Predictors and management of post-banding ulcer bleeding in cirrhosis: A systematic review and meta-analysis
Handling Editor: Dr. Alessio Aghemo
Abstract
Background and Aims
Post-banding ulcer bleeding (PBUB) is an understudied complication of oesophageal varices endoscopic band ligation (EBL). This systematic review with meta-analysis aimed at: (a) evaluating the incidence of PBUB in patients with cirrhosis treated with EBL in primary or secondary prophylaxis or urgent treatment for acute variceal bleeding and (b) identifying predictors of PBUB.
Methods
We conducted a systematic review of articles in English published in 2006–2022 using the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. Searches were made in eight databases including Embase, PubMed and Cochrane Library. Random-effects meta-analysis was used to determine the incidence, mean interval and predictors of PBUB.
Results
Eighteen studies (9034 patients) were included. The incidence of PBUB was 5.5% (95% CI 4.3–7.1). The mean time for it to occur was 11 days (95% CI 9.94–11.97). Model for End-stage Liver Disease (MELD) score (OR 1.162, 95% CI 1.047–1.291) and EBL done in emergency setting (OR 4.902, 95% CI 2.99–8.05) independently predicted post-ligation ulcer bleeding. Treatment included drugs, endoscopic procedures and transjugular intrahepatic portosystemic shunt. Refractory bleeding was treated with self-expandable metallic stents or balloon tamponade. Mortality was on average 22.3% (95% CI 14.1–33.6).
Conclusions
Patients with high MELD score and receiving EBL in an emergency setting are more prone to develop PBUB. Prognosis is still poor and the best therapeutic strategy to address remains to be ascertained.
Abbreviations
-
- APRI Score
-
- Alanine aminotransferase to Platelet Ratio Index
-
- APTT
-
- activated partial thromboplastin time
-
- CI
-
- 95% confidence interval
-
- CMA
-
- comprehensive meta-analysis
-
- EBL
-
- oesophageal varices endoscopic band ligation
-
- GEV
-
- gastroesophageal varices
-
- HCC
-
- hepatocellular carcinoma
-
- HVPG
-
- hepatic venous pressure gradient
-
- INR
-
- international normalized ratio
-
- MELD Score
-
- Model for End-stage Liver Disease
-
- MBN and MK
-
- Maria de Brito Nunes and Mathias Knecht
-
- NOS
-
- Newcastle-Ottawa Scale
-
- NSBB
-
- non-selective beta-blockers
-
- OR
-
- odds ratio
-
- p
-
- p-value
-
- PBU
-
- post-banding ulcers
-
- PBUB
-
- post-banding ulcer bleeding
-
- PICO
-
- Population, Interventions, Comparisons, Outcomes
-
- PPI
-
- proton pump inhibitors
-
- PRISMA
-
- Preferred Reporting Items for Systematic Reviews and Meta-analyses
-
- PT
-
- prothrombin time
-
- ROB 2 Tool
-
- Cochrane's risk of bias
-
- SD
-
- standard deviation
-
- SEMS
-
- oesophageal self-expandable metallic stent
-
- TIPS
-
- transjugular intrahepatic portosystemic shunt
-
- VET
-
- viscoelastic tests of coagulation
-
- VH
-
- variceal haemorrhage
Key points
- MELD score and emergency EBL are the strongest predictors of post-banding ulcer bleeding (PBUB) in cirrhosis.
- The pooled post-PBUB mortality in the studies included was 22.3%.
- The strategies to prevent PBUB and the best treatment approach need to be prospectively investigated.
