Intrahepatic and extrahepatic aminotransferase elevation associated with clinical-therapeutic events in a schizophrenic patient
Key Clinical Message
A schizophrenic patient showed rhabdomyolysis with idiopathic transaminitis. The intermixed pattern of intrahepatic and extrahepatic alanine aminotransferase (ALT) elevation is associated with respective clinical-therapeutic events. Aminotransferases play a role as surrogate biomarkers of “liver metabolic functioning” beyond the obsolete classical concept associating ALT elevation only with liver cellular damage.
Introduction
Rhabdomyolysis, a syndrome of skeletal muscle cell damage, engenders the release of toxic intracellular materials into systemic circulation 1. The pathogenesis of rhabdomyolysis is based on an increase in free ionized calcium in the cytoplasm 1. Prompt diagnosis requires routine monitoring of serum creatine kinase (CK) activity in a patient with a suggestive history or clinical features 1.
Serum concentrations of alanine (ALT) and aspartate (AST) aminotransferases have been regarded as markers of liver injury 2. Measurement of ALT and AST enzymatic activity is still most commonly done to evaluate putative liver injury 2. Blood concentrations of ALT and AST reflect liver cell membrane damage, with subsequent leakage of intracellular enzymes into circulation, especially the cytosolic ones 2. Transaminases are reliable predictors of individual components including type 2 diabetes and decreased hepatic insulin sensitivity, coronary heart disease, atherothrombotic risk profile, and overall risk of cardiovascular and metabolic disease 2. Therefore, routine testing of aminotransferases ALT and AST is now regarded as an indicator of “liver metabolic function” 2.
Case History and Examination
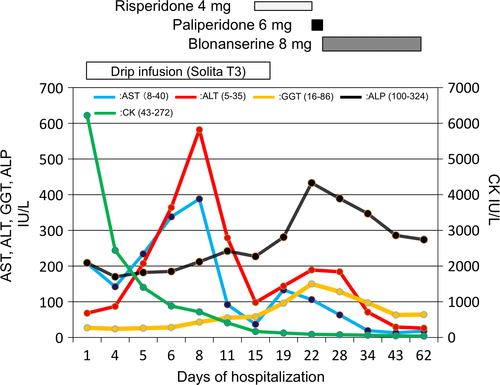
A 40-year-old man diagnosed with schizophrenia at the age of 17 had functioned stably in his community for more than two decades. A psychiatric clinic had prescribed haloperidol 3 mg and biperiden 1 mg for him. He had no known diagnosis of chronic liver disease. He denied using any non-prescription or herbal supplement. His family history was negative for liver disease and genetic myopathy. We rejected the possibility of polydipsia by history using information from his mother. Three days before admission, his condition worsened suddenly. He was admitted to our hospital because of auditory hallucinations, delusions, and chaotic and aggressive behavior. For 2 weeks, he had not taken medicines but had worked intensely. Then, aggravation of psychotic symptoms occurred. When admitted, he presented abnormal behavior, agitation, self-talking, self-laughing, and aggression in the quiet room. He refused meals and beverages. At 165.8 cm height, his weight was 58.5 kg, implying his body mass index (BMI) as 21.3 kg/m2. Physical examination revealed 147/105 mmHg blood pressure, 113 beats/min heart rate, and 36.3 °C body temperature. Skin and mucous were not dry. He had no evidence of rigidity or muscle tenderness, or of hepatomegaly. Other system examination results were unremarkable. Baseline tests such as those of serum electrolytes, urine examination, thyroid hormones, chest X-ray, brain CT, and electrocardiography all yielded normal results. Results of the main initial laboratory evaluations are presented in the Table 1: serum CK, 6622 IU/L; serum AST, 208 IU/L; ALT, 68 IU/L; and serum myoglobin, 1644 ng/mL. On the 2nd day, he was diagnosed with rhabdomyolysis. Intravenous infusion containing 35 mmol/L sodium chloride with 20 mmol/L potassium chloride (Solita T3) was started at a rate of 100 mL/h, accompanied by restriction of