Journal list menu
Export Citations
Download PDFs
ISSUE INFORMATION
EDITORIALS
Global Health in the ANZ Journal of Surgery
- Pages: 1833-1834
- First Published: 13 October 2020
Thinking outside the box: not as easy as you might think
- Pages: 1834-1835
- First Published: 13 October 2020
PERSPECTIVES
Embedding a data culture in surgical practice: challenges and the need for a new approach
- Pages: 1838-1839
- First Published: 13 October 2020
Basic science education at medical school: views of students interested in pursuing a surgical career
- Pages: 1840-1842
- First Published: 13 October 2020
SPECIAL ARTICLES
Screening and testing for COVID-19 before surgery
- Pages: 1845-1856
- First Published: 07 August 2020

On the basis of a rapid review of the literature and advice from a clinical expert working group containing seven senior surgeons and a senior medical virologist, evidence-based recommendations have been produced along with a proposed schema for the preoperative screening of surgical patients suspected of having active COVID-19. A printable questionnaire has also been developed for verbally screening patients for COVID-19 during either face-to-face or telemedicine consultations.
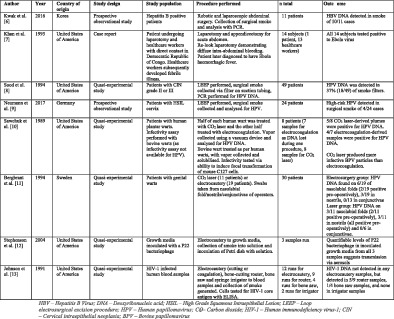
Assessing the risk of viral infection from gases and plumes during intra-abdominal surgery: a systematic scoping review
- Pages: 1857-1862
- First Published: 17 August 2020
Staying home but not out of trouble: no reduction in presentations to the South Australian paediatric major trauma service despite the COVID-19 pandemic
- Pages: 1863-1864
- First Published: 15 August 2020
REVIEW ARTICLES
Systematic review and meta-analysis of the association between diverticulosis of the appendix and neoplasia
- Pages: 1871-1877
- First Published: 24 March 2020
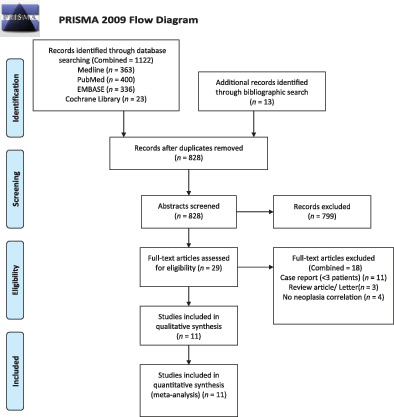
Meta-analysis of 17 147 patients from 11 eligible studies provided a pooled diverticula of the appendix (DA) prevalence of 1.74%. Presence of neoplasia in DA specimens was 26.94% versus 1.28% in appendicectomy specimens without DA. Random-effects model demonstrated that pooled risk ratio was 25.46 (95% confidence interval 12.77–50.75, P < 0.00001). The strong association with neoplasia in this meta-analysis reinforces the clinical significance of DA to surgeons, pathologists and radiologists.
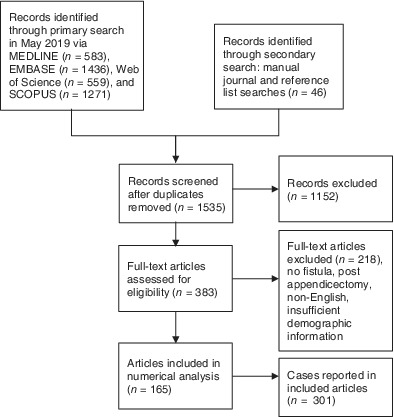
Fistulae involving the appendix: a systematic review of the literature
- Pages: 1878-1887
- First Published: 13 October 2020
Mucinous appendiceal neoplasms with or without pseudomyxoma peritonei: a review
- Pages: 1888-1894
- First Published: 05 August 2020
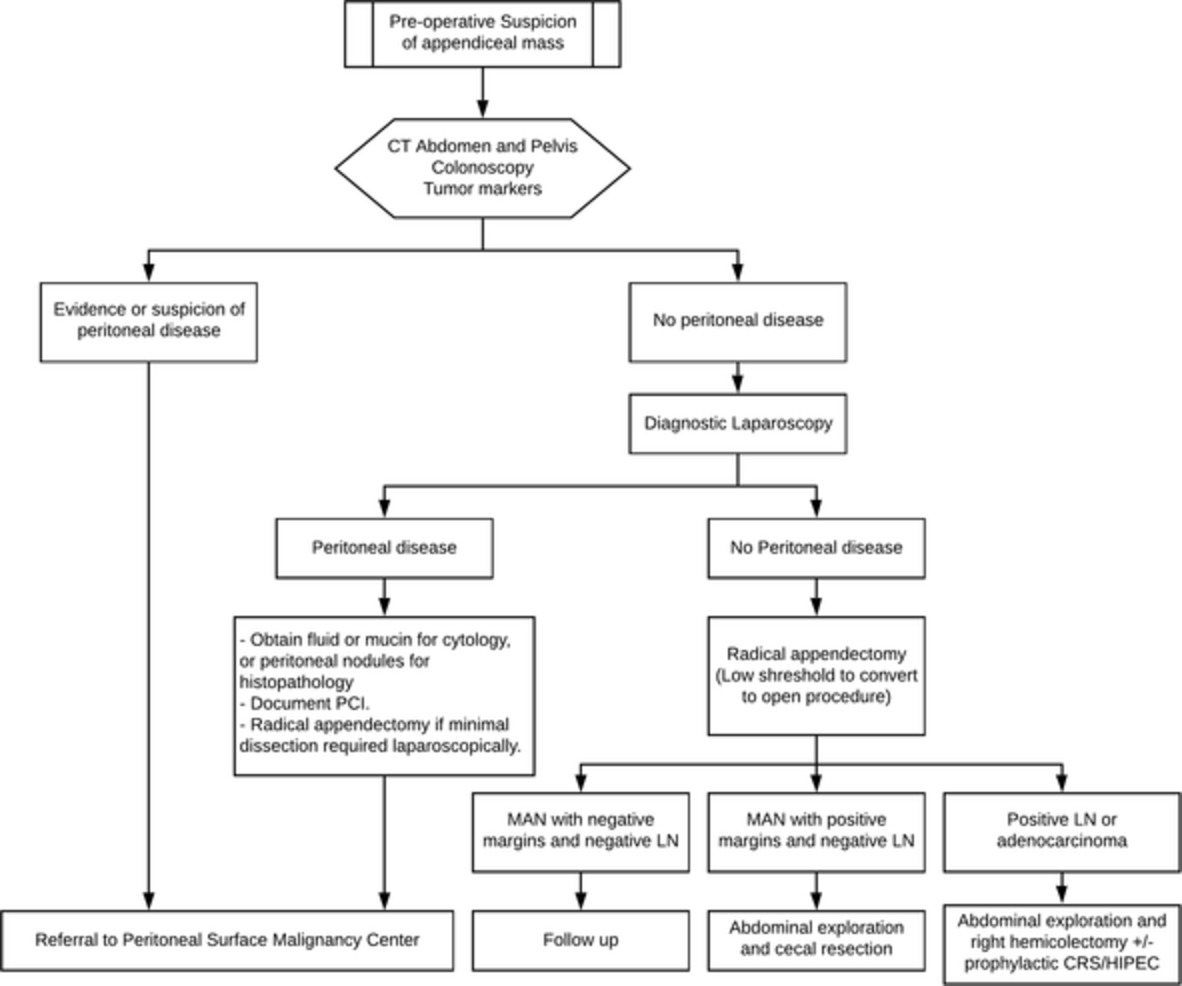
• Mucinous appendiceal neoplasms warrant from the simplest to the most complicated surgery.• The updated histopathological classification is the cornerstone of decision making.• Advanced appendiceal tumours that have spread to the peritoneum are potentially curable by surgery.• Standard treatment is cytoreductive surgery and hyperthermic intraperitoneal chemotherapy.• Better surgical technique and perioperative care greatly diminished the morbidity of CRS + HIPEC.
