Scabies surrepticius: An uncommon presentation of a common dermatosis
Abstract
We report an atypical presentation of a common disease to highlight the importance of making a correct diagnosis of scabies surrepticius in front of any itchy dermatosis especially in elderly patients. The misdiagnosis of this disease results in extensive infestation, especially with the use of corticosteroids.
1 INTRODUCTION
Scabies is a common parasitic infestation caused by the mite Sarcoptes scabiei.1 It spreads predominantly through human-to-human contact. The estimated worldwide prevalence is 200 million people.1 Recently “scabies surreptious” has been established to unify the numerous variants and the atypical presentation of scabies.2
2 CASE REPORT
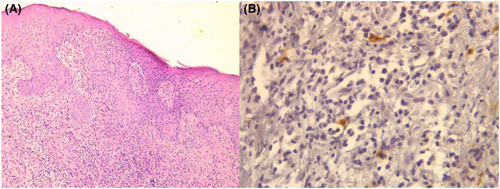
A 67-year-old man, with no particular medical history, presented with an itchy eruption, evolving over 3 months. We did not note any triggering factor (systemic or topic drug, contact allergen). Clinical examination revealed a polymorphic skin eruption (crusty erythemato-vesicular lesions associated with erythematous excoriated papules on the abdomen, trunk and limbs) (Figure 1A). There was no involvement of the face and mucosae. There were no other organs involved. The clinical diagnosis was challenging. The diagnoses mainly evoked were eczema, cutaneous lymphoma or drug eruption. We opted for a skin biopsy There was an acanthotic epidermis with foci of spongiosis, without keratinocytic necrosis, associated with an inflammatory infiltrate of moderate perivascular and interstitial density in the superficial dermis (Figure 2A). This infiltrate was made up of multiple mast cells demonstrated by anti-CD117 (C-kit) (Figure 2B). Blood count showed hyper eosinophilia. A diagnosis of urticaria pigmentosa was made based on clinical and histological findings. The patient was treated with a high-potency corticosteroid, once a day. On follow-up, 1 month later, the patient presented an extension of lesions and onset of multiple tense blisters on abdomen and thigh (Figure 1B). His wife reported a recent itch. The physical examination of his wife showed excoriated papules with scratching streaks in breast area and abdomen. The examination of the wife made us reconsider the initial diagnosis of our patient. The patient was referred for a parasitological sample with microscopic examination. The presence of eggs and excrement of sarcopte scabiei confirmed the diagnosis of scabies surreptious. Treatment of our patient and his wife with benzyl benzoate lotion in one course resulted in clinical improvement after 2 weeks.

3 DISCUSSION
Classic scabies presents with skin lesions often located on web spaces of fingers, hands and wrist. Mite-related lesions may be found in buttock, breast, areola, penis and scrotum.1, 2
The term Scabies surrepticius has been recently introduced to encompass the various atypical presentations of scabies that can be mistaken for another dermatosis.2 Subtypes of scabies surrepticius included not only crusted scabies, but also other variants: incognito, nodular, scalp-related and other less common morphologies that mimic, clinically and/or histologically other dermatoses (such bullous pemphigoid, langerhans cell histiocytosis, mastocytosis, ecthyma, pityriasis rosea, prurigo nodularis, systemic lupus erythematosus and urticaria pigmentosa).2-5
Establishing the diagnosis of scabies in these individuals can be challenging. The International Alliance for the Control of Scabies (IACS) criteria for the diagnosis of scabies may be of great help in cases of surrepticious scabies.1 Based on these criteria, the diagnosis of scabies, in our patient, may be confirmed by the visualization of eggs on light microscopy of skin samples.1
In our patient, topical corticosteroids masked the typical symptoms and led to the onset of bullous lesions. In 1975, Orkin used the term of “scabies incognito” to describe the unusual clinical presentation of the mite infestation in patients treated with topical (or systemic) corticosteroids. Clinically, skin lesions seen in scabies incognito are not specific with diffuse crusted macules, papules, nodules and blisters.3, 5
In our case, histological findings showed the presence of multiple mast cells which supported the role of these cells during scabies.4
Once the diagnosis of scabies is established, not only the patient but also close contacts should receive treatment with either topical medication (such as permethrin 5% cream, benzyl benzoate lotion) or systemic drug (ivermectin).
AUTHOR CONTRIBUTIONS
The authors fulfill the ICMJE Criteria for Authorship and contributed equally. Dr Kouki Chaima is the guarantor of the content of the manuscript, included the data and analysis. Dr Kobi Mouna contributed to interpretation of data and revision of the manuscript. Dr Linda Manaa contributed to data collection. Dr Njim Laila and Dr Mohamed Mariem contributed to analysis and interpretation of data, revised it critically. Dr Zili jamaleddine and Hichem Belhadjali contributed to final approval of the version of the manuscript to be submitted. All authors had access to the data and a role in writing this manuscript.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
None.
CONSENT
The patient in this manuscript has given written informed consent to the publication of the case details.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




