Female sex and advanced age are associated with invasive cytomegalovirus disease in solid organ transplant recipients
Corresponding Author
Whitney A. Perry
Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, Boston, Massachusetts, USA
Correspondence
Whitney Perry, Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, 800 Washington Street, Box #238, Boston, MA 02111, USA.
Email: [email protected]
Search for more papers by this authorBradley J. Gardiner
Department of Infectious Disease, Alfred Health and Central Clinical School, Monash University, Melbourne, Victoria, Australia
Search for more papers by this authorLori Lyn Price
The Institute for Clinical and Health Research Policy Studies (ICRHPS), Tufts Medical Center, Boston, Massachusetts, USA
Tufts Clinical and Translational Science Institute, Tufts University, Boston, Massachusetts, USA
Search for more papers by this authorMarta Rodriguez-Garcia
Department of Immunology, Tufts University School of Medicine, Boston, Massachusetts, USA
Search for more papers by this authorJennifer K. Chow
Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, Boston, Massachusetts, USA
Search for more papers by this authorDavid R. Snydman
Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, Boston, Massachusetts, USA
Search for more papers by this authorCorresponding Author
Whitney A. Perry
Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, Boston, Massachusetts, USA
Correspondence
Whitney Perry, Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, 800 Washington Street, Box #238, Boston, MA 02111, USA.
Email: [email protected]
Search for more papers by this authorBradley J. Gardiner
Department of Infectious Disease, Alfred Health and Central Clinical School, Monash University, Melbourne, Victoria, Australia
Search for more papers by this authorLori Lyn Price
The Institute for Clinical and Health Research Policy Studies (ICRHPS), Tufts Medical Center, Boston, Massachusetts, USA
Tufts Clinical and Translational Science Institute, Tufts University, Boston, Massachusetts, USA
Search for more papers by this authorMarta Rodriguez-Garcia
Department of Immunology, Tufts University School of Medicine, Boston, Massachusetts, USA
Search for more papers by this authorJennifer K. Chow
Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, Boston, Massachusetts, USA
Search for more papers by this authorDavid R. Snydman
Division of Geographic Medicine and Infectious Diseases, Tufts Medical Center, Boston, Massachusetts, USA
Search for more papers by this authorAbstract
Background
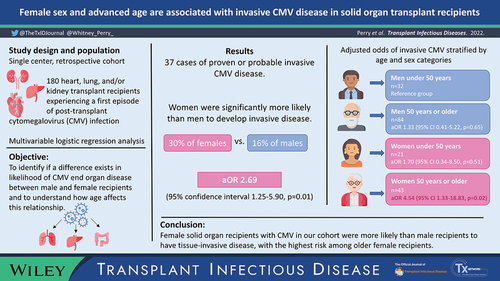
Limited data exist to describe sex-based differences in the severity of cytomegalovirus (CMV) infection after solid organ transplant (SOT). We sought to identify if a difference exists in likelihood of tissue-invasive disease between male and female SOT recipients and to understand how age affects this relationship.
Methods
A retrospective cohort of 180 heart, liver, and kidney recipients treated for CMV was examined. A logistic regression model was developed to assess the relationship between female sex and CMV type (noninvasive vs. invasive). A secondary regression analysis looked at the relationship of invasive CMV with a variable combining sex with age above or below 50.
Results
There were 37 cases of proven or probable invasive CMV, occurring in 30% of females versus 16% of males. After adjustment for potential confounders, females with CMV infection were significantly more likely to have invasive disease (odds ratio (OR) 2.69, 95% confidence interval (CI) 1.25–5.90, p = .01). Females 50 years or older were at particular risk compared with males under 50 years (adjusted OR 4.54, 95% CI 1.33–18.83, p = .02).
Conclusion
CONFLICT OF INTEREST
D.R.S. reports Merck research grant funding and consultation (Endpoint committee), Takeda research grant funding and consultation (Endpoint committee Chair), and Symbio consultation (Data Safety Monitoring Board). J.K.C reports Merck and Takeda research grant funding. B.G. reports institutional research funding from Takeda.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available upon reasonable request from the corresponding author.
