequent inflammation and failure frequently occurs around miniscrews placed higher in nonkeratinized alveolar gingiva.26 When more activation distance is needed, a miniplate appears to be a better option as the fixating miniscrews on the zygomatic crest are at a sufficient distance from the intruded roots. Moreover, the working part of the miniplate can be placed more precisely according to the biomechanical needs. Because maxillary molars have a single palatal root, there is usually enough interradicular space to insert a miniscrew on the palate, either between the molars or between the first molar and second premolar.7, 27
In the lower jaw, the insertion of miniscrews into the buccal alveolar bone is similar to the upper jaw. However, the insertion from the lingual side has not been recommended because of an increased risk of failure, probably due to jiggling forces of the tongue.28 In our second case, the lingually placed miniscrew was lost after 6 months and had to be replaced with a screw inserted to the retromolar area. The initial position was biomechanically more favorable as the resultant force was applied through the center of resistance. In the retromolar position, the resultant force was posterior to the center of resistance, causing the segment to tip distally.
3.2 Amount of force
The amount of force used for molar intrusion varies significantly in the literature. The recommended force load is usually between 100 and 200 g per side for intrusion of a single molar,7, 21, 29 and between 200 to 400 g per side to intrude a maxillary posterior segments.14 Force exceeding 400 g is not recommended as it may jeopardize the stability of the miniscrew.30 However, this also depends on the bone density at the insertion site. Miniscrews can remain clinically stable even at forces up to 900 g, when placed into dense mandibular bone.31 There seems to be a lack of agreement regarding the timing of force application, which ranges from immediate loading to 12 weeks delay.32 Most authors recommend immediate loading of the miniscrews with continuous forces, provided that primary stability is present.33, 34 In agreement with other studies, a force of 150 g per side was used in both of our cases.
3.3 Molar intrusion and anatomical considerations
Molar intrusion, apart from the desired clinical effect, may also have a negative influence on the tooth itself and adjacent anatomical structures. As in other types of orthodontic tooth movement, the risk of external apical root resorption should be considered. From histological studies, it is apparent that some resorption is always present as a result of orthodontic tooth movement.35 In most cases, resorption lacunae are restored after the end of treatment,36 and in 3%–5% of cases, severe resorption with significant loss of root structure is found.37 Studies on experimental animals and humans have shown that during intrusion of multiradicular teeth with temporary anchorage devices only clinically negligible root resorption occurs.16, 38-40 As the root is pushed into the bone and force is concentrated on the root apex, the blood supply may also be compromised. Some changes occur in the pulp as a result; however, it has been shown that these changes are only temporary and are restored back to normal in 3 months.41, 42 During intrusion, apical remodeling of the alveolar crest also occurs due to supraalveolar transseptal periodontal fibers.43-45 In cases where overeruption is accompanied by adequate bone remodeling, this may not be a problem, as the bone will level during the intrusion. However, in cases with attachment loss and reduced bone around the overerupted tooth, a fiberotomy prior to intrusion may be beneficial as it may reduce further remodeling of the alveolar crest.46 Pushing the roots into the maxillary sinus and toward the neurovascular bundle in the mandibular canal also does not seem to have any clinical implications. The wall of the maxillary sinus remodels and apposition of newly formed bone is apparent after 7 months of intrusion according to histological studies.39 In the lower jaw, the neurovascular bundle also does not sustain any damage by the intruded roots as the intrusion is gradual.38 Only a rare case of temporary paresthesia of the lower lip has been described as a result of intrusion.47
In both presented cases, sufficient intrusion of overerupted teeth was achieved. The amount of intrusion was approximately 3 mm in 12 months. The rate of intrusion was slightly slower when compared to other studies, with similar amounts of molar intrusion being achieved in 5 to 8 months.14, 29, 48
Sufficient intrusion of overerupted teeth in both cases enabled normal prosthetic reconstruction in the opposing arches. However, in the second case, intrusion of the upper left molar was overcompensated and the resulting prosthetic reconstruction of the opposing tooth was finished in the exaggerated position. Close communication with the treating prosthodontist regarding timing of reconstruction is therefore necessary to avoid such complications. Had the lower restoration been at the ideal plane of occlusion, the overly intruded tooth would have settled into occlusion.
4 SUMMARY
Orthodontic intrusion with the use of temporary anchorage devices (miniplates, miniscrews) before prosthetic reconstruction is a viable alternative to patients presenting with severe overeruption of teeth in the lateral segments, which frequently occurs after tooth loss in the opposing jaw. It provides a problem-focused treatment with safe and predictable results. This approach is particularly useful in patients, who are otherwise not in a need of a comprehensive orthodontic treatment and where alternative solutions would require a significant loss of tooth structure or invasive surgical procedure.
AUTHOR CONTRIBUTIONS
Josef Kučera treated both patients orthodontically and prepared the original draft. Ivo Marek participated on the treatment planning, reviewed and edited the manuscript. Martin Tomeček was responsible for the implant insertion, temporary anchorage placement, and prosthetic reconstruction in Case 1. René Foltán was responsible for implant placement and temporary anchorage placement in Case 2. Barbara Foltánová carried out the prosthetic reconstruction in Case 2.
ACKNOWLEDGEMENT
We thank Dr. Joe Safirstein, Oregon, USA, for an attentive reading, valuable insights and language correction.
CONFLICT OF INTEREST
All authors have no financial interest in any of the products or companies mentioned in this article.
Open Research
DATA AVAILABILITY STATEMENT
Research data are not shared.
Written informed consent was obtained from both patients to publish this report in accordance with the journal's patient consent policy.




