A novel UBE2A splice site variant causing intellectual disability type Nascimento
Funding information
This research was supported by funding from the Scientific Research Project of Hunan Education Department (21A0043) Xiangwen Peng, the Health Commission of Hunan Province (B2019138), Yan Shuyuan and Changsha Science and technology Plan (kq1901012), Linglin Pan.
Abstract
X-linked intellectual disability type Nascimento (XLID) is a rare disease caused by variants in the ubiquitin-conjugating enzyme E2A gene (UBE2A). Patients with XLID have similar phenotypes, including speech impairments, severe intellectual disability, hearing loss, wide facies, synophrys, generalized hirsutism, and urogenital abnormalities. Till date, only two splice-site variants of the UBE2A gene have been observed in patients with X-linked ID type Nascimento. Here, we report the case of a Chinese boy with a syndrome clinically similar to XLID with speech impairment, severe intellectual disability, and moderate hearing loss. However, different characteristics were also present in the patient, including an inability to maintain his head in an upright posture. Both of the patient's palms have a single transverse palmar crease. Subsequent whole-exome sequencing revealed a novel splice site variant in UBE2A (c.241 + 1 G > A). Our study not only expands the variant spectrum and clinical characteristics of UBE2A deficiency syndrome but also provides clinical evidence for genetic diagnoses.
1 INTRODUCTION
X-linked ID type Nascimento (XLID), characterized by a syndromic intellectual disability due to gene variants on the X chromosome, has received great attention due to the high incidence rate of intellectual disability in males.1-5 According to recent reports, the X-chromosome comprises only approximately 5% of the human genome but accounts for approximately 15% of the genes currently known to be associated with intellectual disability.6
Ubiquitin-conjugating enzyme E2 (UBE2A) is involved in the proteasome pathway for protein degradation and DNA repair7 and is located on Xq24.8-10 UBE2A contains 6 exons, and the protein contains 119 amino acids. UBE2A deficiency syndrome, also known as X-linked ID type Nascimento (MIM #300860), was first described by Nascimento in 2006 and was characterized clinically by a pronounced delay in psychomotor development, wide facies, synophrys, generalized hirsutism, a horizontal eyebrow, and urogenital abnormalities.11, 12 Since then, two splice-site variants in UBE2A, seven missense variants in UBE2A, and four larger deletions in UBE2A have been found.7, 13 However, there have been few reports of UBE2A splice site variants in China.
Here, we report the case of a Chinese patient diagnosed with XLID with a novel UBE2A splice site mutation (c.241 + 1 G > A) with a few unique clinical features. Identifying novel variants of UBE2A in XLID will help prevent disability and provide more opportunities to explore the molecular basis of intellectual disability.
1.1 Ethics compliance
Written informed consent was obtained from the patient's parents, and all of the procedures were reviewed and approved by the Ethics Committee of Changsha Hospital for Maternal and Child Health Care at Hunan Normal University (Hunan, Changsha, China).
2 CASE PRESENTATION
The proband was born on September 18, 2018; a boy, G1P1, 35 weeks 4 days gestation, birthed by cesarean section due to fetal distress, with a birth weight of 2.15 kg, and an unknown Apgar score. A history of intrapartum hypoxia or asphyxia was denied. At a gestational age of 34 weeks and 4 days, Doppler ultrasound showed that the femur and humerus were at a size expected for approximately 30 weeks of gestational age, the internal diameter of the fetal aortic arch and isthmus was slightly narrow, the umbilical vein was abnormal, the S/D ratio of the umbilical vein was higher than the RI value, and the S/D and RI values of the middle cerebral artery were lower. Neither numerical nor gross structural chromosomal abnormalities were found (Figure 1). A SNP (Affymetrix CytoScan 750 K Array) gene chip analysis revealed no pathogenic microdeletion or microduplication aberrations in the whole genome.
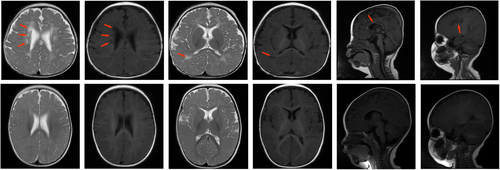
On September 18, 2018, the patient was hospitalized for 28 days for neonatal treatment at the Second Affiliated Hospital of Xiangya as a result of “premature birth and intrauterine distress” (the specific diagnoses and treatments administered are unknown). The patient remained unable to maintain his head in an upright posture from 7+ months to 40 months, and movement training was initiated. We noticed that both of the patient's palms had a single transverse palmar crease and that his intellectual development was significantly behind that of children of the same age; therefore, we considered the diagnosis of developmental delay and genetic mutation. Brain MRI (April 3, 2019) showed abnormal signal changes in the deep white matter area adjacent to the lateral ventricle (symmetrical distribution of patch-like, slightly longer T1 and slightly longer T2 signal changes can be seen in the deep white matter area beside the lateral ventricles of the bilateral cerebrum, with low signal on DWI and slightly low signal on T2 FLAIR) (Figure 2). The patient's rehabilitation program has continued till date.