oral fluids under physical restraint. Antipsychotics were indicated as causing neuroleptic malignant syndrome 3. Therefore, we were unable to prescribe it to the patient because of elevated concentration of serum creatine kinase. Continued intravenous infusion caused positive balances and urine production. The individual value curve for CK, AST, ALT, alkaline phosphatase (ALP), and γ-glutamyl transferase (GGT) during hospitalization is shown in the Fig. 1. Actually, CK fell rapidly on the 4th day, although AST and ALT started to increase rapidly and mutually in parallel. The respective values of CK, AST, ALT, ALP, and GGT on the 8th day were 715, 388, 582, 212, and 43 IU/L. The AST/ALT ratio was 0.67. He had no symptoms or other stigmata of liver disease. Blood liver function tests were normal: total bilirubin, 1.02 mg/dL; cholinesterase, 221 IU/L; hepaplastin test, 73%; and international normalized ratio (INR) of 1.36. Viral serology tests for hepatitis B and C were negative (Table 1). On the 15th day, AST and ALT decreased rapidly. On the 15th day, risperidone therapy, at a dose of 4 mg/day, was started to treat his hallucinations and his chaotic and aggressive behavior. On the 19th day, his mental state was stabilized. His behavior improved. Therefore, intravenous infusion was discontinued. Meals were started. On the 22nd day, CK was normal, but ALP, ALT, AST, and GGT were elevated as shown in the Fig. 1. Subsequently, we changed to slow-release paliperidone 6 mg/day to treat his hallucinations and because of difficulty swallowing risperidone. From the 28th day, because his liver damage was suspected to have occurred as an adverse effect of risperidone therapy, blonanserin 8 mg/day was used instead. His liver function data subsequently returned to a normal range by the 43rd day. He was discharged in a stable condition with normal serum aminotransferases on the 67th day. His psychiatric condition and his health condition have remained stable.
| Normal range | 1st day | 8th day | 22nd day | 43rd day | 62nd day | |
|---|---|---|---|---|---|---|
| Creatine kinase (CK) | 43–272 IU/L | 6622 | 715 | 87 | 46 | 38 |
| Aspartate aminotransferase (AST) | 8–40 IU/L | 208 | 388 | 106 | 13 | 18 |
| Alanine aminotransferase (ALT) | 5–35 IU/L | 68 | 582 | 189 | 29 | 26 |
| Lactate dehydrogenase (LDH) | 102–204 IU/L | 562 | 513 | 295 | 147 | 141 |
| Alkaline phosphatase (ALP) | 100–324 IU/L | 209 | 212 | 433 | 286 | 274 |
| γ-glutamyl transferase (GGT) | 16–86 IU/L | 27 | 43 | 150 | 63 | 64 |
| Cholinesterase (ChE) | 237–495 IU/L | –a | 221 | – | – | – |
| International normalized ratio (INR) | 1.0–1.4 | – | 1.36 | – | – | – |
| Ammonia (NH3) | 12–66 μg/dL | – | 54 | – | – | – |
| Hepaplastin test (HPT) | 70–130% | – | 73 | – | – | – |
| Myoglobin | 0–60 ng/mL | 1644 | 168 | – | – | – |
| Total bilirubin | 0.2–1.2 mg/dL | – | 1.02 | – | – | – |
| Direct bilirubin | 0–0.4 mg/dL | – | 0.51 | – | – | – |
| Urea nitrogen | 8–20 mg/dL | 18.5 | 12.9 | 7.3 | 10.2 | 11.7 |
| Creatinine | 0.6–1.1 mg/dL | 1.09 | 0.85 | 0.67 | 0.73 | 0.85 |
| Sodium | 135–148 mmol/L | 144 | 135 | 141 | 140 | 139 |
| Potassium | 3.5–5 mmol/L | 3.6 | 4.4 | 3.9 | 4.1 | 4.2 |
| Hepatitis B antigen | Negative | Negative | – | – | – | – |
| Hepatitis C antibody | Negative | Negative | – | – | – | – |
| C-reactive protein | 0–0.3 mg/dL | 0.58 | 0.96 | 0.59 | – | – |
| Red blood cell count | 400–540 × 104/μL | 454 | 452 | 419 | 382 | 429 |
| Hemoglobin | 13–17 g/dL | 13.8 | 13.9 | 12.8 | 11.8 | 13.2 |
| Hematocrit | 35–45% | 40.6 | 39.6 | 37.0 | 34.5 | 38.5 |
| White blood cell count | 3500–9100/μL | 8870 | 5590 | 7970 | 4030 | 4550 |
- a Not determined.
