Atypical parkinsonism can be a presenting feature of late-onset Huntington's disease
Abstract
Huntington's disease is a progressive neurodegenerative disease that typically manifests with Choreic movements, psychological disorders, and cognitive decline. Some patients can initially present atypical movements other than the usual symptoms, such as parkinsonism, ataxia, and dystonia. In this report, we present an HD patient who presented with atypical parkinsonism.
1 INTRODUCTION
Huntington's disease (HD) is an autosomal dominant and progressive neurodegenerative disease that typically manifests with choreic movements, psychological disorders, and cognitive decline. Some patients can initially present atypical movements other than the usual symptoms, such as parkinsonism, ataxia, and dystonia.1 The CAG trinucleotide repeats expansion is associated with some neurodegenerative disorders. CAG repeats within the huntingtin (HTT) gene range from 6 to 37 in disease-free people, and between 30 and 180 in affected individuals.2
In this report, we present an HD patient who presented with atypical parkinsonism.
2 CASE REPORT
A 56-year-old male patient underwent treatment for depression for 8 years and afterward gradually developed speech difficulties. Then, gait difficulties, urge incontinence, constipation, memory impairment, and frequent falling were added to his presentation during the next 4 months. His past medical history was negative for encephalitis or toxin exposure, and he had never been received neuroleptics or other antidopaminergic drugs. His father had HD and died, and his sister has HD with 42 CAG repetitions. (Video S1 and Video S2).
On examination the patient had a masked face, saccadic eye movements were slow in all directions more prominent vertically, he had upward gaze restriction, but no restriction on the downward movement. The upper and lower extremities were generally rigid and Brady-kinetic; he walked wide-base with support. He was doing repetitive movements with his hands during examination (folding and unfolding his handkerchief). He could not stand straight for more than 3 min to check blood pressure during standing, but he did not have blood pressure drop during sitting from a lying position. His speech was unclear, high-pitched, quivering, and whiny. (Video S3) The patient had significant cognitive disorders (could not perform MoCA and MMSE). He did not have REM behavior disorders.
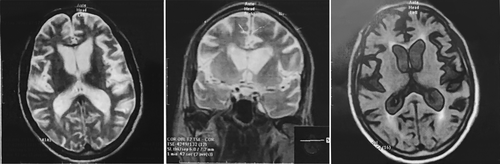
Magnetic resonance imaging (MRI) of the brain demonstrated generalized atrophy, more prominent on temporal lobes, and bilateral caudate atrophy. (Figure 1).
Regarding his family history, CAG repetition was checked for him, and genetic testing demonstrated 39 CAG repetitions on the Huntingtin gene (HTT).
He was on Donepezil 5 mg a day, Amantadine 100 mg a day, and Valproate sodium 200 mg a day. We added levodopa 25 mg three times a day and increased it gradually to 100 mg three times a day, and increased Amantadine to 100 mg twice a day, which caused mild improvement in his bradykinesia, rigidity, and gait.
3 DISCUSSION
Huntington's disease often begins with chorea. HD sometimes initiates with conditions like parkinsonian phenotype, ataxia, and dystonia,1 and it is demonstrated that longer CAG expansions are associated with this situation in the early stages of the disease,3 as well as earlier age at onset.1
Though chorea is the typical feature in HD patients demonstrating in early to middle ages, chorea may be absent in late-onset HD, generally in patients with lower CAG repetition, which commonly leads to a misdiagnosis, mainly if the genetic risk is unidentified, and disease progression is usually slower in these late manifesting patients. In addition, cognitive and behavioral problems are less common.4 Also, late-onset parkinsonism is usually levodopa responsive in contrast to early-onset HD.5
Three patients with late-onset Huntington's disease who presented with levodopa responsive parkinsonism and cardiovascular dysautonomia have been reported, at first, they were misdiagnosed as multiple system atrophy (MSA), but then HD was diagnosed (42–44 CAG repetitions).5 Another patient was reported by Ciammola et al.6 who developed depression followed by bradykinesia, gait freezing, postural instability, dystonia, and mild chorea.
Here, we report another patient with atypical parkinsonism, which was suggestive of MSA at first, but because of severe cognitive decline and positive family history of HD, CAG repetition was checked and he had 39 repeats on HTT.
Therefore, HD should be considered as a differential diagnosis of patients with atypical parkinsonism, especially if family history is positive.
AUTHOR CONTRIBUTIONS
MS involved in conception, organization, and execution of research project, and review and critique of manuscript. NBM involved in conception, organization and execution of research project. SS involved in organization of research project and manuscript writing of the first draft. ME involved in conception, execution, and organization of research project.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST
None of the authors has any conflict of interest to disclose.
ETHICAL APPROVAL
This article is taken from the disease registry, titled “Parkinson's Disease Registry in Patients Referred to Neurology Clinics of Shahid Beheshti University of Medical Sciences in Tehran (SBMU-PDR)” with the code number “IR.SBMU.RETECH.REC.1398.439” from ethics committee. supported by the deputy of research and technology at Shahid Beheshti University of Medical Sciences (http://dregistry.sbmu.ac.ir). We hereby confirm that the present study conforms to the ethical standards and guidelines of the journal.
CONSENT
The patients have given written and informed consent for online publication of their videos.
Open Research
DATA AVAILABILITY STATEMENT
Data is available on request.




