Pitfall of isolated superior mesenteric artery dissection with normal D-dimer level
All authors meet the ICMJE authorship criteria.
Sumika Uno and Shun Yamashita contributed equally to this work.
Abstract
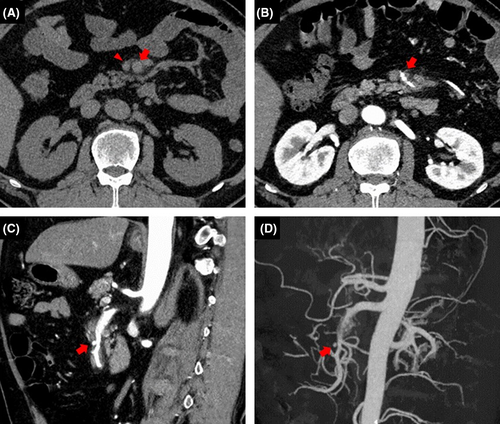
A 51-year-old man with untreated hypertension developed sudden-onset epigastric pain. Despite a normal D-dimer level, abdominal contrast-enhanced computed tomography revealed superior mesenteric artery dissection. Abdominal contrast-enhanced computed tomography is mandatory when examining patients with sudden-onset abdominal pain, even those with a normal D-dimer level.
A 51-year-old man with untreated hypertension awoke with epigastric pain, which disappeared after a few minutes. Three days later, he was transferred by ambulance to our hospital because sudden severe epigastric pain appeared when picking up a baseball. On admission, his blood pressure was 256/147 mmHg. He had epigastric tenderness and exhibited profuse cold sweating. Despite his normal D-dimer level of 0.46 μg/ml, abdominal contrast-enhanced computed tomography (CT) revealed superior mesenteric artery (SMA) dissection (Figure 1). With maintenance of his systolic blood pressure below 120 mmHg, he was discharged on the ninth hospital day without an increase in the size of the false lumen on abdominal contrast-enhanced CT.
The incidence of spontaneous isolated SMA dissection (ISMAD) is as low as 0.06%.1, 2 Although abdominal contrast-enhanced CT is required to diagnose ISMAD, it is not always performed in patients with a normal D-dimer level because of the extremely high negative predictive value of the D-dimer level for acute aortic dissection.1 However, the D-dimer level in patients with ISMAD can be normal.1 Because sudden-onset abdominal pain appears in 92% of patients with ISMAD,2 abdominal contrast-enhanced CT is mandatory even in patients with a normal D-dimer level who exhibit such symptoms.
AUTHOR CONTRIBUTIONS
SU involved in concept, literature search, and drafting of manuscript. SY involved in concept and drafting of manuscript. MT involved in concept and literature search. SI-Y involved in concept and revision of manuscript.
ACKNOWLEDGMENT
We thank Angela Morben DVM, ELS, from Edanz (https://jp.edanz.com/ac), for editing a draft of this manuscript.
FUNDING INFORMATION
No specific grant was received for this work from any funding agency.
CONFLICT OF INTEREST
The authors state that they have no conflict of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




