Incidence, risk factors, outcomes, and clinical management of BK viremia in the modern era of kidney transplantation
Denis Qeska
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorRebecca Bic Kay Wong
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorOlusegun Famure
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Division of Nephrology, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorYanhong Li
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorHilary Pang
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorXin Yun Liang
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorMary Parker Zhu
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorCorresponding Author
Shahid Husain
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Department of Medicine, University of Toronto, Toronto, Ontario, Canada
Division of Infectious Diseases, University Health Network, Toronto, Ontario, Canada
Correspondence
Shahid Husain, Infectious Diseases Specialist, Director of Research, Ajmera Transplant Centre, University Health Network, 585 University Ave, MaRS building, Suite 9-9080, Toronto ON M5G 2N2, Canada.
Email: [email protected]
Search for more papers by this authorSang Joseph Kim
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Division of Nephrology, University Health Network, Toronto, Ontario, Canada
Department of Medicine, University of Toronto, Toronto, Ontario, Canada
Search for more papers by this authorDenis Qeska
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorRebecca Bic Kay Wong
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorOlusegun Famure
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Division of Nephrology, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorYanhong Li
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorHilary Pang
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorXin Yun Liang
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorMary Parker Zhu
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Search for more papers by this authorCorresponding Author
Shahid Husain
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Department of Medicine, University of Toronto, Toronto, Ontario, Canada
Division of Infectious Diseases, University Health Network, Toronto, Ontario, Canada
Correspondence
Shahid Husain, Infectious Diseases Specialist, Director of Research, Ajmera Transplant Centre, University Health Network, 585 University Ave, MaRS building, Suite 9-9080, Toronto ON M5G 2N2, Canada.
Email: [email protected]
Search for more papers by this authorSang Joseph Kim
Kidney Transplant Program, Toronto General Hospital, University Health Network, Toronto, Ontario, Canada
Division of Nephrology, University Health Network, Toronto, Ontario, Canada
Department of Medicine, University of Toronto, Toronto, Ontario, Canada
Search for more papers by this authorQeska and Wong contributed equally to this work.
Husain and Kim are co-senior authors of this work.
Abstract
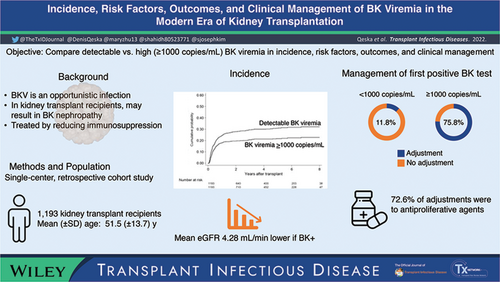
BK viremia is endemic among kidney transplant recipients (KTRs). Incidence, risk factors, outcomes, and clinical
management of detectable versus high BK viremia have not been considered previously in KTR in the modern era. This observational study examined KTR transplanted between January 1, 2009 and December 31, 2016. Any BK viral load in the serum constituted detectable BK viremia and ≥103 copies/ml constituted high viremia. Among 1193 KTRs, the cumulative probability of developing detectable and high BK viremia within 2 years posttransplant were 27.8% and 19.6%, respectively. Significant risk factors for detectable BK viremia included recipient age (HR 1.02 [95% CI: 1.01, 1.03]) and donor age (HR 1.01 [95% CI: 1.00, 1.02]). Recipient age also predicted high BK viremia (HR 1.02 [95% CI: 1.01, 1.03]), whereas White race (HR 0.70 [95% CI: 0.52, 0.95]), nondepleting induction therapy (HR 0.61 [95% CI: 0.42, 0.89]), and delayed graft function (HR 0.61 [95% CI: 0.42, 0.88]) were protective. Mean estimated glomerular filtration rates were 4.28 ml/min/1.72 m2 (95% CI: 2.71, 5.84) lower with detectable BK viremia. Although low viral load was usually not acted upon at first presentation, antiproliferative dose reductions were the most common initial management. BK viremia remains a common early complication in a modern cohort of KTRs. These findings highlight the benefit of early BKV monitoring in addition to intensive clinical management. Clinical responses beyond first positive BK viremia tests, and their implications for graft outcomes, merit further investigation.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Supporting Information
