The rural–urban enigma of allergy: What can we learn from studies around the world?
Paul C. Schröder
LMU Munich, University Children's Hospital, Munich, Germany
Member of the German Center for Lung Research (DZL), Munich, Germany
Search for more papers by this authorJing Li
Department of Allergy and Clinical Immunology, State Key Laboratory of Respiratory Disease, The First Affiliated Hospital, Guangzhou Medical University, Guangzhou, China
Search for more papers by this authorGary W. K. Wong
Department of Paediatrics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong, China
Shared last authorship.Search for more papers by this authorCorresponding Author
Bianca Schaub
LMU Munich, University Children's Hospital, Munich, Germany
Member of the German Center for Lung Research (DZL), Munich, Germany
Shared last authorship.Correspondence
Bianca Schaub, University Children's Hospital Munich, Lindwurmstr. 4, Munich 80337, Germany
Tel.: +49 89 4400 57856
Fax: +49 89 4400 54764
E-mail: [email protected]
Search for more papers by this authorPaul C. Schröder
LMU Munich, University Children's Hospital, Munich, Germany
Member of the German Center for Lung Research (DZL), Munich, Germany
Search for more papers by this authorJing Li
Department of Allergy and Clinical Immunology, State Key Laboratory of Respiratory Disease, The First Affiliated Hospital, Guangzhou Medical University, Guangzhou, China
Search for more papers by this authorGary W. K. Wong
Department of Paediatrics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong, China
Shared last authorship.Search for more papers by this authorCorresponding Author
Bianca Schaub
LMU Munich, University Children's Hospital, Munich, Germany
Member of the German Center for Lung Research (DZL), Munich, Germany
Shared last authorship.Correspondence
Bianca Schaub, University Children's Hospital Munich, Lindwurmstr. 4, Munich 80337, Germany
Tel.: +49 89 4400 57856
Fax: +49 89 4400 54764
E-mail: [email protected]
Search for more papers by this authorAbstract
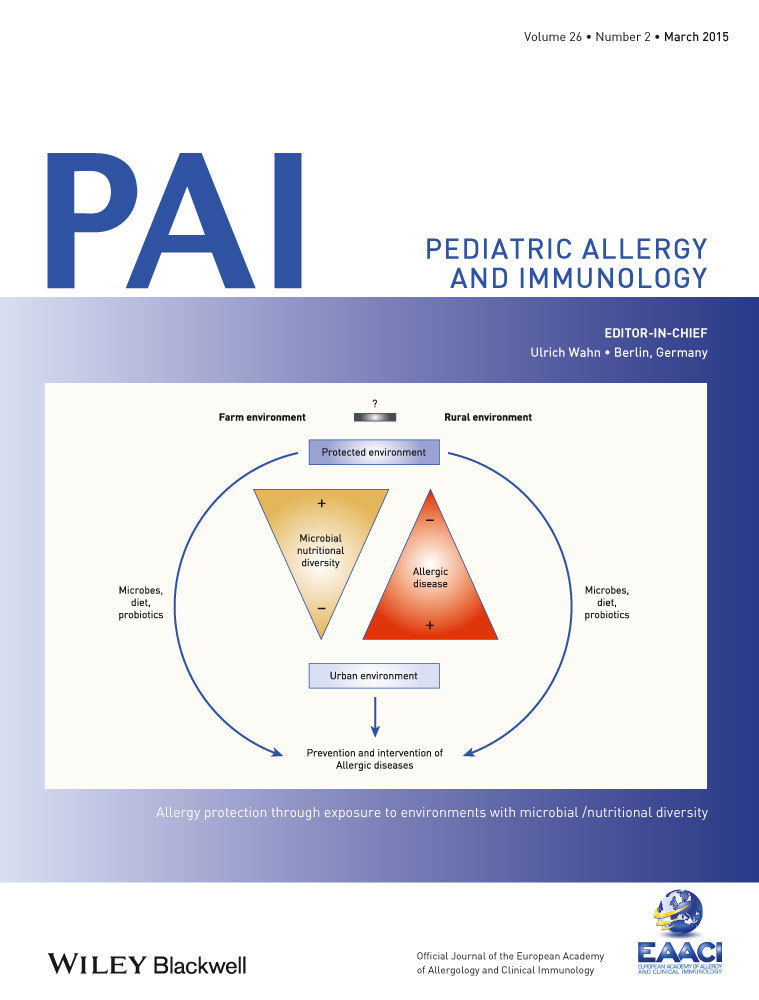
Childhood asthma and related allergic conditions have become the most common chronic disorders in the Western world. Many studies from around the world have demonstrated an increasing trend of asthma prevalence over the last few decades (Lancet, 368, 2004, 733). A few recent reports also suggested that childhood asthma prevalence may be showing a plateau or even a decline in few developed countries. Given the rapid changes in the prevalence over a short period of time, environmental factors are the more likely candidates explaining such trend. One of the most consistent epidemiological findings was that subjects living in the rural areas had lower prevalence of allergies when compared to those from urban areas (Clin Exp Allergy 