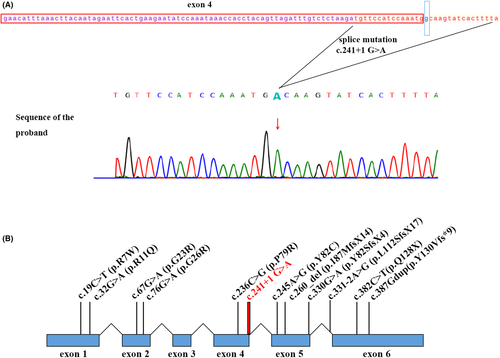
Whole-exome sequencing (WES) detection revealed the following: UBE2A:NM_003336.3:exon4:c.241 + 1G > A: variant: pathogenic (PVS1 + PM2 + PP3) (Figure 3). Strong evidence of pathogenicity (PVS1) was present as the mutation identified occurs in the splicing region and may lead to altered protein function. There was moderate pathogenic evidence (PM2) as the mutation is listed in the Berry gene Chinese population-specific database “Shenzhou Genome Database” and the Human Exon Database (ExAC), but not in the Reference Population Thousand Genomes (1000G) and Population Genome Mutation Frequency Database (gnomAD). The supporting pathogenic evidence (PP3) included the following: a conservative prediction by GERP, showing that this locus is evolutionarily conserved and has the potential for functional impact, and a protein function prediction by CADD and DANN, indicating that the mutation is harmful.
According to a public database query, UBE2A gene mutations (OMIM:312180) can cause X-linked recessive, X-linked syndromic, and Nascimento-type intellectual disability (OMIM: 300860, Budny et al. al., 2010). X-linked intellectual disability syndrome Nascimento type mainly manifests as intellectual disability, language delay, midface dysplasia, and small feet.
The results of next-generation sequencing showed that the proband had a hemizygous UBE2A mutation (c.241 + 1G > A), the mother had a heterozygous mutation, and the father had no mutation; therefore, the mutation was inherited from the phenotypically normal mother (Figure 4A).

The CNV-seq test results revealed no chromosomal aneuploidy or known, definite pathogenic genomic copy number variations (CNVs) above 100 kb (Figure 4B).
The family denied any similar medical history in the family and any genetic metabolism-related family medical history.
A physical examination conducted at the age of 7 months revealed that the patient's height was 62.5 cm, his head circumference was 40.0 cm, and his weight was 6.9 kg. The patient presented with a short stature, flat face, wide eye spacing, and a single transverse palmar crease. The patient's face was round, and his upper and lower limbs were short (Figure 5A–E). Cardiopulmonary auscultation showed no obvious abnormalities.

A professional examination was conducted at the child health department, and the patient's mental performance was determined to be normal, his responses average, and his follow-up and listening abilities were good. However, the patient insensitive to teasing, little active pronunciation and was prone to crying. He was unable to hold his head up for more than 15 s, was happy leaning back, held his head up at an angle less than 45°, demonstrated poor elbow support, was unable to roll over, and showed poor lower body weight support. The muscle tone of the limbs was low, and the tendon reflexes were slightly weakened.
In the auxiliary examination, during the patient's hospitalization in the neonatal department, echocardiography showed patent ductus arteriosus, congenital ventricular septal defect and patent foramen ovale. A hearing test (April 3, 2019) revealed the following: 40 dnBl/50 dnBl. On April 24, 2019, re-examination at our hospital revealed no obvious abnormality. An X-ray of the hip joint (December 9, 2019) at our hospital showed no obvious abnormalities, and repeated thyroid function, routine blood tests, and liver and kidney function tests showed no obvious abnormalities.
A Gesell test (May 18, 2020) was conducted and revealed the following: 29 points for adaptability, 30 points for gross motor, 34 points for fine motor, 46 points for language, and 47 points for personal-social.
Till date, for treatment, the child has been administered exercise training, EEG, EMG, intermediate frequency therapy, biofeedback, occupational therapy, language training, and other interventions in our department.