Risk factors for mortality after emergency laparotomy: scoping systematic review
- Pages: 1895-1902
- First Published: 24 June 2020
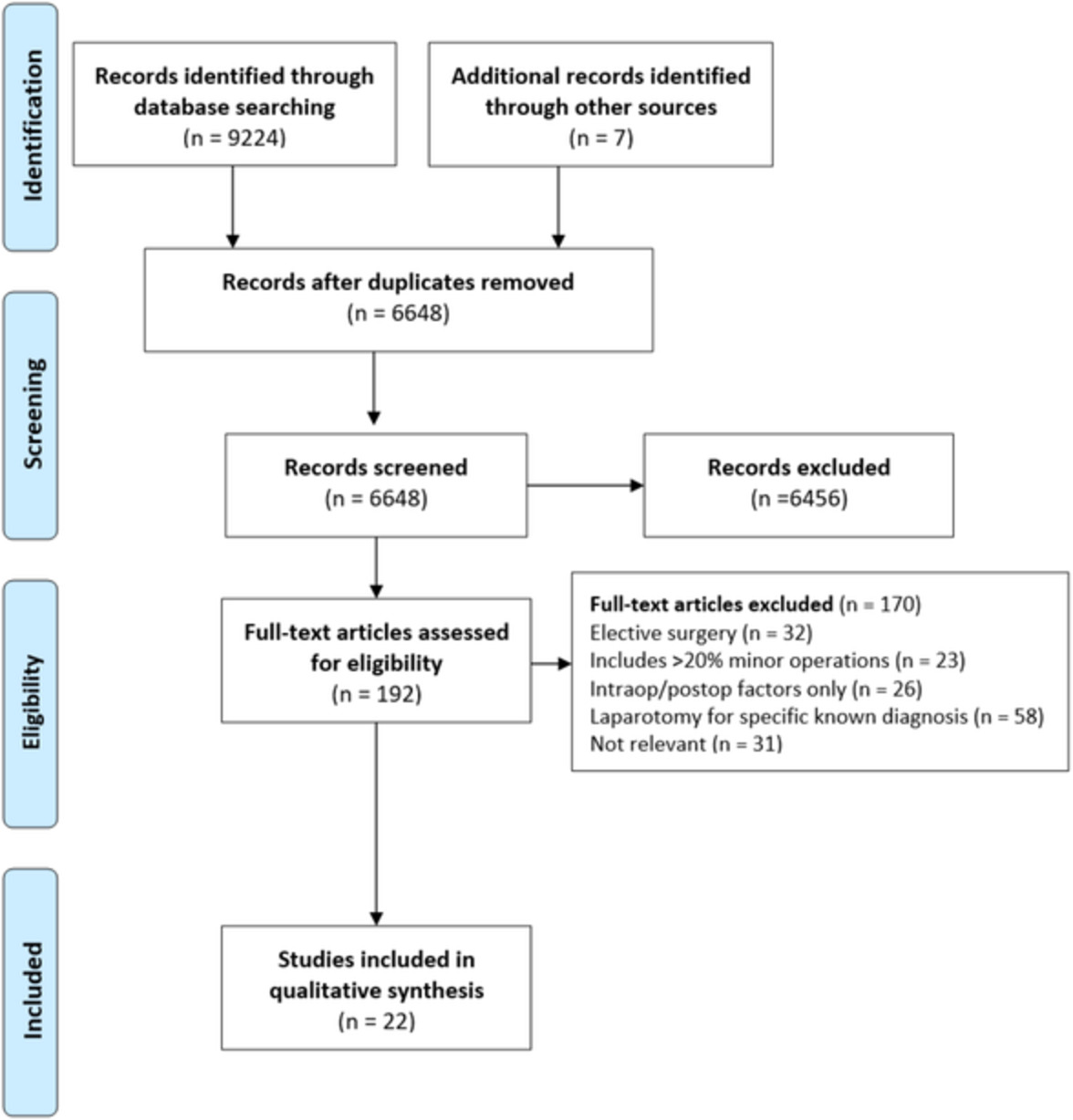
Several preoperative factors influence outcomes from emergency laparotomy. Multiple physiological derangements and comorbidity factors worsen mortality post-operatively. Increased body mass index (obese and overweight categories) are the only factors found to be protective against post-operative death following emergency laparotomy.
GLOBAL HEALTH
Universal access to safe, affordable, timely surgical and anaesthetic care in Papua New Guinea: the six global health indicators
- Pages: 1903-1909
- First Published: 20 July 2020
Delivery of surgical care in Samoa: perspectives on capacity, barriers and opportunities by local providers
- Pages: 1910-1914
- First Published: 18 June 2019
How will increasing surgical volume affect mortality in the Pacific, Papua New Guinea and Timor Leste?
- Pages: 1915-1919
- First Published: 17 May 2020
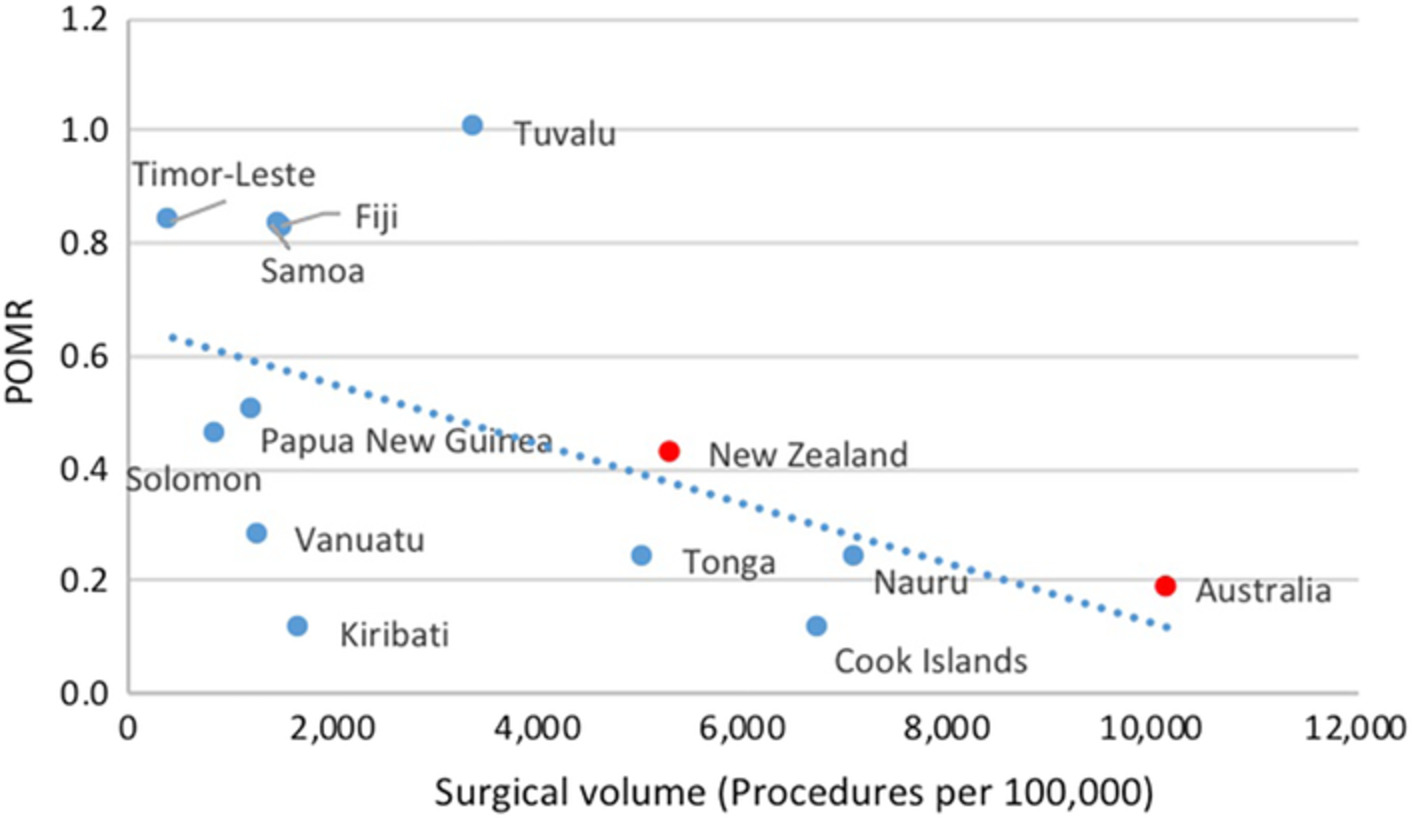
Currently the South Pacific experience about 750 postoperative deaths per year, representing 1% of crude mortality in the region. Given that more than 400 000 procedures are needed in these countries to reach the Lancet Commission of Global Surgery target of 5000/100 000, surgical scale up would result in perioperative mortality contributing on average 3.3% of all national crude mortality, assuming the POMR stays the same which is challenging to predict. Although postoperative mortality as a proportion of all mortality may increase with surgical scale up, we feel that the POMR is likely to decrease as Lancet Commission of Global Surgery targets for surgical volume are reached.