30, 2000, 187; Pediatr Pulmonol 44, 2009, 793). Clear understanding of the mechanisms of how the environmental determinants in the rural environment may affect the early immune system resulting in lower risk of allergies and asthma will facilitate the development of future primary preventive strategies. In this study, we review recent data from around the world and explore the epidemiology and mechanistic studies that may explain the rural–urban difference of allergies.
References
- 1Asher MI, Montefort S, Björkstén B, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 2006: 368: 733–43.
- 2Beasley R, Ellwood P, Asher I. International patterns of the prevalence of pediatric asthma the ISAAC program. Pediatr Clin North Am 2003: 50: 539–53.
- 3Peat JK, van den Berg RH, Green WF, et al. Changing prevalence of asthma in Australian children. BMJ 1994: 308: 1591–6.
- 4Ninan TK, Russell G. Respiratory symptoms and atopy in Aberdeen schoolchildren: evidence from two surveys 25 years apart. BMJ 1992: 304: 873–5.
- 5Li J, Wang H, Chen Y, et al. House dust mite sensitization is the main risk factor for the increase in prevalence of wheeze in 13- To 14-year-old schoolchildren in guangzhou city, china. Clin Exp Allergy 2013: 43: 1171–9.
- 6Weiland SK, Von Mutius E, Hirsch T, et al. Prevalence of respiratory and atopic disorders among children in the East and West of Germany five years after unification. Eur Respir J 1999: 14: 862–70.
- 7Beasley R, Keil U, Von Mutius E, et al. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet 1998: 351: 1225–32.
- 8Wong GWK, Hui DSC, Chan HH, et al. Prevalence of respiratory and atopic disorders in Chinese schoolchildren. Clin Exp Allergy 2001: 31: 1225–31.
- 9Asher MI. Worldwide variations in the prevalence of asthma symptoms: the International Study of Asthma and Allergies in Childhood (ISAAC). Eur Respir J 1998: 12: 315–35.
- 10Wong GWK, Lai CKW. Outdoor air pollution and asthma. Curr Opin Pulm Med 2004: 10: 62–6.
- 11Anderson HR, Ruggles R, Pandey KD, et al. Ambient particulate pollution and the world-wide prevalence of asthma, rhinoconjunctivitis and eczema in children: Phase One of the International Study of Asthma and Allergies in Childhood (ISAAC). Occup Environ Med 2010: 67: 293–300.
- 12Ross Anderson HR, Butland BK, van Donkelaar A, et al. Satellite-based estimates of ambient air pollution and global variations in childhood asthma prevalence. Environ Health Perspect 2012: 120: 1333–9.
- 13Wong GWK, Brunekreef B, Ellwood P, et al. Cooking fuels and prevalence of asthma: a global analysis of phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Lancet Respir Med 2013: 1: 386–94.
- 14Custovic A. To what extent is allergen exposure a risk factor for the development of allergic disease? Clin Exp Allergy 2015: 45: 54–62.