1 INTRODUCTION
Cirrhosis is the fifth leading cause of adult deaths worldwide. Portal hypertension (increased pressure gradient between the portal vein and the inferior vena cava) is the main complication of cirrhosis and leads to the formation of porto-systemic collaterals, including gastroesophageal varices (GEV) that are present in over 50% of patients with cirrhosis at diagnosis.1 GEV increase in size over time, and can rupture, leading to gastrointestinal haemorrhage. Variceal haemorrhage (VH) constitutes a major decompensating event in cirrhosis, and despite the advances in its treatment, it is still associated with significant mortality (15%–20% at 6 weeks).1-3
Oesophageal varices endoscopic band ligation (EBL) is an endoscopic procedure aimed at eradicating varices by ligating them with rubber rings (bands). According to current international guidelines, EBL of oesophageal varices plays an important therapeutic role in three settings: (a) the prevention of a first VH as an alternative to non-selective beta-blockers (NSBB) in patients with contraindications or who cannot tolerate these drugs1, 4; (b) to achieve haemostasis in combination with vasoactive drugs (somatostatin, octreotide or terlipressin) in patients with acute VH; and (c) to prevent recurrent bleeding. In the latter case patients are treated both with NSBB and EBL. EBL is considered safe, but is not free of complications like chest pain, dysphagia, fever, and development of post-banding ulcers (PBU) that may lead to bleeding (PBUB).5 After banding, when the ligation bands drop off, a superficial ulcer is formed that may bleed, which can be difficult to distinguish from VH due to portal hypertension. In these patients, bleeding is likely triggered by the EBL-induced ulcer that may damage the underlying mucosal vessels or varices.5, 6 PBUB induce significant mortality and morbidity in cirrhosis.5, 7, 8
The aims of this systematic review were to summarize the existing data regarding the incidence of PBUB, and to identify predictors of PBUB in patients with cirrhosis. Additionally, we described the current strategies used to manage bleeding after PBUB.
2 METHODS
2.1 Protocol and registration
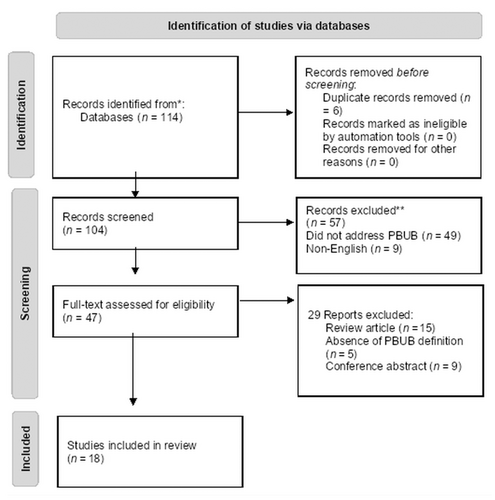
The review follows the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) recommendations.9 Ethical approval was not sought because of the study design. The PROSPERO registered protocol number is CRD42022353449.
2.2 Search strategy, inclusion and exclusion criteria
Electronic databases were searched using text words related to PBUB in google Scholar, Medline (OVID interface), Embase (OVID interface), PubMed, Cochrane Library, Cochrane Central Register of Controlled Trials (CENTRAL), clinicaltrials.gov, EU clinical Trials, and citations for studies published between 2006 and May 25, 2022. Indeed, in 2006 with Baveno IV recommendations,10 EBL replaced variceal injection sclerotherapy for the prevention and treatment of bleeding oesophageal varices. The search strategy is detailed in Table S1.
Randomized controlled trials, cohort studies, case control, cross sectional studies and case series studies in English language, satisfying the following inclusion criteria were included: studies published between 2006 and May 2022. Only peer-reviewed articles were accepted; PICO (Population, Interventions, Comparisons, Outcomes): a population of patients with cirrhosis (aged 18 years old or more) and portal hypertension undergoing EBL either as urgent treatment, primary or secondary prophylaxis of variceal bleeding; indicator or intervention: EBL interventions for primary prophylaxis, secondary prophylaxis or acute variceal bleeding, reporting on PBUB incidence, risk factors, management and outcomes. Outcomes: incidence of PBUB, predictive factors of PBUB, management and treatments for PBUB, mortality.
PBUB had to be clearly defined and considered the origin of the upper gastrointestinal bleeding after EBL, if one ulcer or more are observed at the ligation site, with or without bleeding, and without another apparent source of bleeding.
Case reports and review articles were excluded. Two reviewers (MBN and MK) independently screened abstracts and selected full text articles for inclusion. The discrepancies were solved by the senior authors.
2.3 Data extraction and quality assessment
From the eligible articles the reviewers extracted the following information: study characteristics (author, year, recruitment period, sample size); demographic characteristics of the population (age, sex); clinical characteristics of the population (cirrhosis aetiology, Child–Pugh score and MELD score); EBL and PBUB characteristics (setting of endoscopy, incidence of PBUB, interval ligation and risks factors for PBUB, management, follow-up duration and mortality associated with PBUB).
