Central mucoepidermoid carcinoma of the mandible deriving from odontogenic cyst: A case report and review of the literature
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Abstract
Mucoepidermoid Carcinoma (MEC) it can origin from a mandibular odontogenic cyst. We report the case of a 63-year-old man with MEC of the right retromolar trigonum of the mandibula. We performed a wide mandibular excision and immediate reconstruction with a fibula bone free flap.
1 INTRODUCTION
The mucoepidermoid carcinoma (MEC) is one of the most common malignant tumor of minor salivary glands usually deriving from the glands of the palate. Less common hystotypes are adenoid cystic carcinoma, adenocarcinoma, and acinic-cell carcinoma.1-7 The World Health Organization (WHO) classification of Head and Neck tumors referred to mucoepidermoid carcinoma as “a salivary gland malignancy composed of mucinous, intermediate and squamous tumour cells forming cystic and solid patterns”.8
Although roughly 60% of MECs develop in the major salivary glands, especially in the parotid gland, they commonly involve the minor glands of the palate.9
Central MEC is a rare intraosseous variant occurring in the jaws and represents only 2% to 4% of all MECs.10, 11 It occurs most frequently in the fourth and fifth decade of life, with a male to female ratio of 1:1.4512; in 50% of cases, they are associated with odontogenic cyst or unbroken tooth.13
Several theories regarding its origin have been postulated.14-17 The most worthy considered neoplastic transformation of the epithelial lining of odontogenic cysts to be the most plausible in tumor's development.18-20
Its diagnosis is mainly based on clinical, radiographic, and histopathological findings. In literature, only 170 cases of mandibular odontogenic cysts MEC, central type, have been previously reported.
Due to its rarity, the treatment of choice for central MEC has not been outlined yet.
We present here the case of a mandibular odontogenic cysts MEC, central type, treated with a large mandibular excision and immediate reconstruction with a fibula bone-free flap,21-24 and we reviewed the existing literature.
2 CASE EXAMINATION
A 63-year-old man presented in February 2022 at the Department of Plastic Surgery of San Giovanni Addolorata Hospital (Rome, Italy) with a firm soft-tissue lesion at the level of right retromolar trigonum, complaining swallowing difficult from 2 months. We performed an excisional biopsy of the lesion, with the histological result of a low-grade MEC. Contrast-enhanced neck and chest CT showed a mass (4.1 × 2.2 × 4.7 mm) at the level of right retromolar trigonum, with well-defined margins, with cystic components and calcifications, without significative contrast enhancement.
The patient underwent a right mandible resection from level 45 to the upper maxillary branch with a right functional neck dissection (I–III levels) followed by a reconstruction time with a right fibula bone-free flap modeled by a single osteotomy and revascularized with an end-to-end anastomosis to the right lingual artery as well as to the right retro-angular-mandibular vein.
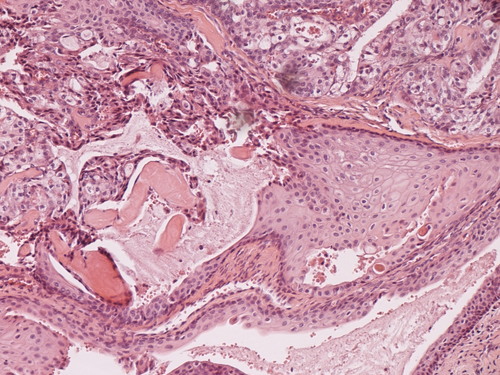
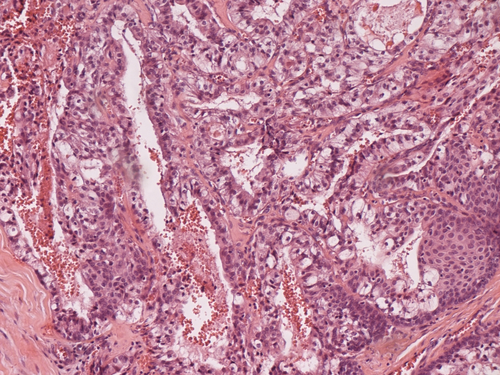
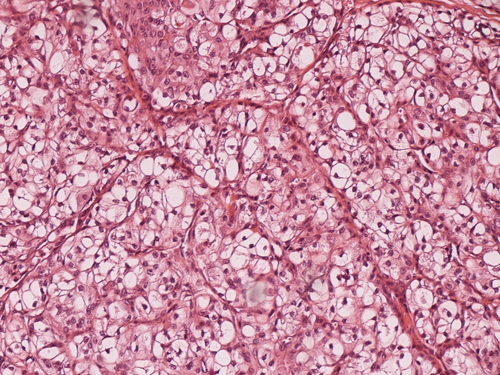
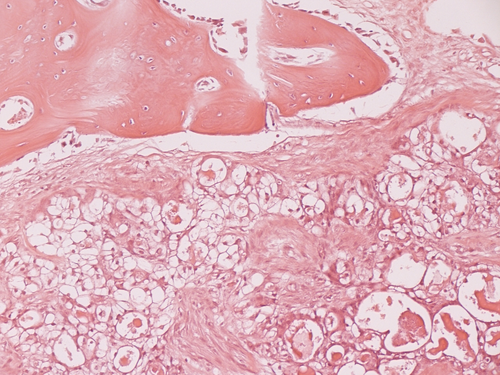
Final microscopic examination revealed an intraosseous neoplasm composed predominantly by cystic spaces and four cell types: clear cells, mucin-producing, squamous, and intermediate cells (Figures 1-4). There was a large predominance of clear and mucin-producing cells, with rare mitoses and little nuclear atypia. Mucin-producing cells were PAS and PAS-diastase positive. Moreover, a cyst covered by a normal epidermoid epithelium was detected, probably related to a pre-existent odontogenic cyst. The diagnosis was low-grade mucoepidermoid carcinoma, central type originated from a mandibular odontogenic cysts. No metastatic regional lymphadenopaties were found. The patient was discharged 13 days after surgery; his follow-up CT, performed 6 months after surgery, showed no recurrence of the disease.