Breast disease in Timor-Leste
- Pages: 1920-1924
- First Published: 16 February 2020
A retrospective quantitative case–control study of breast-related presentation for 1 year was conducted at Hospital Nationale Guido Valadares (sole tertiary hospital) in Dili. This study was conducted to determine the burden of breast disease and to inform public health measures to address early detection, diagnosis and management.
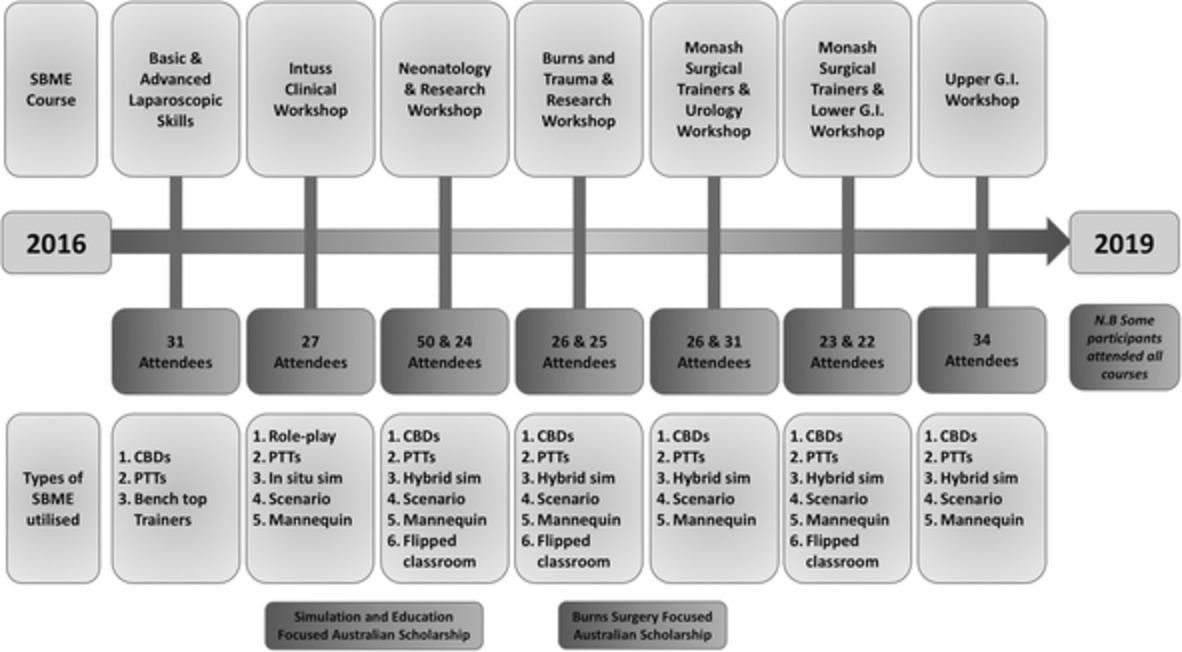
Overview of a novel paediatric surgical simulation-based medical education programme in Myanmar
- Pages: 1925-1932
- First Published: 19 August 2020
Muheza approach: a sustainable mesh hernia service in a resource-poor setting and developing a national methodology to hernia surgery in Tanzania
- Pages: 1933-1937
- First Published: 20 July 2020
PERIOPERATIVE ISSUES AND MANAGEMENT
Implementation of electronic health records systems in surgical units and its impact on performance
- Pages: 1938-1942
- First Published: 30 July 2019
The advent of electronic health record systems in Australia may increase hospital efficiencies and decrease length of stay in the setting of acute appendicitis.
Surgical Locker room Environment: Understanding the Hazards (SLEUTH) study
- Pages: 1943-1946
- First Published: 10 July 2020

There is a concerningly high burden of potentially hazardous medical waste dumped in surgical changing rooms. We hope that the current study will raise awareness of the need for appropriate disposal of medical equipment before entering changing rooms and leads to formal evaluation and initiatives to mitigate medical waste and the associated cost in our healthcare system.
Feasibility study of an online modifiable Enhanced Recovery After Surgery protocol with specific focus on opioid avoidance
- Pages: 1947-1952
- First Published: 14 May 2020

There is a growing opioid crisis in the Western world. Addiction to opioids often starts with prescriptions after a hospital admission. We evaluated the feasibility of an opioid-scarce Enhanced Recovery After Surgery (ERAS) protocol after colorectal surgery and found that opioid use was significantly reduced when this new protocol was implemented.
SURGICAL ONCOLOGY
Strategies for ‘bloodless’ surgery: the experience of cytoreductive surgery for peritoneal carcinomatosis in Jehovah's Witnesses
- Pages: 1953-1957
- First Published: 28 June 2020
Novel prognostic score for outcomes after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for colorectal cancer with metachronous peritoneal carcinomatosis
- Pages: 1958-1964
- First Published: 11 March 2020
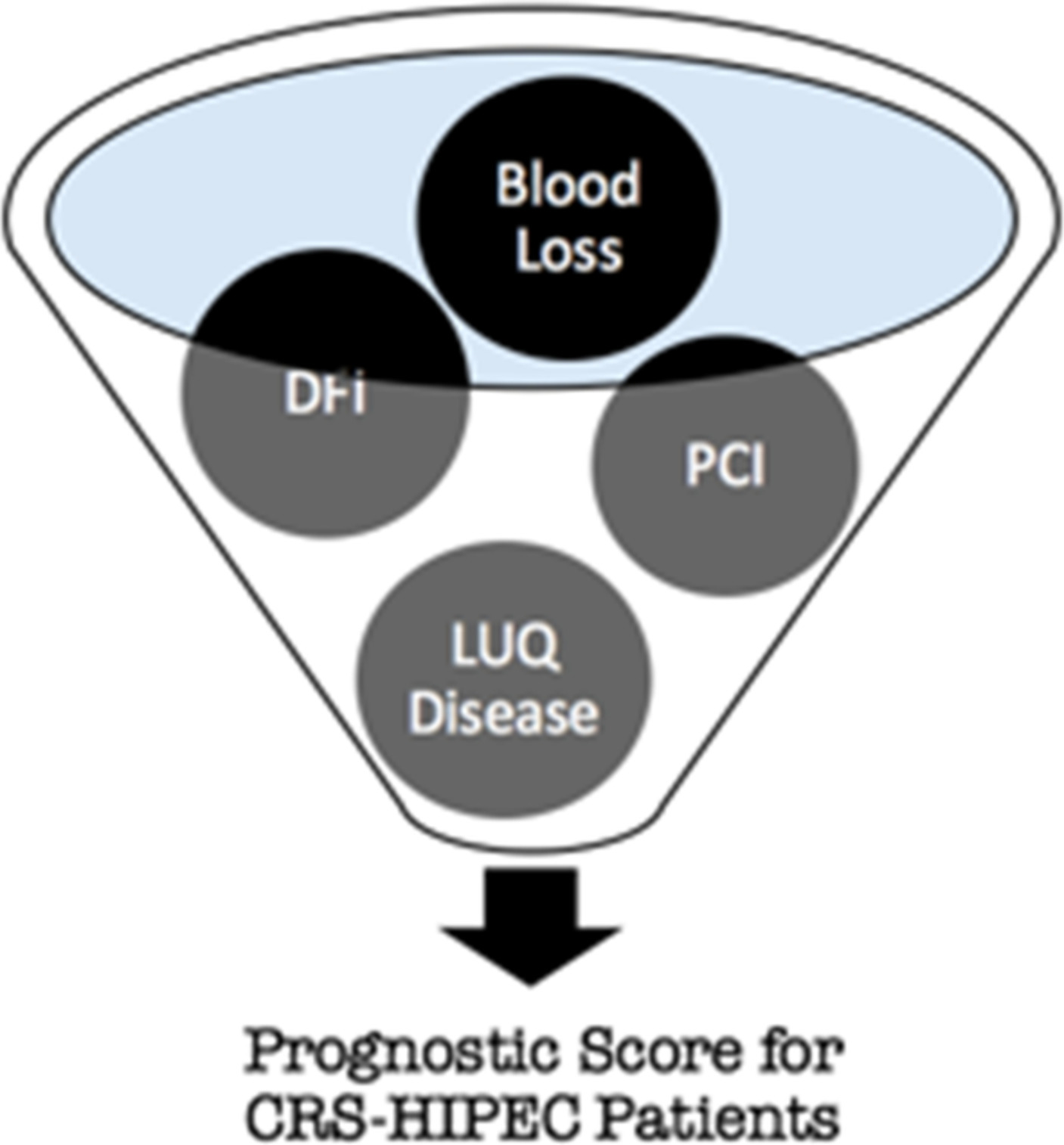
We determined pre- and peri-operative parameters with significant predictive value for post-operative outcomes in patients with recurrent colorectal cancer presenting as peritoneal carcinomatosis undergoing Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Our prognostic models provide an objective and simple risk stratification system for accurately prognosticating patients following cytoreductive surgery and hyperthermic intraperitoneal chemotherapy.