Quality assessment of the observational studies was performed using the Newcastle-Ottawa Scale (NOS) (Tables S2 and S3). Studies were classified in high quality if ≥7 points, moderate quality if 5–6 points and low quality if ≤4 points. Thirteen studies were classified into high quality,4, 5, 7, 8, 11-18 four studies were at moderate risk of Bias.19-22 Cochrane's ROB 2 Risk of Bias Tool was used to assess the risk of bias in two randomized controlled trials (Table S4). These two included studies were at low risk of Bias.23, 24
2.4 Statistical analysis
Meta-analysis was performed to determine the incidence of PBUB in cirrhotic patients, overall and comparing urgent EBL treatment setting versus primary and secondary prophylaxis (elective EBL). The software Comprehensive meta-analysis (CMA), version 3 was used. The odds ratio (OR) with 95% confidence interval (CI) is the measure of association used in this meta-analysis for the risk's factors of PBUB. Rates with 95% confidence interval were used for the incidence and mortality associated with PBUB.
We selected a random-effects model because of the differences between the studies (different population and setting of endoscopies). For the assessment of heterogeneity, clinical heterogeneity such as characteristics of population, losses to follow-up, outcomes and different management/treatments were considered. Statistical heterogeneity was tested using the I2 test. A I2 ≥ 50% or p < .1 was suggestive of considerable heterogeneity among the studies. Publication bias was measured using Egger's regression.
3 RESULTS
3.1 Selection process and characteristics of the studies
Eighteen studies were included in the systematic review (Figure 1) of which 14 were retrospective observational studies,5, 7, 8, 11-19, 21, 22 four studies were prospective, with two prospective observational studies4, 20 and two randomized controlled trials.23, 24 The main study characteristics are provided in Table S5. The indication for EBL was elective (primary and/or secondary prophylaxis) in three studies,12, 21, 23 urgent treatment of active variceal bleeding in one study,22 and both elective prophylaxis and urgent treatment of acute variceal bleeding in 14 studies.4, 5, 7, 8, 11, 13-20, 22, 24 Sixteen included studies were unicentric and two were multicentric studies.12, 14 Overall, these studies included a total of 9043 patients, 6819 (75.4%) male and 2224 (24.6%) female. The aetiology of cirrhosis was variable, the more common being alcoholic liver disease, with 2612 cases (28.9% of the patients), and viral chronic liver disease in 2001 (22%) patients. The severity of cirrhosis was graded by the Child–Pugh score in 16 studies,4, 5, 7, 12-14, 16, 18-20, 22-24 3414 (44%) patients being in Child–Pugh class A, 2832 (37%) were Child–Pugh B and 1420 (19%) patients were Child–Pugh C.
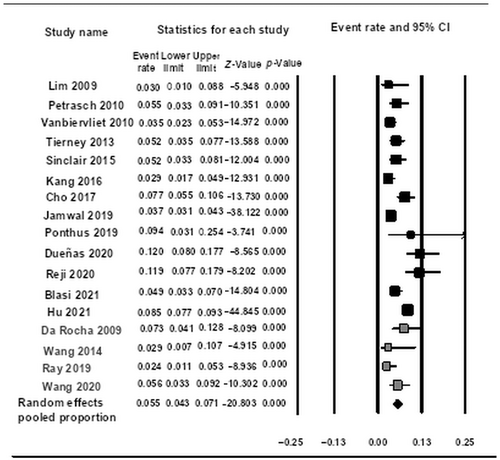
3.2 Incidence of post-banding ulcer bleeding
The pooled incidence of PBUB in patients with cirrhosis was reported in 17 studies (Figure 2). Overall, incidence of PBUB was 5.5% (95% CI 4.3–7.1) with significant heterogeneity (I2 = 87.6%, p < .01). The incidence of PBUB was slightly higher in the retrospective studies (5.8%, 95% CI 4.3–7.7, p < .001), compared with prospective studies (4.7%, 95% CI 2.8–7.6, p < .001), but the incidence rate difference of 1.1% is not statistically significant (p < .001). When analysed independently, no considerable statistical heterogeneity is identified in prospective studies (I2 = 48.2%, p < .001; Figures S1 and S2).