Currently, the child is able to walk with assistance. He can walk several steps by himself but cannot squat or stand alone. After a fall, the patient moves into a sitting position and stands up with the assistance of an object. He can say common names such as mom, dad, and grandma, and he can name common items, with a vocabulary of approximately 10 words. His word comprehension is dominated by nouns, approximately 30 words. He can understand simple commands. He is able to pinch pills with his thumb and index finger, but his fingertip pinching is poor. He is able to build with 2 building blocks, uses the index finger to point to objects, and can hold a pen to doodle; however, he cannot match a shape to a board, cannot self-feed with a spoon, and requires assistance with putting on and taking off his clothes. His limb muscle tone remains slightly low. The patient is uncooperative in muscle strength examinations, but the tendon reflexes can be elicited by Gesell's test (December 2, 2021), and the most recent findings are as follows: 35 points for adaptability, 29 points for gross motor, 28 points for fine motor, 47 points for language, and 28 points for personal-social.
3 DISCUSSION
In the present study, we used whole-exome sequencing to identify a novel UBE2A splice site variant (c.241 + 1 G > A) in a Chinese proband with X-linked intellectual disability. This is the second case report of this syndrome associated with novel splice site variants in China, to the best of our knowledge.
Notably, we report novel molecular and clinical data of this patient with intellectual disability. Till date, only two splice-site variants in UBE2A, seven missense variants in UBE2A, and four larger deletions in UBE2A have been reported.7, 12-21 In addition, all probands with UBE2A deficiency syndrome have similar phenotypes, including characteristic facial appearance, speech anomalies, and intellectual disability.18, 22 However, the clinical presentation of our proband was novel, including a deep single transverse palmar crease and an inability to hold the head erect, which has not been described in previous patients.
In addition, the phenotypes of all reported probands with UBE2A variant syndrome and the patient described in the present study were analyzed, and three UBE2A variant syndrome patient groups could be classified: (1) those with larger deletions (largedel), (2) those with missense variants (miss), and (3) those with splice site variants (splice) (Table 1). All patients were males and showed severe intellectual disability and speech impairment.
| References | Dingyuan Ma et.al (2019) | Giugliano et al. (2018) | Nascimento et al.(2006) | Budny et al. (2010) | Haddad et al. (2013) | Czeschik et al. (2013) | Tsurusaki et al. (2017) | Weimin Jia et al. (2019) | de Leeuw et al; Honda et al; Thunstrom et al; Czeschik et al; | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | 1 | 1 | III.3 | III.8 | 1 | 2 | IV:4 | V:2 | IV:13 | III:12 | IV:3 | III-5 | III-6 | III-7 | 5 | 1 | II:3 | |||
| General | ||||||||||||||||||||
| Type of mutation | Splice | Splice | Splice | Miss | Miss | Miss | Miss | Miss | Miss | Largedel | Miss | Splice | ||||||||
| Number of different mutation | 4 | 7 | 3 | |||||||||||||||||
| Number of patients | 9 | 13 | 4 | |||||||||||||||||
| Gender | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M |
| Ethnicity | Chinese | Chinese | Caucasian | Brazilian | Caucasian | Caucasian | Japanese | Chinese | ||||||||||||
| Mutation | c.241 + 1G > A | c.331-2A > G (p.L112SfsX17) | c.330G > A (p.Y82SfsX4) | c.382C > T | c.67G > A (p.G23R) | c.32G > A (p.R11Q) | c.19C > T (p.R7W) | c.236C > G (p.P79R) | c.76G > A (p.G26R) | c.245A > G (p.Y82C) | ||||||||||
| Gestational weeks | 35 + 4 W | NA | 39 | 40 | 35 | 35 | NA | 39 | 40 | NA | 39 | NA | NA | NA | 40 | 39 | NA | |||
| Birth weight (g) | 2150 | NA | 3970 | 3150 | 2405 | 3200 | NA | 3500 | 5500 | NA | 3600 | NA | NA | NA | 2800 | 2355 | NA | |||
| Birth height (cm) | NA | NA | 36 | 35 | 48 | 50 | NA | NA | NA | NA | NA | NA | NA | NA | NA | 46 | NA | |||
| Development | ||||||||||||||||||||
| Inability to maintain his head in upright position | + | NA | NA | NA | − | − | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | 0/0 | 0/0 | 1/1 |
| Speech impairment | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | 9/9 | 13/13 | 4/4 |