Discussion
Results underscore two important clinical issues. The schizophrenic patient showed sudden onset of rhabdomyolysis. The intermixed pattern of intrahepatic and extrahepatic causes of ALT elevation is associated with respective clinical-therapeutic events.
First, the patient suddenly developed rhabdomyolysis. Psychiatric patients with rhabdomyolysis often are asymptomatic 1. The patient presented with rhabdomyolysis that was biochemically proven by an elevated CK (6622 IU/L) and AST (208 IU/L)/ALT (68 IU/L) ratio >3, which, taken together with a normal ALP and GGT indicate an extrahepatic source of transaminitis. The most common causes of rhabdomyolysis are illicit drugs, medical drugs, muscular diseases, trauma, neuroleptic malignant syndrome, seizure, and immobility 4. His past medical, medication, and family histories, respectively, rule out potential drug abuse, behavioral peculiarities such as psychogenic polydipsia and polyphagia, and genetic myopathy. Systemic bacterial infection is unlikely in the absence of inflammation of the blood chemistry tests. Unfortunately, we failed to ascertain what occurred with this patient immediately before admission. Because excessive physical activity is a major cause of rhabdomyolysis in psychiatric patients 1, somewhat elevated CK concentration might result from his excessive physical activity and concurrent interruption of routine medication.
Second, the intermixed pattern of intrahepatic and extrahepatic causes of ALT elevation is associated with respective clinical-therapeutic events. Given shorter half-lives of CK and AST and the resuscitative measures undertaken for treating rhabdomyolysis 2, 4-7, serum concentrations of CK and AST improved more rapidly than ALT during the first few days, as shown in the Table 1 and Fig. 1. Antipsychotic therapy started immediately after admission can be expected to cause liver dysfunction, which might explain the hepatotoxic pattern of overlapped elevation of ALT more than AST on days 4–8 of hospitalization that might be completely unrelated to rhabdomyolysis. This hypothesis is supported by a concomitant elevation of ALP and GGT (liver function biomarkers) and a continuous decrease in CK (rhabdomyolysis marker), as shown in the Fig. 1 and Table 1. Consequently, this allegedly unusual and mysterious elevation of transaminases that is believed to result from psychotic rhabdomyolysis might reflect intermixed patterns of intrahepatic and extrahepatic causes of ALT elevation associated with respective clinical-therapeutic events.
Two isoforms of ALT are ALT1 and ALT2. Actually, ALT1 and ALT2 appear to have not only different tissue sources but also cellular localization, suggesting dissimilar biological roles in the pathogenesis of acute or chronic liver disease 2. ALT1 is encoded by a gene of GPT1 located in chromosome 8 (8p24.3), but ALT2 is encoded by a different gene of GPT2 located in chromosome 16 (16q12.1) 2. ALT1, which is expressed primarily in liver 8, and ALT2, which is expressed primarily in muscular tissue 9, cannot be discriminated using current biochemical tests measuring serum ALT 2. Recently, most activity in circulation is found to be attributed to ALT1 10. Furthermore, elevation of ALT concentrations does not necessarily indicate hepatocellular damage 11. If two isoforms of ALT were applicable in clinical practice, then it might stimulate further insight into how these conflicting observations of seemingly unrelated clinical and biochemical events are explainable and reconciled.
In conclusion, facts associated with this case support the emerging evidence that aminotransferases are surrogate biomarkers of “liver metabolic function” beyond the classical concept of liver cellular damage because their enzymatic activity might actually reflect key aspects of the physiology and pathophysiology of the liver function 2.
Consent
Written informed consent was obtained from the patient for publication of this case report.
Acknowledgment
We acknowledge Dr. H. Matsukura for critical reading of the manuscript.
Conflict of Interest
None declared.