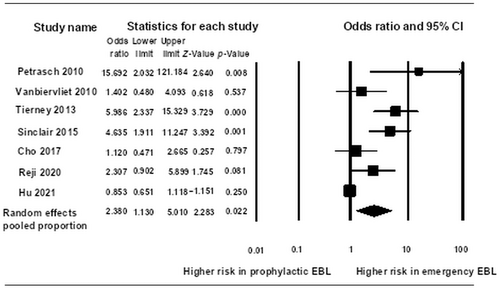
3.2.1 Incidence of post-banding ulcer bleeding with endoscopic band ligation in urgent treatment setting versus endoscopic band ligation in primary and secondary prophylaxis
In a subgroup analysis of seven studies (Figure 3), a total of 7527 patients with 515 bleeders from PBUBs, PBUB was more frequent in those having urgent EBL (OR 2.360, 95% CI 1.130–5.010, p < .001) compared with the primary and secondary prophylactic group ligation, with significant heterogeneity (I2 87.6%, p < .01). The pooled incidence rate of PBUB among patients treated with urgent EBL was 8.3% (95% CI 6.4–10.7), with considerable heterogeneity (I2 56%, p < .001). The pooled incidence rate of PBUB in the group with prophylactic EBL was 3.9% (95% CI 1.8–8.4), with important heterogeneity (I2 92%, p < .001). There is a significant difference of 4.5% between the two groups (p < .0001). One study13 was the exception presenting a higher incidence of PBUB after prophylactic EBL compared with urgent EBL. This difference might also be related to the differences in sample size and in the characteristics of the population, since in this study patients treated with prophylactic EBL had a higher MELD score (mean MELD score 18.6 ± 5.1) compared with the other studies only with prophylactic EBL treatment, that present a mean MELD score below 14.4, 13, 21, 23 One study5 was not included due to the lack of data about the number of patients undergoing to EBL in the elective versus urgent situations.
3.3 Mean interval of post-banding ulcer bleeding occurrence
The pooled random effect describes a value for the time PBUB's occurrence in six studies of 11 days (95% CI 9.9–12) without heterogeneity (I2 .000, p < .001) (Figure S3). The rest of studies do not give mean and standard deviation (SD) values and thus could not be incorporated into the meta-analysis.
3.4 Predictors of post-banding ulcer bleeding
Fifteen studies assessed the predictors of PBUs using multivariate analysis. These disclosed a wide range of predicting factors: higher MELD score (six studies),5, 8, 12, 14-16 emergency ligation for acute variceal bleeding (four studies),8, 11, 16, 24 ulcers with high-risk stigmata on endoscopy (three studies),13, 14, 18 Child–Pugh score C (three studies)4, 16, 20 or high APRI score (one study),7 previous variceal bleeding (one study),7 peptic oesophagitis (two studies),7, 8 lack of administration of proton pump inhibitors (PPI) (one study),21 concomitant gastric varices (two studies),15, 21 high risk varices on endoscopy (one study),16 higher number of bands (two studies),11, 13 low propanonol dose (two studies),5, 24 presence of hepatocellular carcinoma (HCC; one study)5 and low haemoglobin level (one study).18 Even though most studies assessed the coagulation parameters and platelets as potential predictors of PBUB, only one study7 identified an impairment on coagulation (low prothrombin index) as an independent predictor of PBUB. Articles showing a high Child–Pugh score as predictor of PBUB did not provide enough data to perform a meta-analysis (Table S6).
3.4.1 High model for end-stage liver disease score
A higher MELD score was a predictor of PBUB in six studies (Figure S4), with a pooled random effect odds ratio (OR) of 1.162 (95% CI 1.047–1.291, p < .001). There was significant heterogeneity (I2 67.752; with p = .015). The mean MELD score of patients with PBUB was 18 or more in three studies.5, 8, 14 Two studies had an inferior MELD score of 1312 and 1015 in the group of patients with PBUB, but higher than the non-bleeding group in these studies. One study16 was not included in this meta-analysis due to lack of sufficient data.
3.4.2 Urgent endoscopic band ligation
Urgent EBL was associated with PBUB in four studies (Figure S5) with a pooled OR of 4.902 (95% CI 2.986–8.047, p < .001). There was no statistical heterogeneity (I2 .000, p < .001).