Primary pharyngolaryngectomy with jejunal free flap reconstruction: a single centre's evolving experience
- Pages: 1965-1969
- First Published: 01 May 2020
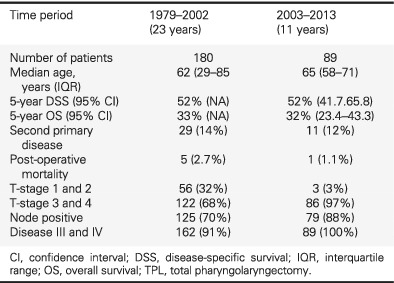
Our unit undertook a 11-year review of all hypopharyngeal squamous cell carcinomas treated with primary total pharyngolaryngectomy aiming to provide an update on survival outcomes, morbidity, post-operative complications and evolving management strategies. We report one of the largest single-centre series to date.
GENERAL SURGERY
Can normal inflammatory markers rule out acute appendicitis? The reliability of biochemical investigations in diagnosis
- Pages: 1970-1974
- First Published: 12 November 2019
Carcinoid tumours of the appendix: an analysis of emergency appendicectomies over a 24-year period and outcomes of laparoscopic versus open resection
- Pages: 1975-1978
- First Published: 09 April 2020
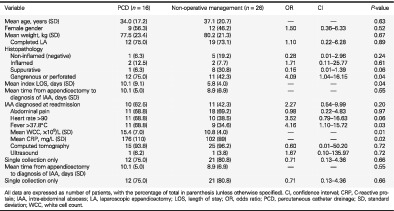
Non-operative management of small post-appendicectomy intra-abdominal abscess is safe and effective
- Pages: 1979-1983
- First Published: 08 June 2020
Cohort study of 1241 patients to identify predictors of negative appendicectomy
- Pages: 1984-1990
- First Published: 17 August 2020
A low negative appendicectomy rate may be achieved by careful clinical assessment by elucidating a patients signs and symptom duration with blood test results assessing for leucocytosis.
Cytokines in abdominal exudate and serum predict small bowel obstruction following appendectomy
- Pages: 1991-1996
- First Published: 17 August 2020
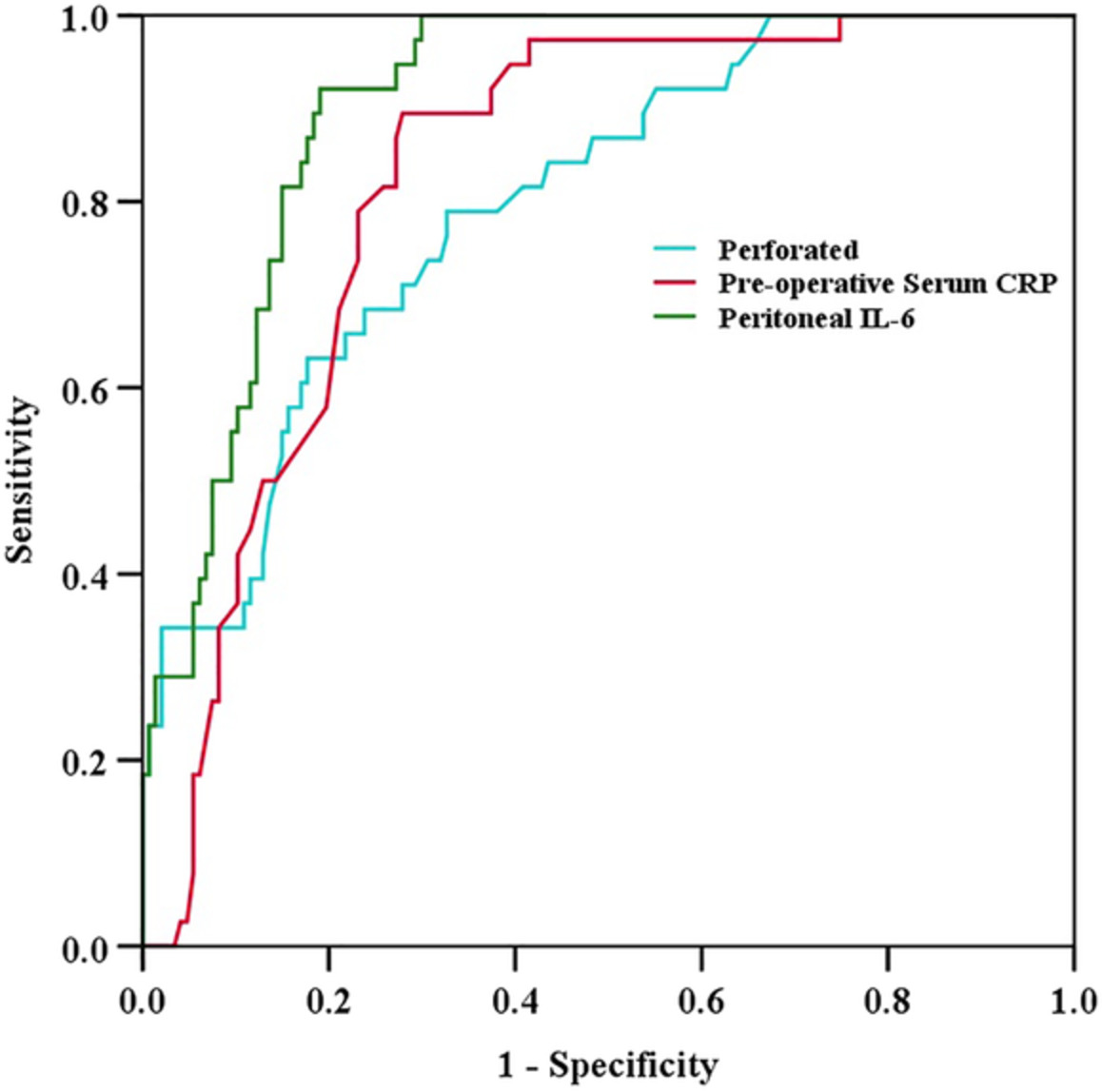
In this study, we detected the changes of C-reactive protein, interleukin-1β, interleukin-6 and tumour necrosis factor-alpha in serum and enterocoelia perioperatively. Moreover, in order to investigate the value of inflammatory markers for the prediction of small bowel obstruction, we analysed the correlation between the small bowel obstruction occurrence and the level of inflammatory markers.