Supporting Information
| Filename | Description |
|---|---|
| tid13960-sup-0001-SuppMat.docx13.4 KB | Supporting Material |
| tid13960-sup-0002-Visual-Abstract.TIF2.2 MB | Visual Abstract |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Freeman RB. The ‘indirect’ effects of cytomegalovirus infection. Am J Transplant. 2009; 9(11): 2453-2458. https://doi.org/10.1111/j.1600-6143.2009.02824.x
- 2Gardiner BJ, Chow JK, Brilleman SL, Peleg AY, Snydman DR. The impact of recurrent cytomegalovirus infection on long-term survival in solid organ transplant recipients. Transpl Infect Dis. 2019; 21(6):e13189. https://doi.org/10.1111/tid.13189
- 3Leeaphorn N, Garg N, Thamcharoen N, Khankin EV, Cardarelli F, Pavlakis M. Cytomegalovirus mismatch still negatively affects patient and graft survival in the era of routine prophylactic and preemptive therapy: a paired kidney analysis. Am J Transplant. 2019; 19(2): 573-584. https://doi.org/10.1111/ajt.15183
- 4Reischig T, Jindra P, Svecová M, Kormunda S, Opatrný K, Treska V. The impact of cytomegalovirus disease and asymptomatic infection on acute renal allograft rejection. J Clin Virol. 2006; 36(2): 146-151. https://doi.org/10.1016/j.jcv.2006.01.015
- 5Sagedal S, Nordal KP, Hartmann A, et al. The impact of cytomegalovirus infection and disease on rejection episodes in renal allograft recipients. Am J Transplant. 2002; 2(9): 850-856. https://doi.org/10.1034/j.1600-6143.2002.20907.x
- 6Sobieszczańska-Małek M, Korewicki J, Komuda K, et al. Heart transplantation and risk of cardiac vasculopathy development: what factors are important? Ann Transplant. 2017; 22: 682-688. 10.12659/aot.905267
- 7Johansson I, Andersson R, Friman V, et al. Cytomegalovirus infection and disease reduce 10-year cardiac allograft vasculopathy-free survival in heart transplant recipients. BMC Infect Dis. 2015; 15: 582. https://doi.org/10.1186/s12879-015-1321-1
- 8Freeman RB, Paya C, Pescovitz MD, et al. Risk factors for cytomegalovirus viremia and disease developing after prophylaxis in high-risk solid-organ transplant recipients. Transplantation. 2004; 78(12): 1765-1773. https://doi.org/10.1097/01.tp.0000142619.01510.a5
- 9Ghosh S, Klein RS. Sex drives dimorphic immune responses to viral infections. J Immunol. 2017; 198(5): 1782-1790. https://doi.org/10.4049/jimmunol.1601166
- 10Klein SL. Sex influences immune responses to viruses, and efficacy of prophylaxis and treatments for viral diseases. Bioessays. 2012; 34(12): 1050-1059. https://doi.org/10.1002/bies.201200099
- 11Ford ML, Mannon RB. Time for increased awareness of sex as a biological variable in transplantation. Am J Transplant. 2021; 21(10): 3215-3216. https://doi.org/10.1111/ajt.16733
- 12Melk A, Babitsch B, Borchert-Mörlins B, et al. Equally interchangeable? How sex and gender affect transplantation. Transplantation. 2019; 103(6): 1094-1110. https://doi.org/10.1097/TP.0000000000002655
- 13Hickey KT, Doering LV, Chen B, et al. Clinical and gender differences in heart transplant recipients in the NEW HEART study. Eur J Cardiovasc Nurs. 2017; 16(3): 222-229. https://doi.org/10.1177/1474515116651178
- 14Sawinski D, Goral S. BK virus infection: an update on diagnosis and treatment. Nephrol Dial Transplant. 2015; 30(2): 209-217. https://doi.org/10.1093/ndt/gfu023
- 15Lau A, West L, Tullius SG. The impact of sex on alloimmunity. Trends Immunol. 2018; 39(5): 407-418. https://doi.org/10.1016/j.it.2018.01.008
- 16Maenosono R, Nian Y, Iske J, et al. Recipient sex and estradiol levels affect transplant outcomes in an age-specific fashion. Am J Transplant. 2021; 21(10): 3239-3255.https://doi.org/10.1111/ajt.16611
- 17Ljungman P, Boeckh M, Hirsch HH, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. 2017; 64(1): 87-91. https://doi.org/10.1093/cid/ciw668
- 18Gardiner BJ, Chow JK, Price LL, Nierenberg NE, Kent DM, Snydman DR. Role of secondary prophylaxis with valganciclovir in the prevention of recurrent cytomegalovirus disease in solid organ transplant recipients. Clin Infect Dis. 2017; 65(12): 2000-2007. https://doi.org/10.1093/cid/cix696
- 19Gardiner BJ, Nierenberg NE, Chow JK, Ruthazer R, Kent DM, Snydman DR. Absolute lymphocyte count: a predictor of recurrent cytomegalovirus disease in solid organ transplant recipients. Clin Infect Dis. 2018; 67(9): 1395-1402. https://doi.org/10.1093/cid/ciy295
- 20Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150(9): 604-612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
- 21 Genentech. Cytovene (ganciclovir) package insert. Genentech; 2016.
