Clinical and histological findings of autosomal dominant renal-limited disease with LMX1B mutation
Abstract
Aim
Mutations of LMX1B cause nail-patella syndrome, a rare autosomal dominant disorder. Recently, LMX1B R246Q heterozygous mutations were recognised in nephropathy without extrarenal manifestation. The aim of this study was to clarify characteristics of nephropathy caused by R246Q mutation.
Methods
Whole exome sequencing was performed on a large family with nonsyndromic autosomal dominant nephropathy without extrarenal manifestation. Clinical and histological findings of patients with LMX1B mutation were investigated.
Results
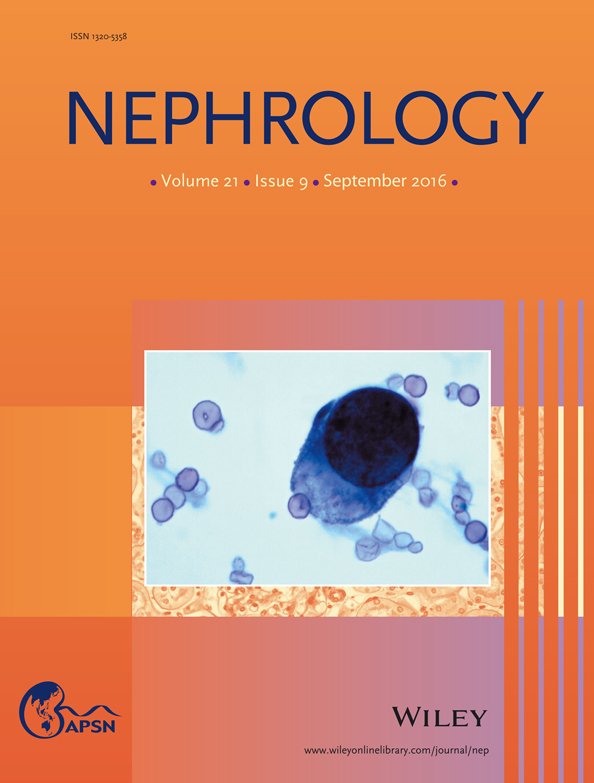
LMX1B R246Q heterozygous mutation was identified in five patients over three generations. Proteinuria or haematoproteinuria was recognized by urinary screening from all patients in childhood. Proteinuria gradually increased to nephrotic levels and renal function decreased in adolescence. Two patients progressed to end-stage renal disease in adulthood. Renal histology demonstrated minimal change in childhood and focal segmental glomerulosclerosis in adulthood. Using electron microscopy, focal collagen deposition could be detected in glomeruli even when a “moth-eaten appearance” was not apparent in the glomerular basement membrane. In addition, podocin expression in glomerular podocytes was significantly decreased, even in the early stages of disease progression.
Conclusion
Comprehensive genetic analyses and collagen or tannic acid staining may be useful for diagnosis of LMX1B-associated nephropathy. While renal prognosis of R246Q may be worse than that of typical NPS nephropathy, signs of podocytopathy can be detected during the infantile period; thus, childhood urinary screening may facilitate early detection.