| Filename | Description |
|---|---|
| tid13915-sup-0001-FigureS1.docx19.8 KB | Figure S1: Study population flow diagram for all adult kidney transplant recipients transplanted between January 1, 2009 and December 21, 2016. |
| tid13915-sup-0002-FigureS2.docx170.9 KB | Figure S2: The cumulative probabilities of developing (A) any first positive BK test and (B) the first BK test with viral load ≥103 copies/ml over 8 years posttransplant. |
| tid13915-sup-0003-TableS1-S8.docx45.5 KB | Table S1: Baseline recipient, donor, and transplant characteristics for the study cohort at 30 days posttransplant. Table S2: The number of events, follow-up times, and incidence rates for studied outcomes of BK viremia, death-censored graft failure, death with graft function, and total graft failure. Table S3: Univariable Cox regression models of the risk factors for testing BK positive and for developing a BK viral load ≥103 copies/ml. Table S4: Acute rejection did not significantly predict risk of any BK viremia or BK viral load ≥103 copies/ml when incorporated as a time-varying covariate in multivariable Cox regression models in this sensitivity analysis. Table S5: Degree of initial clinician response to positive BK tests, separated by level of viral load in first positive BK test. Table S6: Univariable Cox regression models for immunosuppressant adjustment in response to the first BK viremia test as a risk factor for first rejection or BK virus-associated nephropathy (BKVAN). Table S7: Univariable and multivariable stepwise Cox proportional hazard ratios for clinical outcomes of death-censored graft failure, death with graft function, and total graft failure, with (A) any BK positive test or (B) BK viral load ≥103 copies/ml as risk factors (other risk factors not shown). Table S8: Mixed linear regression models for effect of (A) any positive BK test or (B) BK viral load ≥103 copies/ml on mean estimated glomerular filtration rate (eGFR) at 1, 3, 6, 12, and 24 months posttransplant. |
| tid13915-sup-0004-Methods.docx14.6 KB | Supplementary methods |
| tid13915-sup-0005-VisualAbstract.pptx3.6 MB | Graphical Abstract |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Schold JD, Rehman S, Kayle LK, Magliocca J, Srinivas TR, Meier-Kriesche H-U. Treatment for BK virus: incidence, risk factors and outcomes for kidney transplant recipients in the United States. Transpl Int. 2009; 22(6): 626-634. https://doi.org/10.1111/j.1432-2277.2009.00842.x
- 2Hassan S, Mittal C, Amer S, et al. Currently recommended BK virus (BKV) plasma viral load cutoff of >= 4 log10/mL underestimates the diagnosis of BKV-associated nephropathy: a single transplant center experience. Transpl Infect Dis. 2014; 16(1): 55-60. https://doi.org/10.1111/tid.12164
- 3Blazquez-Navarro A, Dang-Heine C, Wittenbrink N, et al. BKV, CMV, and EBV interactions and their effect on graft function one year post-renal transplantation: results from a large multi-centre study. EBioMedicine. 2018; 34: 113-121. https://doi.org/10.1016/j.ebiom.2018.07.017
- 4Sawinski D, Goral S. BK virus infection: an update on diagnosis and treatment. Nephrol Dial Transplant. 2015; 30(2): 209-217. https://doi.org/10.1093/ndt/gfu023
- 5Hirsch HH, Brennan DC, Drachenberg CB, et al. Polyomavirus-associated nephropathy in renal transplantation: interdisciplinary analyses and recommendations. Transplantation. 2005; 79(10): 1277-1286. https://doi.org/10.1097/01.TP.0000156165.83160.09
- 6Kasiske BL, Zeier MG, Chapman JR, et al. KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney Int. 2010; 77(4): 299-311. https://doi.org/10.1038/ki.2009.377
- 7Almeras C, Vetromile F, Garrigue V, Szwarc I, Foulongne V, Mourad G. Monthly screening for BK viremia is an effective strategy to prevent BK virus nephropathy in renal transplant recipients. Transpl Infect Dis. 2011; 13(2): 101-108. https://doi.org/10.1111/j.1399-3062.2011.00619.x
- 8Elfadawy N, Flechner SM, Schold JD, et al. Transient versus persistent BK viremia and long-term outcomes after kidney and kidney-pancreas transplantation. Clin J Am Soc Nephrol. 2014; 9(3): 553-561. https://doi.org/10.2215/CJN.08420813
- 9Hertz-Tang AL, Astor BC, Mandelbrot DA, Mohamed MA, Djamali A, Parajuli S. BK viremia is not associated with adverse outcomes in the absence of BK nephropathy. Clin Transplant. 2018; 32:e13283. https://doi.org/10.1111/ctr.13283
- 10Simard-Meilleur M-C, Bodson-Clermont P, St-Louis G, et al. Stabilization of renal function after the first year of follow-up in kidney transplant recipients treated for significant BK polyomavirus infection or BK polyomavirus-associated nephropathy. Transpl Infect Dis. 2017; 19(3):e12681. https://doi.org/10.1111/tid.12681