- 15Murray CS, Poletti G, Kebadze T, et al. Study of modifiable risk factors for asthma exacerbations: virus infection and allergen exposure increase the risk of asthma hospital admissions in children. Thorax 2006: 61: 376–82.
- 16Sporik R, Holgate ST, Platts-Mills TA, et al. Exposure to house-dust mite allergen (Der p I) and the development of asthma in childhood. A prospective study. N Engl J Med 1990: 323: 502–7.
- 17Bakolis I, Heinrich J, Zock JP, et al. House dust-mite allergen exposure is associated with serum specific IgE but not with respiratory outcomes. Indoor Air 2014: doi: 10.1111/ina.12137.
- 18Lodge CJ, Allen KJ, Lowe AJ, et al. Perinatal cat and dog exposure and the risk of asthma and allergy in the urban environment: a systematic review of longitudinal studies. Clin Dev Immunol 2012: 2012: 176484.
- 19Woodcock A, Lowe LA, Murray CS, et al. Early life environmental control: effect on symptoms, sensitization, and lung function at age 3 years. Am J Respir Crit Care Med 2004: 170: 433–9.
10.1164/rccm.200401-083OC Google Scholar
- 20Strachan DP. Hay fever, hygiene, and household size. BMJ 1989: 299: 1259–60.
- 21Von Mutius E, Martinez FD, Fritzsch C, et al. Skin test reactivity and number of siblings. BMJ 1994: 308: 692–5.
- 22Ball TM, Castro-Rodriguez JA, Griffith KA, et al. Siblings, day-care attendance, and the risk of asthma and wheezing during childhood. N Engl J Med 2000: 343: 538–43.
- 23Matricardi PM, Rosmini F, Ferrigno L, et al. Cross sectional retrospective study of prevalence of atopy among Italian military students with antibodies against hepatitis A virus. BMJ 1997: 314: 999–1003.
- 24Matricardi PM, Rosmini F, Riondino S, et al. Exposure to foodborne and orofecal microbes versus airborne viruses in relation to atopy and allergic asthma: epidemiological study. BMJ 2000: 320: 412–7.
- 25Flohr C, Quinnell RJ, Britton J. Do helminth parasites protect against atopy and allergic disease? Clin Exp Allergy 2009: 39: 20–32.
- 26Van den Biggelaar AHJ, Rodrigues LC, van Ree R, et al. Long-term treatment of intestinal helminths increases mite skin-test reactivity in Gabonese schoolchildren. J Infect Dis 2004: 189: 892–900.
- 27Braun-Fahrländer C, Gassner M, Grize L, et al. Prevalence of hay fever and allergic sensitization in farmer's children and their peers living in the same rural community. Clin Exp Allergy 1999: 29: 28–34.
- 28Von Ehrenstein OS, Von Mutius E, Illi S, et al. Reduced risk of hay fever and asthma among children of farmers. Clin Exp Allergy 2000: 30: 187–93.
- 29Weinstock J. Do we need worms to promote immune health? Clin Rev Allergy Immunol 2014: doi: 10.1007/s12016-014-8458-3.
- 30Vartiainen E, Petäys T, Haahtela T, et al. Allergic diseases, skin prick test responses, and IgE levels in North Karelia, Finland, and the Republic of Karelia, Russia. J Allergy Clin Immunol 2002: 109: 643–8.
- 31Von Hertzen L, Laatikainen T, Pitkänen T, et al. Microbial content of drinking water in Finnish and Russian Karelia – Implications for atopy prevalence. Allergy 2007: 62: 288–92.
- 32Barnes M, Cullinan P, Athanasaki P, et al. Crete: does farming explain urban and rural differences in atopy? Clin Exp Allergy 2001: 31: 1822–8.
- 33Wickens K, Lane JM, Fitzharris P, et al. Farm residence and exposures and the risk of allergic diseases in New Zealand children. Allergy 2002: 57: 1171–9.