HEPATOPANCREATICOBILIARY SURGERY
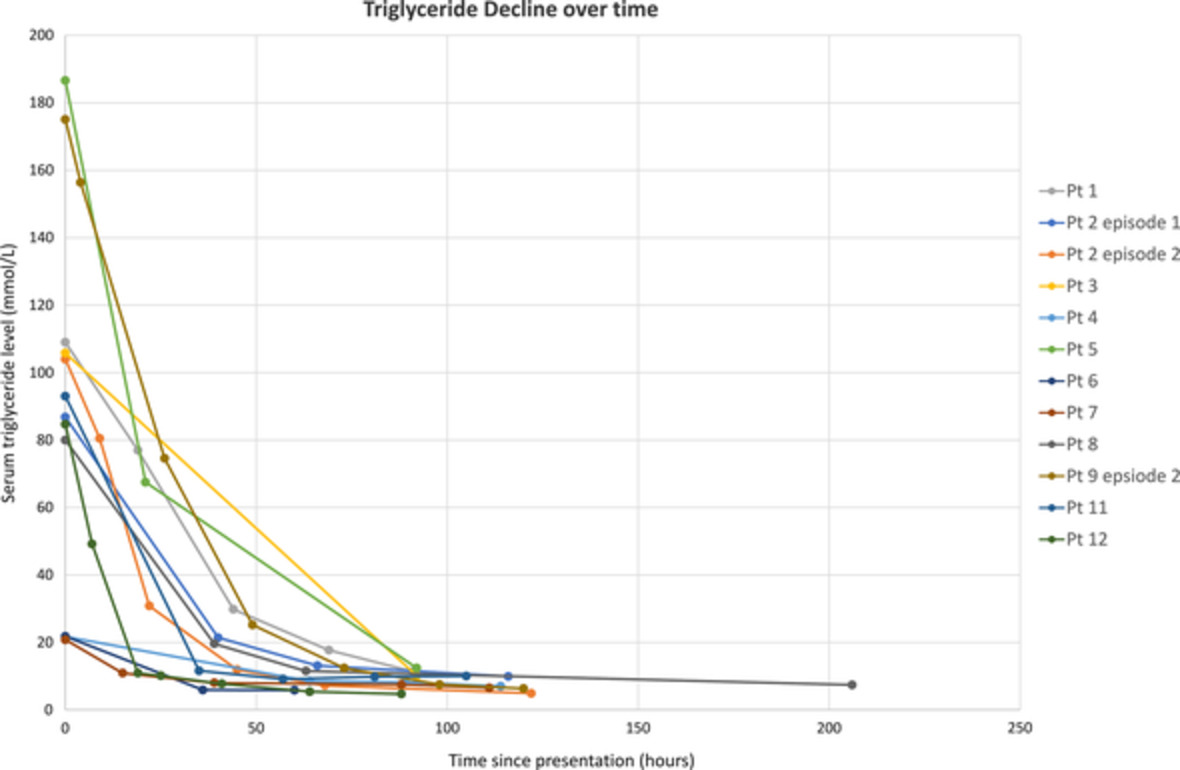
Anti-lipid therapy and risk factor management for triglyceridaemia-induced acute pancreatitis
- Pages: 1997-2003
- First Published: 19 March 2020
Diabetes-related outcomes after pancreatic surgery
- Pages: 2004-2010
- First Published: 20 July 2020
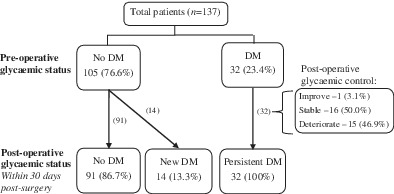
This article aims to describe the glycaemic status of patients pre- and post-pancreatectomy, compare patient's clinical characteristics, group according to pre- and post-pancreatectomy diabetes mellitus (DM) status and identify predictors of post-operative pancreatogenic DM. The development or continuance of DM within 30 days post-pancreatectomy occurs in approximately one in seven persons. No patients with pre-existing DM demonstrated a remission of DM post-pancreatectomy. All patients should be screened for diabetes pre-operatively and followed up post-operatively, particularly those with pre-existing impaired renal function.
Index cholecystectomy rates in mild gallstone pancreatitis: a single-centre experience
- Pages: 2011-2014
- First Published: 27 April 2020
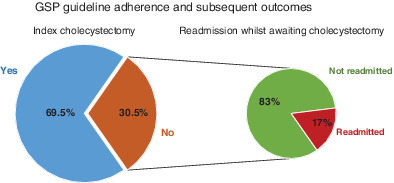
Gallstone pancreatitis has evidence-based guidelines which recommend index admission cholecystectomy in patients with mild disease. A retrospective chart audit within the Sunshine Coast Health District found a 69.5% compliance rate to the guidelines. There was a 17% readmission rate in patients not receiving index cholecystectomy reinforcing the importance of guideline adherence.
Delayed referral increases the need for surgery and intervention in patients with acute pancreatitis
- Pages: 2015-2019
- First Published: 24 August 2020
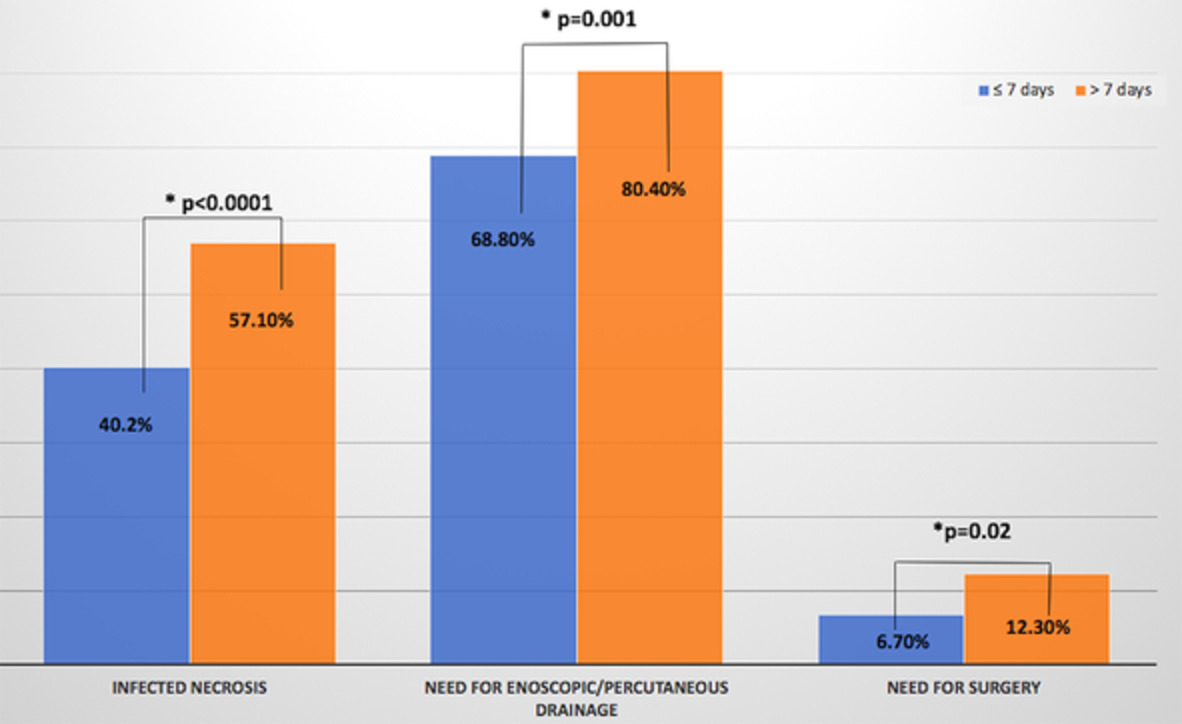
Patients with acute pancreatitis were who were referred from other hospitals a tertiary care centre were studied and their outcomes were analysed. Subgroup analysis of patients between those referred early (7 days) versus those referred late (>7 days) was done. Patients referred 7 days of pain onset had higher rates of organ failure (P = 0.007), including acute lung injury (P = 0.008) and acute kidney injury (P = 0.026) whereas those referred late had higher infected necrosis (P < 0.0001), requirement of endoscopic/percutaneous drainage (P < 0.001) and need for surgery (P < 0.02).
Comparison between video-assisted retroperitoneal debridement and small incision pancreatic necrosectomy in infected pancreatic necrosis
- Pages: 2020-2025
- First Published: 11 August 2020

Our aim was to evaluate the outcome by comparing video-assisted retroperitoneal debridement (VARD) and small incision pancreatic necrosectomy (SIPN) for infected pancreatic necrosis. SIPN and VARD are both an effective treatment for infected pancreatic necrosis with acceptable mortality and complication rates. SIPN can reduce the rate of reinterventions due to poor clinical improvement with a shorter hospital stay and a lower total cost compared with VARD.