- 22 Genentech. Valcyte (valganciclovir) package insert. Genentech; 2017.
- 23Kotton CN, Kumar D, Caliendo AM, et al. The third international consensus guidelines on the management of cytomegalovirus in solid-organ transplantation. Transplantation. 2018; 102(6): 900-931. https://doi.org/10.1097/TP.0000000000002191
- 24Snydman DR, Werner BG, Heinze-Lacey B, et al. Use of cytomegalovirus immune globulin to prevent cytomegalovirus disease in renal-transplant recipients. N Engl J Med. 1987; 317(17): 1049-1054. https://doi.org/10.1056/NEJM198710223171703
- 25Snydman DR, Werner BG, Dougherty NN, et al. Cytomegalovirus immune globulin prophylaxis in liver transplantation. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1993; 119(10): 984-891. https://doi.org/10.7326/0003-4819-119-10-199311150-00004
- 26Atabani SF, Smith C, Atkinson C, et al. Cytomegalovirus replication kinetics in solid organ transplant recipients managed by preemptive therapy. Am J Transplant. 2012; 12(9): 2457-2464. https://doi.org/10.1111/j.1600-6143.2012.04087.x
- 27Santos CA, Brennan DC, Fraser VJ, Olsen MA. Incidence, risk factors, and outcomes of delayed-onset cytomegalovirus disease in a large, retrospective cohort of heart transplant recipients. Transplant Proc. 2014; 46(10): 3585-3592. https://doi.org/10.1016/j.transproceed.2014.08.043
- 28McBride JM, Sheinson D, Jiang J, et al. Correlation of cytomegalovirus (CMV) disease severity and mortality with CMV viral burden in CMV-seropositive donor and CMV-seronegative solid organ transplant recipients. Open Forum Infect Dis. 2019; 6(2):ofz003. https://doi.org/10.1093/ofid/ofz003
- 29Alfieri CM, Molinari P, Gandolfo M, et al. Cytomegalovirus disease in renal transplanted patients: prevalence, determining factors, and influence on graft and patients outcomes. Pathogens. 2021; 10(4): 473. https://doi.org/10.3390/pathogens10040473
- 30Hernandez C, Mabilangan C, Burton C, Doucette K, Preiksaitis J. Cytomegalovirus transmission in mismatched solid organ transplant recipients: are factors other than anti-viral prophylaxis at play? Am J Transplant. 2021; 21(12): 3958-3970. https://doi.org/10.1111/ajt.16734
- 31Arthurs SK, Eid AJ, Pedersen RA, et al. Delayed-onset primary cytomegalovirus disease after liver transplantation. Liver Transpl. 2007; 13(12): 1703-1709. https://doi.org/10.1002/lt.21280
- 32Viot B, Garrigue I, Taton B, et al. Two-year post-transplantation cytomegalovirus DNAemia in asymptomatic kidney transplant recipients: incidence, risk factors, and outcome. Transpl Infect Dis. Aug 2015; 17(4): 497-509. https://doi.org/10.1111/tid.12408
- 33Chemaly RF, El Haddad L, Winston DJ, et al. Cytomegalovirus (CMV) cell-mediated immunity and CMV infection after allogeneic hematopoietic cell transplantation: the REACT study. Clin Infect Dis. 2020; 71(9): 2365-2374. https://doi.org/10.1093/cid/ciz1210
- 34da Cunha-Bang C, Sørensen SS, Iversen M, et al. Factors associated with the development of cytomegalovirus infection following solid organ transplantation. Scand J Infect Dis. 2011; 43(5): 360-365. https://doi.org/10.3109/00365548.2010.549836
- 35Nuansri S, Kantachuvesiri S, Watcharananan SP, Thongprayoon C, Cheungpasitporn W, Bruminhent J. Clinical characteristics of late-onset cytomegalovirus infection after kidney transplantation. Transplant Proc. 2021; 53(7): 2267-2271. https://doi.org/10.1016/j.transproceed.2021.07.033
- 36Blyth D, Lee I, Sims KD, et al. Risk factors and clinical outcomes of cytomegalovirus disease occurring more than one year post solid organ transplantation. Transpl Infect Dis. 2012; 14(2): 149-155. https://doi.org/10.1111/j.1399-3062.2011.00705.x