3.4.3 Independent predictors of post-banding ulcer bleedings in the analysed studies
Model for End-stage Liver Disease score (OR 1.162, 95% CI 1.047–1.291) and EBL carried out in emergency setting (OR 4.902, 95% CI 2.986–8.047) independently predicted post-ligation ulcer bleeding.
3.4.4 Ulcers with high-risk stigmata on endoscopy
Three studies13, 14, 18 identified the endoscopic aspect of ulcers with high-risk stigmata (red wale sign, cherry spot, white nipple sign, platelet plug) as a predictor of PBUB. However, the pooled OR describes no significant effect of this factor on PBUB (OR 3.872, 95%, CI .794–18.881, p < .001). The studies showed a considerable heterogeneity (I2 80.466; p = .06) (Figure S6).
3.5 Management of post-banding ulcer bleeding
Due to the considerable heterogeneity of included studies, a statistical analysis of the treatment of PBUB was not possible. Data were extracted and are described into the Table S7.
PPI, sucralfate and antibiotics were used as prophylactic treatment in most studies.
Considering the treatment in case of acute PBUB, most studies used the vasoactive drug therapy used for variceal bleeding (somatostatin, octreotide or terlipressin) as well as intravenous PPI. More variability exists across the studies regarding the endoscopic type of treatment applied, with Re-EBL being used to treat PBUB in eight studies.5, 12, 14-16, 19, 23, 24 Other types of endoscopic therapies were used as well (argon plasma coagulation, oesophageal variceal obliteration, like sclerotherapy and cyanoacrylate injection, epinephrine injection, hemoclip). In case of refractory bleeding, oesophageal self-expandable metallic stent (SEMS) was employed in two studies,14, 22 and oesophageal balloon tamponade in six studies.5, 7, 14, 15, 21, 22 TIPS was used in severe bleeding in five studies5, 7, 14, 16, 24 but the number of patients treated were reported only in three studies: one study7 reported two patients receiving an emergency TIPS; in the second study,16 TIPS was used successfully as initial treatment in two patients, and as a rescue treatment in four patients, and was successful in 3; in the third study14 TIPS was performed in 19 patients, of whom 9 survived and 8 died despite TIPS. In one study,14 two patients were transplanted.
3.6 Mortality rate associated with post-banding ulcer bleeding
Fourteen studies reported the mortality associated with PBUB. The pooled mortality reported was 22.3% (95% CI 14.1–33.6), with a significant statistical heterogeneity (I2 81.280, p < .01) (Figure 4).

4 DISCUSSION
Development of PBUB in cirrhosis remains an important complication of EBL and a clinical challenge. The purpose of this systematic review with meta-analysis was to summarize the existing data regarding the incidence of this complication in elective and emergency settings, to describe the identified predictors of PBUB in cirrhosis, and secondarily to recapitulate the strategies used in the management of this complication. We have systematically analysed the literature on PBUB since 2006, when the Baveno IV conference10 recommended using EBL rather than sclerotherapy in the prevention and treatment of bleeding oesophageal varices.
The present systematic review and meta-analysis indicates a pooled incidence of PBUB among the 9043 patients with cirrhosis included of 5.5%. Furthermore, the data showed that patients treated in an emergency setting have a much higher incidence of PBUB compared with patients treated in an elective setting.
The analysis of the literature denotes that MELD score (severity of the liver disease), and emergency EBL are the stronger predictors of PBUB in cirrhosis. These factors suggest that the severity of liver failure plays an important role, but that circumstances associated with the emergency setting (difficulty in placing correctly the bands due to poor visualization during active bleeding, lack of expert assistance, greater number of bands used), comorbidities as infections, or excessive fluid replacement may favour recurrence.
Most of the studies used a multivariable analysis to adjust for potential confounders. However, factors such as bacterial infection, presence of HCC, peptic oesophagitis, concomitant gastric varices, ulcers with high-risk stigmata on endoscopy, high grade varices on endoscopy, higher number of bands, low beta-blocker dose, coagulation impairment, among others, were not clear predictors of PBUB on multivariate analysis. This may be due to low number of events in many series, limiting this type of analysis, which would require an individual patient data meta-analysis to draw robust conclusions. Since PBUBs share features with variceal bleeding, other factors that have not addressed in the studies so far, but potentially add prognostic information are hepatic venous pressure gradient (HVPG), and portal-vein thrombosis increasing portal pressure.