| Intellectual disability | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | 9/9 | 13/13 | 4/4 |
| Heart defects | − | NA | − | NA | + | + | NA | NA | NA | NA | NA | NA | NA | NA | − | + | NA | 9/9 | 3/4 | 0/2 |
| White matter abnormalities | + | + | NA | NA | + | NA | NA | NA | NA | NA | NA | NA | − | + | − | + | − | 6/7 | 3/6 | 2/2 |
| Dysmorphic features | ||||||||||||||||||||
| Synophrys | − | − | + | + | + | − | + | + | + | + | + | + | + | + | + | + | + | 6/9 | 12/13 | 2/4 |
| Ocular hypertelorism | + | − | + | + | + | + | − | − | − | − | − | NA | NA | NA | − | − | + | 8/9 | 3/10 | 3/4 |
| Wide face | + | + | + | + | NA | NA | − | − | + | + | − | NA | NA | NA | − | + | NA | 0/0 | 3/7 | 4/4 |
| Upslanting palpebral fissures | − | − | − | − | + | + | NA | NA | NA | NA | NA | − | − | − | − | − | + | 7/9 | 3/8 | 0/4 |
| Small feet | + | NA | − | − | + | + | − | − | + | + | − | − | − | − | − | NA | − | 5/8 | 4/12 | 1/3 |
| Generalized hirsutism | − | NA | + | + | + | − | NA | NA | + | + | + | + | + | + | + | + | + | 4/9 | 10/11 | 2/3 |
| Hearing loss/impairment | + | NA | − | − | + | NA | NA | NA | NA | NA | NA | NA | NA | NA | + | NA | NA | 2/8 | 2/2 | 1/3 |
| Genital anomalities | ||||||||||||||||||||
| Small penis | + | NA | + | NA | + | + | − | + | + | + | + | − | + | + | − | NA | − | 7/9 | 8/12 | 2/2 |
- Note: Patients with missense mutation (miss) and splice site mutation (splice) include patient 1 (described here. The patients with Larger Deletions (largedel)reported by de Leeuw et al (2010), Hoddad et al. (2010), Czeschik et al. (2013), Thunstrom et al. (2015). Each Type of Mutation are Summarized in a Separate Column—Larger Deletions (largedel), missense mutation (miss), and splice site mutation (splice), number of affected individuals with available clinical data.
- Abbreviation: NA, not available.
In our case, cardiac malformations were found in the fetal and neonatal period but disappeared as the patient grew older. This observation is different from that of other individuals with UBE2A variants with heart defects.7, 11, 12, 17, 20, 23 According to recent reports, four other patients did not have upslanting palpebral fissures. Although these analyses were based on a small number of patients and, therefore, it is difficult to draw valid conclusions, it is worth noting that this observation suggests that individuals with UBE2A splice site variants might not be at increased risk for upslanting palpebral fissures and heart defects. Conversely, individuals with UBE2A splice site variants might be at an increased risk for wide facies, white matter abnormalities and a small penis.
In this boy, the clinical presentation of this new phenotype included shorter limbs. At a gestational age of 34 + 4 W, a four-dimensional color Doppler ultrasound indicated that the femur and humerus were of a size expected for a fetus at a gestation age of approximately 30 W, which may be a new phenotype of UBE2A gene variants.
In conclusion, this report describes novel splice site variants (c.241 + 1 G > A) in the UBE2A gene resulting in an aberrant appearance and severe intellectual disability in a Chinese proband. The patient was found to have a novel clinical appearance, including a deep single transverse palmar crease and inability to hold the head erect. Our report expands the variant spectrum and clinical characteristics of UBE2A deficiency syndrome (also called XLID) and may provide clinical evidence for genetic diagnoses.
AUTHOR CONTRIBUTIONS
Jun He, Shuyuan Yan, Yanling Wang, Ying Cheng, Hongxia Yuan, Xiaoni Kuang, Da Hou, Xueyi Li, Linglin Pan, Guangwen Huang, and Jun He involved in conceptualization, data curation, and formal analysis. Tuanmei Wang involved in funding acquisition. Xiangwen Peng performed writing—review and editing.
ACKNOWLEDGEMENT
We thank the patients and healthy volunteers who agreed to participate in the present study and all those who helped us successfully complete the research.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
ETHICAL APPROVAL
The Ethics Committee of Changsha Maternal and Child Health Hospital approved this study.
CONSENT
Written informed consent was obtained from the parent's patient to publish this report in accordance with the journal's patient consent policy because the patient is a child.
Open Research
DATA AVAILABILITY STATEMENT
All data, models, and codes generated or used during the study appear in the submitted article.