- 37Meije Y, Fortún J, Len Ó, et al. Prevention strategies for cytomegalovirus disease and long-term outcomes in the high-risk transplant patient (D+/R-): experience from the RESITRA-REIPI cohort. Transpl Infect Dis. 2014; 16(3): 387-396. https://doi.org/10.1111/tid.12226
- 38Manuel O, Kralidis G, Mueller NJ, et al. Impact of antiviral preventive strategies on the incidence and outcomes of cytomegalovirus disease in solid organ transplant recipients. Am J Transplant. 2013; 13(9): 2402-2410. https://doi.org/10.1111/ajt.12388
- 39Klein SL, Jedlicka A, Pekosz A. The Xs and Y of immune responses to viral vaccines. Lancet Infect Dis. 2010; 10(5): 338-349. https://doi.org/10.1016/S1473-3099(10)70049-9
- 40Limaye AP, Kirby KA, Rubenfeld GD, et al. Cytomegalovirus reactivation in critically ill immunocompetent patients. JAMA. 2008; 300(4): 413-422. https://doi.org/10.1001/jama.300.4.413
- 41Villacres MC, Longmate J, Auge C, Diamond DJ. Predominant type 1 CMV-specific memory T-helper response in humans: evidence for gender differences in cytokine secretion. Hum Immunol. 2004; 65(5): 476-485. https://doi.org/10.1016/j.humimm.2004.02.021
- 42Di Benedetto S, Derhovanessian E, Steinhagen-Thiessen E, Goldeck D, Müller L, Pawelec G. Impact of age, sex and CMV-infection on peripheral T cell phenotypes: results from the Berlin BASE-II Study. Biogerontology. 2015; 16(5): 631-643. https://doi.org/10.1007/s10522-015-9563-2
- 43Zhu J, Shearer GM, Norman JE, et al. Host response to cytomegalovirus infection as a determinant of susceptibility to coronary artery disease: sex-based differences in inflammation and type of immune response. Circulation. 2000; 102(20): 2491-2496. https://doi.org/10.1161/01.cir.102.20.2491
- 44Perrottet N, Csajka C, Pascual M, et al. Population pharmacokinetics of ganciclovir in solid-organ transplant recipients receiving oral valganciclovir. Antimicrob Agents Chemother. 2009; 53(7): 3017-3023. https://doi.org/10.1128/AAC.00836-08
- 45Hwang J, Purdy JG, Wu K, Rabinowitz JD, Shenk T. Estrogen-related receptor α is required for efficient human cytomegalovirus replication. Proc Natl Acad Sci U S A. 2014; 111(52): E5706-E5715. https://doi.org/10.1073/pnas.1422361112
- 46Lindemann M, Korth J, Sun M, et al. The cytomegalovirus-specific IL-21 ELISpot correlates with allograft function of kidney transplant recipients. Int J Mol Sci. 2018; 19(12): 08. doi:https://doi.org/10.3390/ijms19123945
- 47Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016; 16(10): 626-638. https://doi.org/10.1038/nri.2016.90
- 48Meesing A, Abraham RS, Razonable RR. Clinical correlation of cytomegalovirus infection with CMV-specific CD8+ T-cell immune competence score and lymphocyte subsets in solid organ transplant recipients. Transplantation. 2019; 103(4): 832-838. https://doi.org/10.1097/TP.0000000000002396
- 49Higdon LE, Trofe-Clark J, Liu S, et al. Cytomegalovirus-responsive CD8. Am J Transplant. 2017; 17(8): 2045-2054. https://doi.org/10.1111/ajt.14227
- 50Jorgenson MR, Kleiboeker H, Garg N, et al. Letermovir conversion after valganciclovir treatment in cytomegalovirus high-risk abdominal solid organ transplant recipients may promote development of cytomegalovirus-specific cell mediated immunity. Transpl Infect Dis. 2022; 24(1):e13766. https://doi.org/10.1111/tid.13766
- 51Abu-Omar A, Sester M. Ways to boost cellular immunity in solid organ transplant recipients - the case of letermovir. Transpl Infect Dis. 2022; 24(1):e13787. https://doi.org/10.1111/tid.13787