Predicting survival in non-functional pancreatic neuroendocrine tumours
- Pages: 2026-2031
- First Published: 26 June 2020
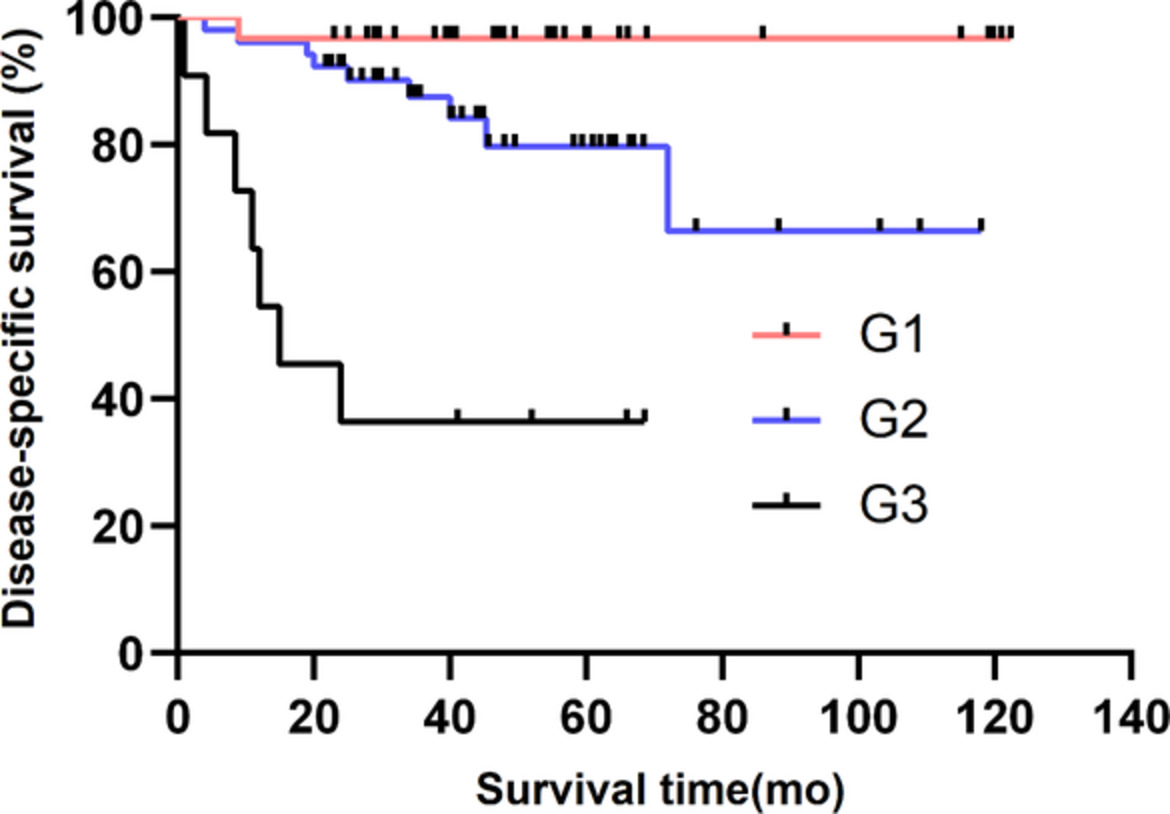
This study aimed to show the surgical outcomes of the non-functional pancreatic neuroendocrine tumours (NF-PNETs) and evaluate the factors predicting disease-specific survival for well-differentiated NF-PNETs (grade G1 and G2 tumours without synchronous distant metastasis). A total of 103 NF-PNETs (40%) were identified for analysis. Age >52 years and tumour grade G2 might be independent predictors of poor disease-specific survival for patients with well-differentiated NF-PNETs.
COLORECTAL SURGERY
Influence of obesity on the risk of recurrent acute diverticulitis
- Pages: 2032-2035
- First Published: 04 March 2020
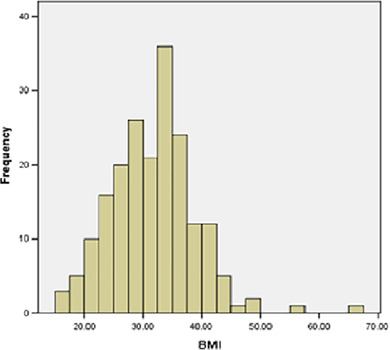
Acute diverticulitis is a common surgical condition, the risk of which has been shown to be increased in obese patients. The risk of recurrent diverticulitis in obese patients has not been well demonstrated previously. We found obesity did not significantly affect the risk of recurrent acute diverticulitis in a cohort of over 1000 patients.
C-reactive protein trajectory in the first 48 hours predicts the need for intervention in conservative management of acute diverticulitis
- Pages: 2036-2040
- First Published: 04 August 2020

This paper demonstrates the utility of a dynamic assessment of C-reactive protein in predicting the failure of conservative management of acute diverticulitis in patients not needing immediate surgery or radiological intervention. If the C-reactive protein is persistently high or is rising in the first 2 days of admission, then there is a higher risk of intervention during the hospital admission. This is the first time such a dynamic assessment is performed in patients with acute diverticulitis.
Associations of novel inflammatory markers with long-term outcomes and recurrence of diverticulitis
- Pages: 2041-2045
- First Published: 28 August 2020
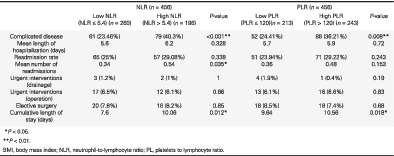
High neutrophil-to-lymphocyte ratio (NLR)/platelet-to-lymphocyte ratio (PLR) is associated with complicated diverticulitis. High NLR/PLR is associated with higher rate of recurrence of acute diverticulitis. High NLR/PLR is associated with longer length of stay when adding all of the hospitalizations for acute diverticulitis.
Acute diverticulitis: an ongoing economic burden on the health system
- Pages: 2046-2049
- First Published: 17 August 2020
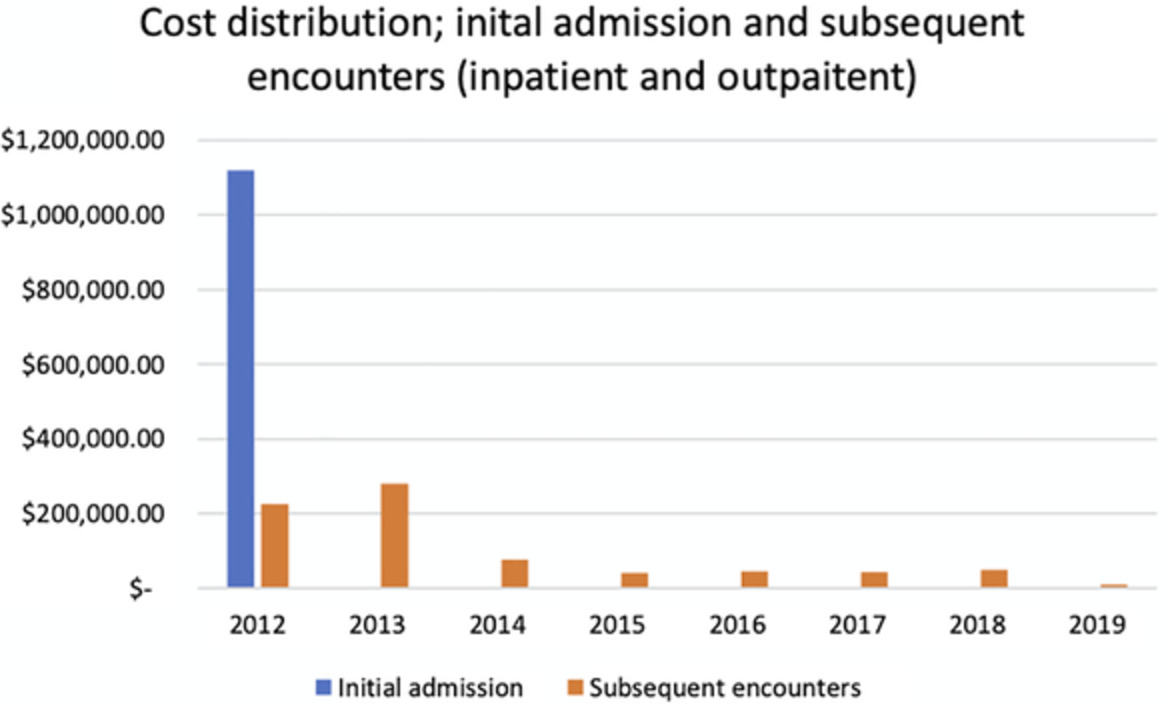
This study provides an accurate estimate of the overall healthcare cost of acute diverticulitis and its sequelae. There are considerable long-term costs associated with the index episode of diverticulitis with only 57% of the cost occurred at initial admission. A large proportion of the expenditure is incurred by a small group that included those with complicated disease. These findings are important for healthcare resource allocation and for targeting health research funding.