- 11Koukoulaki M, Papadaki M, Pistolas D, et al. Effect of transient BK viremia and viruria on long-term renal allograft survival and function. Transplant Proc. 2014; 46(9): 3187-3190. https://doi.org/10.1016/j.transproceed.2014.10.028
- 12Sawinski D, Forde KA, Trofe-Clark J, et al. Persistent BK viremia does not increase intermediate-term graft loss but is associated with de novo donor-specific antibodies. J Am Soc Nephrol. 2015; 26(4): 966-975. https://doi.org/10.1681/ASN.2014010119
- 13Hassig A, Roos M, Etter A, et al. Association of BK viremia with human leukocyte antigen mismatches and acute rejection, but not with type of calcineurin inhibitor. Transpl Infect Dis. 2014; 16(1): 44-54. https://doi.org/10.1111/tid.12153
- 14Famure O, Phan NAT, Kim SJ. Health information management for research and quality assurance: the comprehensive renal transplant research information system. Healthc Manag Forum. 2014; 27(1): 30-36. https://doi.org/10.1016/j.hcmf.2013.11.002
- 15Hirsch HH, Randhawa PS. BK polyomavirus in solid organ transplantation—guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019; 33(9):e13528. https://doi.org/10.1111/ctr.13528
- 16Hasegawa M, Ito T, Saigo K, et al. Association of DNA amplification with progress of BK polyomavirus infection and nephropathy in renal transplant recipients. Transplant Proc. 2014; 46(2): 556-559. https://doi.org/10.1016/j.transproceed.2013.11.114
- 17Hirsch HH, Vincenti F, Friman S, et al. Polyomavirus BK replication in de novo kidney transplant patients receiving tacrolimus or cyclosporine: a prospective, randomized, multicenter study. Am J Transplant. 2013; 13(1): 136-145. https://doi.org/10.1111/j.1600-6143.2012.04320.x
- 18Knight RJ, Gaber LW, Patel SJ, DeVos JM, Moore LW, Gaber AO. Screening for BK viremia reduces but does not eliminate the risk of BK nephropathy: a single-center retrospective analysis. Transplantation. 2013; 95(7): 949-954. https://doi.org/10.1097/TP.0b013e31828423cd
- 19Weiss AS, Gralla J, Chan L, Klem P, Wiseman AC. Aggressive immunosuppression minimization reduces graft loss following diagnosis of BK virus-associated nephropathy: a comparison of two reduction strategies. Clin J Am Soc Nephrol. 2008; 3(6): 1812-1819. https://doi.org/10.2215/CJN.05691207
- 20Maliakkal JG, Brennan DC, Goss C, et al. Ureteral stent placement and immediate graft function are associated with increased risk of BK viremia in the first year after kidney transplantation. Transpl Int. 2017; 30(2): 153-161. https://doi.org/10.1111/tri.12888
- 21Sood P, Senanayake S, Sujeet K, et al. Lower prevalence of BK virus infection in African American renal transplant recipients: a prospective study. Transplantation. 2012; 93(3): 291-296. https://doi.org/10.1097/TP.0b013e31823ec05a
- 22Rech MA, Fleming JN, Moore CL. 25-hydroxyvitamin D deficiency and opportunistic viral infections after kidney transplant. Exp Clin Transplant. 2014; 12(2): 95-100. https://doi.org/10.6002/ect.2013.0201
- 23Cosio FG, Cattran DC. Recent advances in our understanding of recurrent primary glomerulonephritis after kidney transplantation. Kidney Int. 2017; 91(2): 304-314. https://doi.org/10.1016/j.kint.2016.08.030
- 24 Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl. 2012; 2: 139-274. https://doi.org/10.1038/kisup.2012.12
10.1038/kisup.2012.12 Google Scholar
- 25Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011; 11(11): 2279-2296. https://doi.org/10.1111/j.1600-6143.2011.03754.x
- 26Everly MJ, Briley KP, Haisch CE, et al. Racial differences in incident de novo donor-specific anti-HLA antibody among primary renal allograft recipients: results from a single center cohort study. Transpl Int. 2017; 30(6): 566-578. https://doi.org/10.1111/tri.12937
- 27Srinivas TR, Meier-Kriesche HU. Minimizing immunosuppression, an alternative approach to reducing side effects: objectives and interim result. Clin J Am Soc Nephrol. 2008; 3(SUPPL. 2): 101-116. https://doi.org/10.2215/CJN.03510807
- 28Vasudev B, Hariharan S, Hussain SA, Zhu Y-R, Bresnahan BA, Cohen EP. BK virus nephritis: risk factors, timing, and outcome in renal transplant recipients. Kidney Int. 2005; 68(4): 1834-1839. https://doi.org/10.1111/j.1523-1755.2005.00602.x
- 29Schneidewind L, Neumann T, Dräger DL, Kranz J, Hakenberg OW. Leflunomide in the treatment of BK polyomavirus associated nephropathy in kidney transplanted patients – a systematic review. Transplant Rev. 2020; 34:100565.https://doi.org/10.1016/j.trre.2020.100565