The pooled post-PBUB mortality in the 14 studies included in our systematic review was 22.3%, a very high figure, which is even higher than the mortality from variceal bleeding in recent series. Although it is conceivable that not only the incidence of PBUB, but also the mortality was higher in emergency setting, this could not be inferred from this systematic review, as most studies did not provide separate mortality data in emergency versus elective EBL complicated by PBUB. In the study by Sinclair et al. (2015),8 which reported the mortality in elective versus emergency procedures, mortality due to PBUB was higher in the emergency setting. Five deaths following PBUB were reported: one after primary prophylaxis, one post-secondary prophylaxis and three after band ligation in the setting of acute variceal bleeding.
Regardless of the high mortality, there is no standard-of-care treatment for PBUB. The current treatment remains empirical and based on the expertise of the individual centres. Despite there was no signal pointing at any influence of reflux esophagitis on PBUB, a prophylactic treatment with PPI was administered in the majority of the included studies. The literature describe that PPI may diminish the size of PBUs, but in most studies PPI had no effect on bleeding complications or in mortality.5, 18, 25-28 Only one study29 reported a better outcome of EBL with long-term PPIs administration. On the other hand, a judicious use of these drugs is needed due to their known adverse effects in patients with cirrhosis (pneumonia, hepatic encephalopathy, spontaneous bacterial peritonitis, osteoporosis).26, 30, 31 The recent BAVENO VII consensus, recommends that whenever PPIs are started before endoscopy, these should be discontinued if endoscopy does not show a clear indication.32 Similarly, other study7 used sucralfate as prophylaxis for PBUB, without a reduction in the risk of bleeding.
Whether antibiotic prophylaxis was used in the context of PBUB was not explicit in all included studies. Bacterial infections are an important complication in acute variceal bleeding. It remains a risk factor for rebleeding and bleeding control, especially in patients with cirrhosis Child–Pugh B and C.33, 34 When prophylaxis was introduced spontaneous bacterial peritonitis and bacteremia by enteric Gram-negative bacteria were frequent infections.35 Nowadays, respiratory infections accounts for 50% of all cases of infection, in patients with acute variceal bleeding, under antibiotic prophylaxis.34, 36 International guidelines recommend antibiotic prophylaxis on admission to hospital, in cirrhotic patients with acute variceal bleeding because it reduces the risk of infection, improves control of bleeding, reduces rebleeding and mortality.32, 37 Whether the same should be applied to patients with PBUB, remains to be confirmed in future studies.
Medical therapy and different endoscopic procedures similar to those used for acute variceal bleeding were used to treat PBUB. TIPS was used in some studies in patients with severe bleeding.7, 14, 16 Tierney et al. suggest considering an early TIPS in patients with massive haemorrhage secondary to PBUB. Nonetheless, in this study16 patients treated with TIPS presented the highest rate of mortality, which is likely due to a more severe liver disease (higher proportion of patients with Child–Pugh C) or to a delayed decision for TIPS. It is likely that as it happens in spontaneous variceal bleeding in high-risk patients,38 also in high-risk patients with PBUB the early use of TIPS could be associated with lower failure and mortality rates, but this should be investigated in adequate studies. Moreover, our data cannot support an evidence-based recommendation on which specific intervention should be chosen to manage PBUB after the acute haemorrhage is controlled (TIPS or continuing with NSBB and EBL), and the most appropriate therapy still needs to be assessed by specifically designed studies.
As rescue therapy oesophageal SEMS14, 22 or oesophageal balloon tamponade5, 7, 14, 15, 21, 22 were employed in the included studies. Balloon tamponade or SEMS are recommended as a bridge therapy to a more definite treatment in case of refractory variceal bleeding. SEMS are as efficacious and much safer than balloon tamponade.32 The stent can be maintained for up to 1 week (and in some cases has been used for 2 weeks) until a definitive treatment.39 In a retrospective analysis22 included in this systematic review its efficacy in controlling the bleeding in patients with PBUB was of 82%.