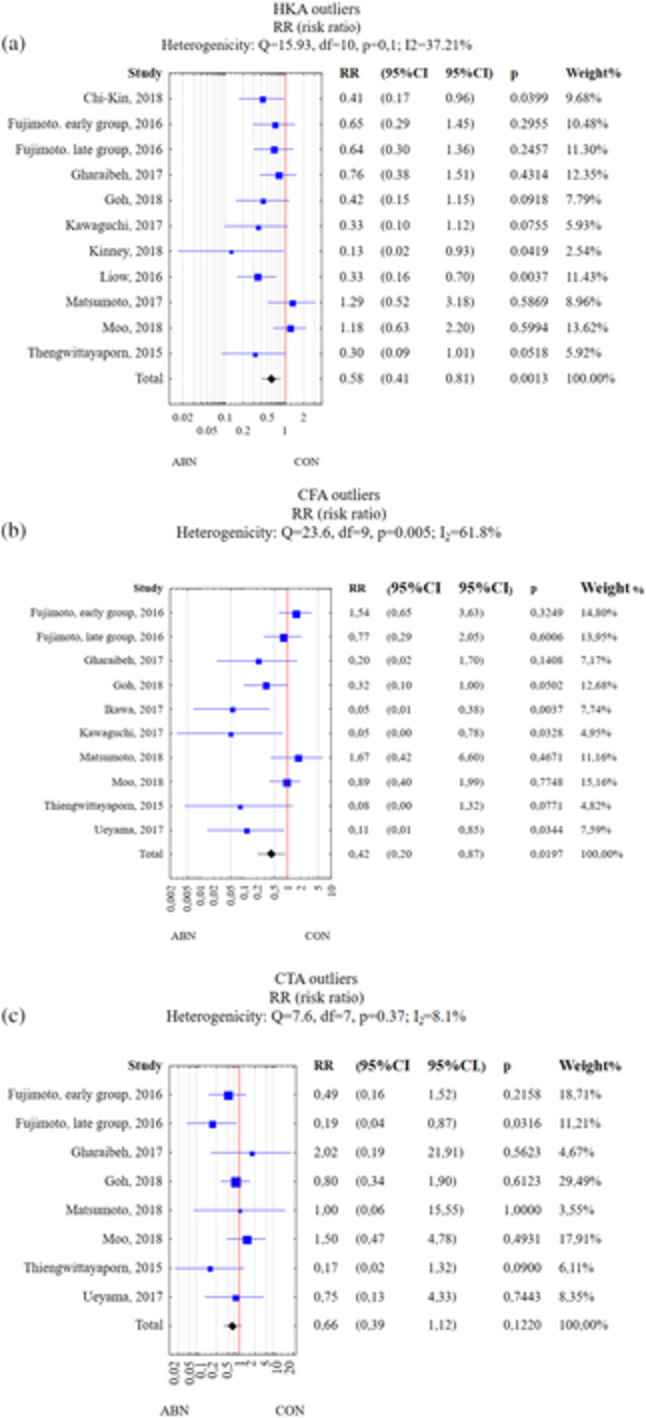
ORTHOPAEDIC SURGERY
Early surgical complications of total hip arthroplasty related to surgical approach
- Pages: 2050-2055
- First Published: 20 July 2020
A 10-year retrospective review of prospectively recorded data extracted from a single hospital registry was performed to compare the incidence of early surgical complications in total hip arthroplasty related to approach. No approach was associated with the primary outcome measure of return to theatre in 1 year on unadjusted analyses or multivariate modelling.
Does well-controlled overt hypothyroidism increase the risk of total knee arthroplasty?
- Pages: 2056-2060
- First Published: 31 July 2020
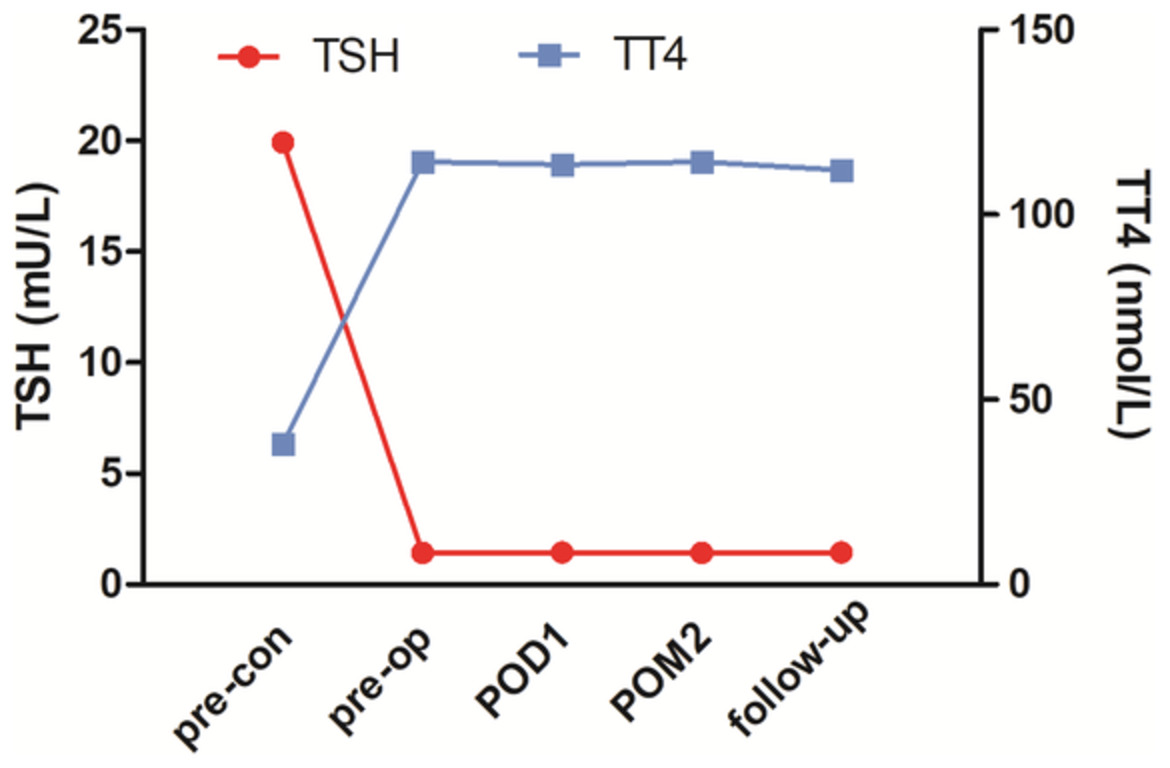
By comparing reversed hypothyroid patients with euthyroid patients, we found well-controlled overt hypothyroidism did not increase the risk of total knee arthroplasty (TKA), except for perioperative blood loss. Surgeons should be aware that even if hypothyroidism is reversed, the risk of more perioperative blood loss still exists and consequently, perioperative blood management is still essential in this population.
Survivorship of highly constrained prostheses in primary and revision total knee arthroplasty: analysis of 6070 cases
- Pages: 2061-2067
- First Published: 19 August 2020
Handheld, accelerometer-based navigation versus conventional instrumentation in total knee arthroplasty: a meta-analysis
- Pages: 2068-2079
- First Published: 01 June 2020
The use of accelerometer-based navigation in total knee arthroplasties in the treatment of osteoarthritis for the restoration of alignment with increased precision and accuracy. Accelerometer-based navigation provides a suitable alternative to computer-assisted surgery and patient-specific instrumentation while maintaining a similar feel and feedback to conventional systems. In addition, there are limited increases in operative times without compromise of blood loss, complications or functional outcomes to date in the published literature.