- 34Perkin MR, Strachan DP. Which aspects of the farming lifestyle explain the inverse association with childhood allergy? J Allergy Clin Immunol 2006: 117: 1374–81.
- 35Ma Y, Zhao J, Han ZR, et al. Very low prevalence of asthma and allergies in schoolchildren from rural Beijing, China. Pediatr Pulmonol 2009: 44: 793–9.
- 36Von Mutius E, Vercelli D. Farm living: effects on childhood asthma and allergy. Nat Rev Immunol 2010: 10: 861–8.
- 37Lluis A, Schaub B. Lesson from the farm environment. Curr Opin Allergy Clin Immunol 2012: 12: 158–63.
- 38Riedler J, Braun-Fahrländer C, Eder W, et al. Exposure to farming in early life and development of asthma and allergy: a cross-sectional survey. Lancet 2001: 358: 1129–33.
- 39Waser M, Michels KB, Bieli C, et al. Inverse association of farm milk consumption with asthma and allergy in rural and suburban populations across Europe. Clin Exp Allergy 2007: 37: 661–70.
- 40Braun-Fahrländer C, Riedler J, Herz U, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med 2002: 347: 869–77.
- 41Marsland BJ, Gollwitzer ES. Host-microorganism interactions in lung diseases. Nat Rev Immunol 2014: 14: 827–35.
- 42Sommer F, Backhed F. The gut microbiota – masters of host development and physiology. Nat Rev Microbiol 2013: 11: 227–38.
- 43Ege MJ, Mayer M, Normand A-C, et al. Exposure to environmental microorganisms and childhood asthma. N Engl J Med 2011: 364: 701–9.
- 44Ege MJ, Mayer M, Schwaiger K, et al. Environmental bacteria and childhood asthma. Allergy 2012: 67: 1565–71.
- 45Kim J-H, Ellwood PE, Asher MI. Diet and asthma: looking back, moving forward. Respir Res 2009: 10: 49.
- 46Loss G, Apprich S, Waser M, et al. The protective effect of farm milk consumption on childhood asthma and atopy: the GABRIELA study. J Allergy Clin Immunol 2011: 128: 766.e4–73.e4.
- 47Loss G, Depner M, Ulfman LH, et al. Consumption of unprocessed cow's milk protects infants from common respiratory infections. J Allergy Clin Immunol 2015: 135: 56–62.e2.
- 48Roduit C, Frei R, Depner M, et al. Increased food diversity in the first year of life is inversely associated with allergic diseases. J Allergy Clin Immunol 2014: 133: 1056–64.
- 49Peters M, Kauth M, Schwarze J, et al. Inhalation of stable dust extract prevents allergen induced airway inflammation and hyperresponsiveness. Thorax 2006: 61: 134–9.
- 50Debarry J, Garn H, Hanuszkiewicz A, et al. Acinetobacter lwoffii and Lactococcus lactis strains isolated from farm cowsheds possess strong allergy-protective properties. J Allergy Clin Immunol 2007: 119: 1514–21.
- 51Debarry J, Hanuszkiewicz A, Stein K, et al. The allergy-protective properties of Acinetobacter lwoffii F78 are imparted by its lipopolysaccharide. Allergy 2010: 65: 690–7.
- 52Hagner S, Harb H, Zhao M, et al. Farm-derived Gram-positive bacterium Staphylococcus sciuri W620 prevents asthma phenotype in HDM- and OVA-exposed mice. Allergy 2013: 68: 322–9.
- 53Harb H, van Tol EAF, Heine H, et al. Neonatal supplementation of processed supernatant from Lactobacillus rhamnosus GG improves allergic airway inflammation in mice later in life. Clin Exp Allergy 2013: 43: 353–64.
- 54Brand S, Teich R, Dicke T, et al. Epigenetic regulation in murine offspring as a novel mechanism for transmaternal asthma protection induced by microbes. J Allergy Clin Immunol 2011: 128: 618–25 e1–7. doi:10.1016/j.jaci.2011.04.035.