The above-mentioned strategies are much the same used for variceal bleeding, implying that the authors have assumed that the mechanism of PBUB is similar to that of VH. The only specific treatment addressing a different possibility has been the use of PPI, but these have not been shown to be universally effective.25, 27, 31 A possibility that deserves further study is whether defects in haemostasis related to the liver disease (low platelet counts, unbalanced coagulation status),4, 40, 41 to concomitant complications (specially infections) or to the circumstances of the treatment (specially in emergency cases with EBL done out of working hours by not expert endoscopists) can be optimized to improve this dismal prognosis.
The coagulation impairment was evaluated on most studies with classic coagulation tests such as prothrombin time (PT), international normalized ratio (INR) and activated partial thromboplastin time (APTT). They were not predictive of PBUB, but it is well known that standard coagulation tests have significant limitations in cirrhosis. In this disease, there is simultaneously a relative deficiency and excess of pro- and anticoagulant components leading to a very fragile balance of haemostasis.42, 43 Other tools for assessment of the haemostasis in cirrhosis like viscoelastic tests of coagulation (VET) are underexplored. These dynamic tests are not routinely used in chronic liver disease outside the transplant setting, but there is evidence that they are more accurate in identifying cirrhotic patients who are at risk of bleeding or thrombosis.44 Five randomized controlled trials studied the use of VET to guide blood product transfusion in cirrhosis prior to invasive procedures, in patients with non-variceal haemorrhage, in patients with variceal bleeding, and in the context of liver transplantation showing a significant reduction in overall blood products transfusion.45-50 Whether VET might be used as predictors of PBUB is a field for future prospective studies. With respect to the management of patients with acute variceal bleeding, the Baveno VII recommendations32 suggest a transient discontinuation of anticoagulation whenever possible until bleeding control is achieved. On the other hand, anticoagulant therapy discontinuation is not recommended in the setting of elective band ligation, or in patients with portal hypertension from extrahepatic portal vein obstruction. Whether anticoagulation or coagulation impair in general might have an impact on the risk of PBUB is not known and should be object of future studies.
A limitation of this systematic review is that most data come from retrospective observational studies, which carry a high risk of bias. This is illustrated by the fact that the incidence of PBUB was higher in retrospective that in prospective studies, but the difference was mild (5.8% in retrospective series vs. 4.7% in prospective series). Many other studies on rebleeding post-EBL could not be included since the incidence of PBUB and different causes of rebleeding were not specified. Clearly, a better knowledge of predicting factors, and specifically the issue of whether haemostatic defects contribute to PBUB, require further study.
In addition, the best treatment approach needs to be investigated in multicentric prospective studies. These should probably stratify patients presenting with PBUB according to the severity of the bleeding and severity of liver failure to define the best treatment approach for each subgroup.
In conclusion, this systematic review analysed data from 18 studies and 9034 patients with cirrhosis and portal hypertension treated with EBL in elective or in an emergency setting. We found that patients with a higher MELD score, or treated with emergency EBL for acute variceal bleeding are more prone to suffer from PBUB. PBUB carries a high mortality despite the variety of treatments used, which calls for prospective, specifically designed studies to improve outcomes of this severe iatrogenic complication.
AUTHOR CONTRIBUTIONS
MBN: data collection, statistical analysis of the data and drafting the manuscript; MK: data collection and manuscript revision; RW: manuscript revision; JB: statistical analysis of the data and manuscript revision, critical revision of the manuscript for important intellectual content AB: study conception, supervision of the study, manuscript revision for important intellectual content. All authors have commented on the manuscript and approved the final version.
ACKNOWLEDGEMENTS
The authors are grateful to Prof. Daniel Hayoz and Prof. Daniel Betticher, Hospital of Fribourg and the Burgergemeinde Bern, for the kind support. Open access funding provided by Inselspital Universitatsspital Bern.
FUNDING INFORMATION
Maria de Brito Nunes receives financial support from a grant from the Hospital of Fribourg, Switzerland and from the Burgergemeinde Bern.
CONFLICT OF INTEREST STATEMENT
The authors do not have any disclosures to report.
ETHICS STATEMENT
Ethical approval was not necessary because of the study design.
PROSPERO REGISTRATION NUMBER
The PROSPERO registered protocol number is CRD42022353449.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.