3 DISCUSSION
The MEC represents the 30–50% of the minor salivary gland malignant tumors. Only 170 cases of MEC originated by a mandibular odontogenic cysts have been reported. During the years, several hypothesis have been proposed to elucidate its pathogenesis, even though it still remains unknown.25-27It seems to originate from ectopic salivar gland fragments entrapped within the bone tissue during the embryogenesis. Another possible etiopathogenesis has mainly centered on the pluripotential capabilities of the epithelial lining of odontogenic cyst. In 30 up to 50% of the cases, it is associated to the presence of included teeth.27-31
The translocation t(11;19) (q14-21;p12-13) represents the most frequent cromosomic aberration associated (30–50% MEC cases).32, 33 Histologically, this tumor consists of variable proportions of clear, mucus-producing, epidermoid, and so-called intermediate cells that show no particular differentiating characteristic. Histopathologically, it is classified as a low- or high-grade malignancy.34, 35 Radiographically, the MEC present as a unilocular or multilocular radiolucent lesion with well-defined edge, except for the more aggressive forms.
The low-grade MEC affects patients from 30 to 60 years old but it can also appear in pediatric age showing frequently cystic aspect, and it grows slowly. Radical surgical treatment with postoperative radiotherapy shows a good prognosis (95% of survival rate at 5 years).
On the contrary, the high-grade MEC affects old patients, usually with a solid aspect showing a rapid growth. Despite a radical surgical treatment with a postoperative radiotherapy could be performed, its prognosis remains poor (5% of survival rate at 5 years).36
4 CONCLUSION
A wide segmental mandibular excision with an immediate reconstruction followed by a postoperative RT (recommended only for the high-grade type) should be considered the gold standard treatment for MEC. Staging, that is, the stage of presentation, is of paramount importance for the prognosis, both for the high-grade and for the low-grade malignancies. A well-timed operation is important as much as the immediate reconstructive stage, especially low-grade tumors. In the case described, the reconstruction of the right mandible has been reached with a free fibula bone flap, which allowed functional and aesthetical reconstruction.
AUTHOR CONTRIBUTIONS
Andrea Loreti, MD, accountable for conceiving the idea. Abate Ornella, MD, responsible for the critical review for important intellectual contents. Floriana Arelli, MD, responsible for revising the manuscript for important intellectual content. Diana Spallone, MD, responsible for the critical review for important intellectual contents. Edoardo Bruno, MD, responsible for designing the work. Pietro De Luca, MD, responsible for drafting for important intellectual contents. Angelo Camaioni, MD, agree to be responsible for all aspects of the work in ensuring that questions related to the integrity of any part of the work. Leopoldo Costarelli, MD, responsible for the microscopic examination.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The authors who have taken part in this study declare that they do not have any commercial associations that might pose or create a conflict of interest with information presented in this article.
ETHICAL APPROVAL
None.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
None.