- 55Schaub B, Liu J, Höppler S, et al. Maternal farm exposure modulates neonatal immune mechanisms through regulatory T cells. J Allergy Clin Immunol 2009: 123: 774–82.e5
- 56Gollwitzer ES, Saglani S, Trompette A, et al. Lung microbiota promotes tolerance to allergens in neonates via PD-L1. Nat Med 2014: 20: 642–7.
- 57Geuking MB, Cahenzli J, Lawson MAE, et al. Intestinal bacterial colonization induces mutualistic regulatory T cell responses. Immunity 2011: 34: 794–806.
- 58Curotto de Lafaille MA, Lafaille JJ. Natural and adaptive foxp3+ regulatory T cells: more of the same or a division of labor? Immunity 2009: 30: 626–35.
- 59Olszak T, An D, Zeissig S, et al. Microbial exposure during early life has persistent effects on natural killer T cell function. Science 2012: 336: 489–93.
- 60Cahenzli J, Köller Y, Wyss M, et al. Intestinal microbial diversity during early-life colonization shapes long-term IgE levels. Cell Host Microbe 2013: 14: 559–70.
- 61Loss G, Bitter S, Wohlgensinger J, et al. Prenatal and early-life exposures alter expression of innate immunity genes: the PASTURE cohort study. J Allergy Clin Immunol 2012: 130: 523.e9–30.e9.
- 62Lauener RP, Birchler T, Adamski J, et al. Expression of CD14 and Toll-like receptor 2 in farmers' and non-farmers' children. Lancet 2002: 360: 465–6.
- 63Lluis A, Depner M, Gaugler B, et al. Increased regulatory T-cell numbers are associated with farm milk exposure and lower atopic sensitization and asthma in childhood. J Allergy Clin Immunol 2014: 133: 551–9.
- 64Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 2013: 504: 446–50.
- 65Trompette A, Gollwitzer ES, Yadava K, et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med 2014: 20: 159–66.
- 66McLoughlin RM, Mills KHG. Influence of gastrointestinal commensal bacteria on the immune responses that mediate allergy and asthma. J Allergy Clin Immunol 2011: 127: 1097–107.
- 67Joerink M, Oortveld MAW, Stenius F, et al. Lifestyle and parental allergen sensitization are reflected in the intrauterine environment at gene expression level. Allergy 2010: 65: 1282–9.
- 68Ege MJ, Herzum I, Büchele G, et al. Prenatal exposure to a farm environment modifies atopic sensitization at birth. J Allergy Clin Immunol 2008: 122: 407–12. doi:10.1016/j.jaci.2008.06.011
- 69Pfefferle PI, Büchele G, Blümer N, et al. Cord blood cytokines are modulated by maternal farming activities and consumption of farm dairy products during pregnancy: the PASTURE Study. J Allergy Clin Immunol 2010: 125: 108–15.e1–3.
- 70Braun-Fahrländer C, Von Mutius E. Can farm milk consumption prevent allergic diseases? Clin Exp Allergy 2011: 41: 29–35.
- 71Pfefferle PI, Prescott SL, Kopp M. Microbial influence on tolerance and opportunities for intervention with prebiotics/probiotics and bacterial lysates. J Allergy Clin Immunol 2013: 131: 1453–63.
- 72Azad MB, Coneys JG, Kozyrskyj AL, et al. Probiotic supplementation during pregnancy or infancy for the prevention of asthma and wheeze: systematic review and meta-analysis. BMJ 2013: 347: f6471.
- 73Calder PC, Kremmyda L-S, Vlachava M, et al. Is there a role for fatty acids in early life programming of the immune system? Proc Nutr Soc 2010: 69: 373–80.
- 74Hollams EM, Hart PH, Holt BJ, et al. Vitamin D and atopy and asthma phenotypes in children: a longitudinal cohort study. Eur Respir J 2011: 38: 1320–7.
- 75Boerner BP, Sarvetnick NE. Type 1 diabetes: role of intestinal microbiome in humans and mice. Ann N Y Acad Sci 2011: 1243: 103–18.