HOW TO DO IT
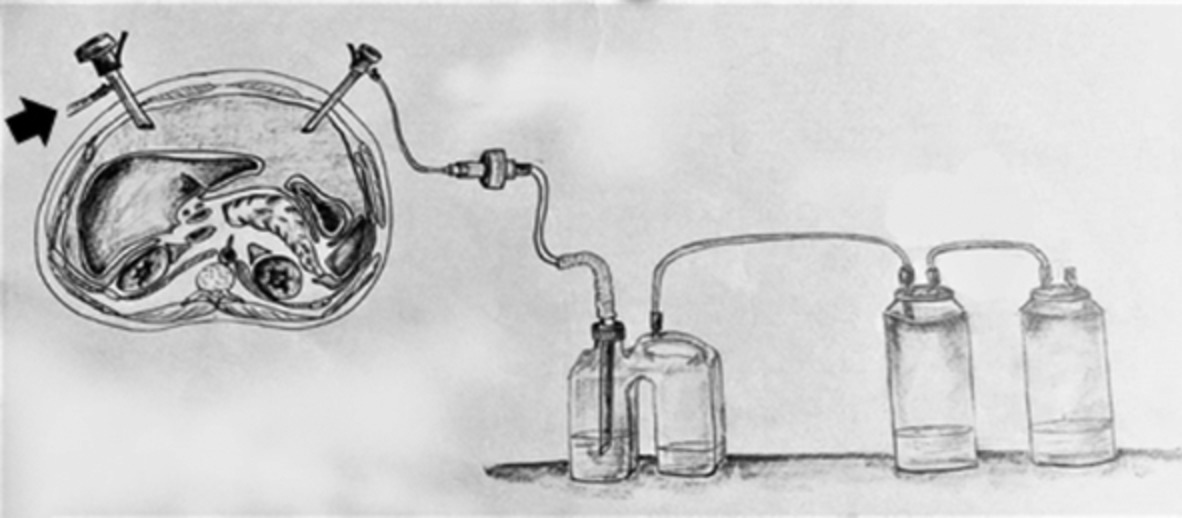
How to prevent uncontrolled abdominal desufflation during laparoscopy in times of the coronavirus pandemic
- Pages: 2080-2081
- First Published: 16 August 2020
How to do liver transplantation using liver allografts with damaged supra-hepatic inferior vena cava
- Pages: 2082-2083
- First Published: 09 September 2020

During deceased donor procurement, the heart procurement team may cut the supra-hepatic inferior vena cava (IVC) too close to the liver surface, depriving the liver allograft from having enough supra-hepatic IVC to perform the anastomosis with the recipient's IVC or hepatic veins. In such instances, liver grafts usually are deemed as non-appropriate for transplantation, being discarded. Here we report a technique for reconstruction of damaged supra-hepatic IVCs through the use of a segment of the infra-hepatic IVC of the liver graft.
PROFESSIONAL SKILLS FOR SURGEONS
Advocacy for global surgery: a Pacific perspective
- Pages: 2084-2089
- First Published: 01 June 2020
IMAGES FOR SURGEONS
Appendix intussusception: a challenging differential diagnosis
- Pages: 2090-2091
- First Published: 25 January 2020
Left-sided tubo-ovarian abscess mimicking appendicitis: a diagnostic dilemma
- Pages: 2092-2093
- First Published: 20 February 2020
Extra-pulmonary tuberculosis mimicking appendicitis
- Pages: 2093-2095
- First Published: 08 June 2020
Invasive amoebiasis: an unlikely mimic of appendicitis
- Pages: 2095-2097
- First Published: 15 May 2020
Migrating Filshie clip: a possible rare cause of appendicitis
- Pages: 2097-2098
- First Published: 18 March 2020
Appendicular mass: a rare form of Yersinia pseudotuberculosis
- Pages: 2098-2100
- First Published: 03 July 2020
Irreducible inguinal hernia and acute appendicitis: a case of Amyand's hernia
- Pages: 2100-2101
- First Published: 17 July 2020
Case report: acute left-sided Amyand's hernia in an elderly patient
- Pages: 2101-2103
- First Published: 04 June 2020
Missing appendix: case of complete appendiceal intussusception secondary to endometriosis
- Pages: 2103-2104
- First Published: 27 June 2020
Wolf in sheep's clothing: a case of mistaken identity – appendiceal mucinous neoplasm
- Pages: 2105-2106
- First Published: 05 June 2020
Incarceration of a Meckel's diverticulum by jejunal diverticulosis: an atypical cause of small bowel obstruction
- Pages: 2107-2108
- First Published: 02 June 2020
Rare case of Meckel's diverticulum neuroendocrine tumour
- Pages: 2108-2110
- First Published: 30 August 2020
Phlegmonous enteritis: a cause for acute abdomen with unusual findings
- Pages: 2111-2112
- First Published: 27 February 2020
Rare case of necrotizing infection of ileal conduit
- Pages: 2112-2114
- First Published: 22 January 2020
Fibrolamellar hepatocellular carcinoma with paraneoplastic neuropsychiatric manifestations
- Pages: 2114-2115
- First Published: 22 January 2020
Unusual cause of arterial enhancing liver tumour
- Pages: 2116-2117
- First Published: 28 January 2020
Reactivated cutaneous tuberculosis presenting as an abscess
- Pages: 2117-2119
- First Published: 27 February 2020
Haemobilia from a ruptured hepatic pseudoaneurysm: a rare outcome of gangrenous cholecystitis
- Pages: 2119-2120
- First Published: 13 February 2020
Rare ‘kettle of fish’ in the management of foreign body ingestion: 834 fish hooks
- Pages: 2122-2123
- First Published: 08 February 2020
Laparoscopic splenectomy for a wandering spleen with resultant splenomegaly and gastric varices
- Pages: 2124-2125
- First Published: 04 February 2020
Delayed Haemorrhage Following Pelvic Side Wall Excision With Internal Iliac Vessel Resection in Locally Recurrent Rectal Cancer
- Pages: 2125-2127
- First Published: 28 January 2020
Delayed mesh infection presenting as an abdominal mass after laparoscopic inguinal hernia repair
- Pages: 2127-2129
- First Published: 06 February 2020
Rare case of cervical colorectal cancer metastasis
- Pages: 2129-2131
- First Published: 11 February 2020
Anterior prostatectomy for the excision of bladder paraganglioma with prostatic invasion: a unique case of partial prostatectomy
- Pages: 2131-2133
- First Published: 25 February 2020
Acute gastric dilation and necrosis from binge eating in anorexia nervosa
- Pages: 2133-2135
- First Published: 25 February 2020
Gastric outlet obstruction due to a parastomal hernia: case report of a robotic-assisted laparoscopic surgery and literature review
- Pages: 2135-2136
- First Published: 26 February 2020
Laparoscopic high anterior resection for unicentric Castleman's disease of the sigmoid mesocolon
- Pages: 2137-2138
- First Published: 02 March 2020
Submuscular pilonidal cyst: a rare presentation of late recurrence of pilonidal disease
- Pages: 2139-2140
- First Published: 04 March 2020
Ossification of the superficial radial nerve causing pain: an unusual case of progressive osseous heteroplasia
- Pages: 2140-2142
- First Published: 03 March 2020
LETTERS TO THE EDITOR
Maintaining the quality standard of oncological thoracic surgery unit activity during the COVID-19 pandemic: experience of no COVID-19 hospital
- Page: 2143
- First Published: 29 August 2020
Re: On the frontiers of change: breast surgeons' views on demarcation between surgical subspecialities in Australia
- Pages: 2143-2144
- First Published: 13 October 2020
Appendiceal intussusception secondary to hamartomatous polyps of Peutz–Jegher syndrome
- Pages: 2144-2145
- First Published: 13 October 2020
Appendicectomy, intra-abdominal abscess, percutaneous drainage and non-operative management
- Pages: 2145-2146
- First Published: 13 October 2020
Endoscopy is important in the management of jejunogastric or jejunojejunogastric intussusception
- Page: 2146
- First Published: 13 October 2020
Patient's preference should be given importance while deciding procedure to treat pilonidal sinus disease
- Pages: 2146-2148
- First Published: 13 October 2020
Re: Indeterminate liver lesions – a virtual epidemic: a cohort study over 8 years
- Page: 2148
- First Published: 13 October 2020